What is Hemorrhage?
Hemorrhage is sudden blood loss from an injured blood vessel. This bleeding could be minor, like when small blood vessels near the surface of your skin are injured, causing small, round spots on the skin (petechiae) or larger patches of bruising (ecchymosis). However, the bleeding could also be significant, leading to various symptoms like changes in vital signs such as pulse and blood pressure, and even changes in mental status. A hemorrhage can happen either outside or inside the body.
External bleeding is evident when it comes from an open wound or a body opening, like the mouth or nose. On the other hand, internal bleeding isn’t immediately visible and requires careful examination by doctors. They have to take a detailed medical history, conduct physical exams, order lab tests, use imaging like X-rays, and closely watch vital signs to diagnose it. Hemorrhage is a principal cause of avoidable death, particularly in people who have recently suffered from trauma.
What Causes Hemorrhage?
When you lose blood, the symptoms you experience can depend on where in your body you’re bleeding from. This is known as hemorrhage. For example, after a serious injury, you might bleed from a cut on your skin, from inside your skull, chest, or belly, or even from a broken bone. The first step to finding out where you’re bleeding from and why is to do a thorough medical examination.
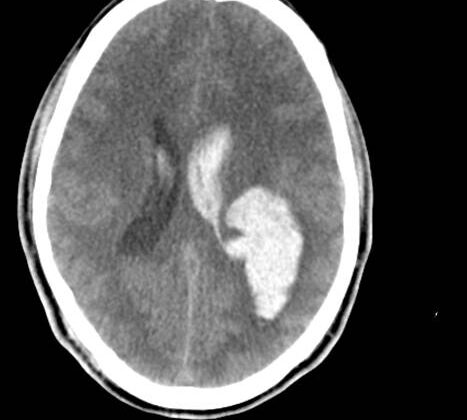
If you’re bleeding within your brain, this is because a blood vessel has burst and started bleeding around or into your brain. Depending on where this happens, your symptoms might differ. This could include weakness on one side of your body, headaches, nausea, vomiting, and confusion. Often, this kind of bleeding can happen if you have high blood pressure for a long time, which can weaken the walls of your arteries. Other causes can be excessive alcohol drinking, prolonged smoking, old age, and substance abuse. Injuries to the head can also cause this type of bleeding.
There is another kind of bleeding in the brain called subarachnoid hemorrhage. This is when blood gathers between tissues that cover the brain, irritating the tissues lining the brain, leading to intense pain. Most people who experience this describe having a sudden severe headache as if it is “the worst headache of their life.” This can be caused by a ruptured aneurysm. However, a traumatic head injury, as well as abnormal connections between blood vessels, can also lead to this form of hemorrhage. Other types of bleeding in the brain can be found inside the brain tissue, or as a collection of blood underneath the skull but outside the brain after a head injury.
In the chest, bleeding is known as hemothorax. This is when the blood starts to pool between the inner lining of your chest wall and the outer surface of your lung. This blocks your lung from fully expanding and makes it hard to breathe. This type of bleeding usually occurs due to injuries, spread of cancer, blood clotting issues, or sometimes it can start without any known reason. When this happens, you may feel dizzy, short of breath, and experience chest pain. Without treatment, this can lead to shock or death. If the blood in the chest builds to high pressure and affects the blood flow back to the heart, this can also be a life-threatening emergency.
Loss of blood in the belly after trauma is harder to detect. The symptoms, such as stomach pain, blood in vomit, blood in urine, passing black stool, or bruising, may not be specific and might need imaging tests to diagnose. A severe case can result in shock and death. Things that can cause bleeding in the belly include damage to organs like the liver, spleen, or kidneys, issues with blood vessels, complications from certain procedures in gyneacology/obstetrics, or blood clotting disorders. Common causes in women who could become pregnant include a pregnancy outside of the womb or the rupture of a cyst.
Bleeding can also occur in a space behind the abdominal area, which contains vital organs and blood vessels. Injuries to this area can be due to trauma to the belly or pelvic area. Depending on the area, the bleeding can result in different symptoms like pain in the belly, back or side of the waist, symptoms involving urine if the bladder is pressed, and weakness of the thigh. A telltale sign can be a bruise on your side.
Long bone fractures, such as the arm and leg bones, can cause serious, life-threatening bleeding. The middle part of these bones is filled with bone marrow, which makes red blood cells and has many arteries. Some bones, like the thigh bone, can hold a large amount of blood, making hemorrhage a serious risk either due to an injury or during surgery.
Risk Factors and Frequency for Hemorrhage
In people under the age of 46 living in America, the main cause of death is bleeding due to injury. The reasons for this bleeding can vary and are often influenced by a person’s lifestyle and economic situation. In the year 2000, the World Health Organization estimated that 9% of all global deaths were caused by injuries. Moreover, injuries amounted to 12% of all health problems worldwide. Interestingly, about 90% of these injuries happen in countries with low to middle income. Both traffic accidents and violent incidents have been linked to high rates of lethal bleeding.
Signs and Symptoms of Hemorrhage
If you’ve been injured, the first step healthcare providers take is to get your history and run physical exams. This helps them figure out where any potential bleeding might be coming from. They usually use a two-step examination method. It includes checking your blood circulation, which is a critical step in the initial survey. During this step, they also try to manage heavy bleeding if there is any. There are five key areas they check to identify life-threatening bleedings: externally (on the skin), in the chest, in the stomach, behind the abdominal area, in the pelvic area, and the thighs.
Patients who are at risk of bleeding should tell their healthcare provider if they are taking any blood-thinning medications, if they have a bleeding disorder, or if they’ve recently had a trauma or medical procedures. In cases of bleeding in the digestive tract, figuring out the source can be tricky without additional tests. However, a detailed history and thorough physical exam can provide clues.
In case of bleeding in the brain, a thorough review of history and a physical exam can give a hint to the healthcare provider about its possible cause. Still, imaging tests are usually needed for confirmation.
Bleeding that occurs without an apparent injury is usually marked by a fast heartbeat, low blood pressure, passing of bloody or black stools, vomiting blood, coughing up blood or blood in the urine.
Testing for Hemorrhage
If your doctor suspects that you have a bleed in your brain, they will likely order certain tests. These might include a CT scan (a type of X-ray that gives detailed pictures of the brain) within six hours of when your symptoms started for the best possible treatment results. If more than six hours have passed, an MRI (a test that uses magnetic fields and radio waves to capture images) might be more effective. A test called a lumbar puncture (sometimes referred to as a spinal tap) might also be helpful as it can detect red blood cells or a change in colour of the fluid surrounding your spinal cord and brain, indicating bleeding.
For a suspected bleed in your chest, the doctor might order a chest X-ray, ultrasound, or a CT scan, depending on what’s available and how stable your condition is. If your condition is unstable, you wouldn’t be moved to a different area for these tests, instead, they would be done at your bedside. This way, the healthcare team can diagnose a large collection of blood, or hemothorax, in the chest without moving you into an unstable situation. Plus, a fluid analysis (a lab test that checks for blood in other forms of fluid) can confirm the diagnosis. To treat a chest bleed, a tube may be placed in your chest to remove excess fluid, and surgery may be performed if the bleeding can’t be controlled otherwise.
In cases of suspected bleeding in your abdomen that’s causing a drop in blood pressure or shock, either a CT scan or a trauma ultrasound, referred to as a focused assessment with sonography for trauma (FAST Scan), may be performed. The FAST scan is a quick and non-invasive test that can, for example, identify an abdominal aortic aneurysm (a swollen area in your body’s main blood vessel) in someone experiencing worrying symptoms. You might need surgery if you show signs of abdominal bleeding; these signs include changes in your abdominal area, worsening condition, instability in your blood pressure and heart rate, and a positive FAST scan result. But if your blood pressure is stable and there’s no immediate threat to your life, doctors may choose less invasive methods of imaging before resorting to surgery. If the bleed is suspected to be in the area towards the back of your abdomen (known as the retroperitoneal area), an ultrasound and a CT scan may be done.
Finally, if you are experiencing bleeding from a body opening, such as your airway or urinary tract, a type of test called an endoscopy might be performed. This involves inserting a tube with a light and camera into orifices like your bronchus for bronchoscopy, bladder for cystoscopy, colon for colonoscopy or upper digestive tract for an esophagogastroduodenoscopy (EGD) to check for any bleeding.
Treatment Options for Hemorrhage
If a person is bleeding severely, how it’s managed can depend on several factors. These can include where the injury is located, how bad it is, the person’s overall health, and what treatment options are available. If the patient is showing signs of low blood volume, or hypovolemia, they will need to be resuscitated with fluids given through an IV.
Resuscitation involves inserting large IV lines and introducing fluids like normal saline or lactated ringer into the body. It also involves starting a transfusion protocol, which means giving the patient blood products like red blood cells, fresh frozen plasma, and platelets. These are given in equal amounts and as needed. It’s important to monitor the patient for hypothermia, which can occur when receiving transfusions.
The goal of this treatment is to increase blood volume and maintain the delivery of oxygen until the bleeding can be stopped. Healthcare providers aim for a certain amount of pressure in the arteries (known as mean arterial pressure or MAP), which is usually above 65 mm Hg. If the injury is from a sharp object, the goal is to have a systolic blood pressure (the pressure when the heart beats) above 90 mm Hg. For brain injuries, the target MAP is 105 mm Hg or higher, and the goal systolic blood pressure is above 120 mm Hg.
It’s also crucial to monitor lactic acid levels and signs of worsening metabolic acidosis (a buildup of acid in the body), as these can lead to a loss of constriction in the blood vessels of the extremities and collapse of the cardiovascular system. For wounds that are external and caused by trauma, applying direct pressure and using tourniquets (devices that tightly squeeze the area) above the bleeding area can be life-saving.
What else can Hemorrhage be?
Spotting a bleed quickly needs a keen doctor. A detailed health history and physical exam can raise suspicions and call for quick intervention. Some types of bleeding may lead to a condition called hypovolemic shock, caused by severe blood loss. It’s important to distinguish this from other causes of shock. Different types of bleeding, like those in the brain, can quickly lead to serious symptoms as there’s little space for extra blood to gather before pressure increases, leading to changes in consciousness and other brain functions. Other conditions to consider include:
- Migraine headaches
- Meningitis or encephalitis (infections of the brain and its lining)
- Brain tumors
- Electrolyte abnormalities (abnormal levels of minerals in the body)
- Stroke
- Heart attack
- Intoxication or poisoning
What to expect with Hemorrhage
The outcome of a traumatic wound that leads to excessive bleeding (hemorrhagic shock) largely relies on early detection and prompt medical action. Without prompt treatment, these wounds can have a high risk of death. The doctor’s job is to ensure that adequate oxygen is getting to your body, control the bleeding, and prevent tissue from getting too little oxygen, which can cause damage.
Possible Complications When Diagnosed with Hemorrhage
Bleeding complications can arise due to reduced blood flow to body organs, leading to oxygen deprivation in the tissues, otherwise known as tissue hypoxia. This lack of oxygen can trigger organ failure, seizures, and even result in a coma or death. In particular, if the brain lacks oxygen for an extended period, it can cause tissue infarction, which often results in long-term neurological and cognitive problems.
A specific type of bleeding known as subarachnoid hemorrhage can cause the blood vessels to constrict several weeks after a bleed, leading to a stroke. Other generalized complications include bleeding again and problems related to staying in the hospital, like deep vein thrombosis (clotting in the veins) and infection.
Here are the complications in a simpler form:
- Tissue hypoxia (oxygen deprivation in tissues)
- Organ failure
- Seizures
- Coma
- Potential Death
- Tissue infarction (tissue death due to lack of blood flow) in the brain
- Long-term neurological and cognitive problems
- Stroke triggered by a subarachnoid hemorrhage
- Bleeding again
- Deep vein thrombosis (blood clot)
- Infections
Preventing Hemorrhage
After experiencing a hemorrhage, or a heavy loss of blood, it’s crucial for patients to understand what their recovery may look like and how they can work to prevent it from happening again. Research has shown that those who survive a hemorrhage often struggle to meet their targets for recovery, mainly due to a lack of available resources. So, before leaving the hospital, it’s essential for patients to talk with their healthcare team about what they hope to achieve in terms of recovery, and where they can turn to for help as they heal.
Not only patients, but their family members too, should be well-versed about the recovery process. This helps everyone involved understand what to expect. Also, granting access to social and financial help can greatly help in dealing with the pressures that may come about as a result of the condition.