What is Acute Promyelocytic Leukemia?
Acute promyelocytic leukemia is a specific type of acute myeloid leukemia, identified by a particular gene combination called PML-RAR-alpha. Patients with this condition often have a high chance of being cured with treatment. It was first observed in 1957 in patients who experienced severe bleeding due to a process called fibrinolysis, rapid worsening of their health, and an increased presence of a cell type called promyelocytes in their blood and bone marrow.
Breakthroughs in understanding the molecular makeup of this leukemia have led to the development of new treatments, arsenic trioxide and all-trans retinoic acid. These therapies have improved the survival outlook for patients.
What Causes Acute Promyelocytic Leukemia?
The RAR-alpha gene, which plays a part in hormone regulation, is located on chromosome 17 and is linked to a condition called Acute Promyelocytic Leukemia (APL). This gene activates various other genes when it binds to a molecule called retinoic acid.
In approximately 90% to 95% of APL cases, the condition stems from a specific rearrangement of chromosomes 15 and 17. This rearrangement creates a fusion of the promyelocytic leukemia gene with RAR-alpha, creating two combined genes which produce a malfunctioning protein, causing an abnormal response to retinoid.
There are also some other less common chromosome rearrangements in APL. For instance, genes in chromosomes 5, 11, 17 can get fused with the RAR-alpha gene. These changes result in the creation of hybrid proteins. Some can respond to retinoid-based treatment, while others show limited to no response.
However, it is still unclear why these chromosome rearrangements happen or why they precipitate leukemia. Some known risk factors are exposure to chemotherapy, ionizing radiation, industrial solvents, and other toxic substances.
Risk Factors and Frequency for Acute Promyelocytic Leukemia
Acute promyelocytic leukemia, a relatively rare leukemia, makes up around 7% to 8% of adult acute myeloid leukemia (AML) cases. This type of leukemia mostly affects middle-aged individuals with an average age of 47. It’s rare to see cases in individuals younger than 20. A slight majority of the cases occur in males.
- Acute promyelocytic leukemia is a relatively rare type, encompassing around 7% to 8% of adult AML cases.
- It is typically seen in middle-aged people, with an average age of 47.
- This type of leukemia is very rare in people below the age of 20.
- There are slightly more cases in males than in females.
Signs and Symptoms of Acute Promyelocytic Leukemia
Patients with this condition often feel generally weak and tired. They may have bleeding gums, small red or purple spots on the skin (petechiae or ecchymoses), changes in vision due to bleeding in the retina, nosebleeds, heavy periods, or infections. They may also experience blood clot-related issues like deep vein thrombosis, blockage of the lung’s main artery (pulmonary embolism), or stroke. In some advanced cases, patients may suffer from severe blood clotting that can cause serious bleeding.
A reduction of all types of blood cells (pancytopenia) is usually noticed when patients first seek medical help. One major difference between Acute Promyelocytic Leukemia (APL) and Acute Myeloid Leukemia (AML) is that many patients with APL run the risk of developing severe clotting and associated high-fibrinolysis, a condition where the body’s usual process of breaking down clots is exaggerated. This is a urgent medical condition that needs immediate attention to prevent bleeding in the brain and lungs.
- General weakness and fatigue
- Bleeding gums
- Red or purple spots on the skin (petechiae or ecchymoses)
- Vision changes due to retinal bleeding
- Nosebleeds
- Heavy periods or infections
- Blood clots, such as deep vein thrombosis, pulmonary embolism or stroke
- The risk of severe blood clotting leading to serious bleeding in advanced cases
- Reduction of all types of blood cells (pancytopenia) at first medical visit
- Higher risk of severe clotting and high-fibrinolysis in APL compared to AML
Testing for Acute Promyelocytic Leukemia
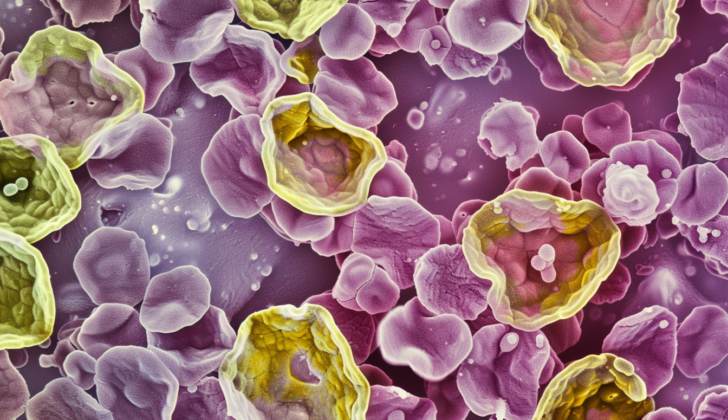
If doctors think someone may have acute promyelocytic leukemia (a type of blood cancer), they need to test their blood as soon as possible. They analyze their blood under a microscope and use a method called FISH to check for specific genes that are indicative of this disease.
It’s also important they run other tests to figure out how well the person’s blood is clotting. This means checking the number of platelets (cells that help your blood clot), the prothrombin time (how long it takes for your blood to clot), the activated partial thromboplastin time (another measure of how long it takes your blood to clot), the d-dimer or fibrin split products (substances in your blood that can indicate a blood clot), and the fibrinogen (another protein that is needed for blood to clot).
To get a better understanding of the disease, they may also take a small sample of bone marrow (the spongy tissue inside your bones) and examine it under a microscope. Another test checks the person’s chromosomes (structures in cells that contain genes) for any unusual patterns.
Not all cases of acute promyelocytic leukemia are the same, and doctors classify the disease into low-risk, intermediate, or high-risk categories based on the number of white blood cells and platelets in the person’s blood. This helps them decide what treatment will be best.
If the person has a high-risk form of the disease and a large number of white blood cells, doctors might need to get a sample of spinal fluid to decide on the best treatment. Before beginning certain types of treatment, they would need to make sure the person’s heart is working well.
Treatment Options for Acute Promyelocytic Leukemia
Acute promyelocytic leukemia is a severe and life-threatening disease that requires immediate treatment. A key component of treatment for this type of leukemia is a drug called All-Trans Retinoic Acid (ATRA), which is used in all modern treatment plans. In fact, it is so important that it is given to patients even before their disease is genetically confirmed.
Before ATRA was introduced in the 1980s, treating this form of leukemia was very challenging, and survival rates were low when relying on chemotherapy alone. However, the combination of ATRA with anthracycline-based treatments significantly improved survival and cure rates.
Another agent, called arsenic trioxide (ATO), also plays an important role in treating leukemia. It acts by altering the behavior of the problematic cells, and it is known to work well in combination with ATRA. In fact, studies have shown that combining ATRA and ATO is even less toxic than combining ATRA and chemotherapy. Therefore, ATRA-ATO has become the new standard of care for patients with low to intermediate risk leukemia.
There are variations in treatments for patients with high-risk disease or other severe health conditions. For example, ATRA combined with Idarubicin or ATRA combined with ATO and an antibody-drug conjugate called gemtuzumab ozogamicin are preferred for high-risk patients who do not have heart problems. The latter combination can also be used for those with serious health conditions, older adults, and patients with heart issues who can’t tolerate harsh treatments.
There is ongoing debate about the necessity of ongoing ‘maintenance’ therapy after the initial treatment phase. It might not be necessary for patients who have received intensive initial treatment that includes ATO.
Alongside the treatment of leukemia itself, supportive treatment also plays a crucial role in patient survival. This includes maintaining an adequate blood platelet count and preventing or managing systemic infections, given that leukemia patients are often immunocompromised. This means that patients with a fever need immediate antibiotics and potential antifungal treatment if the fever continues. When it comes to severe, unidentified infections, vancomycin should be considered.
Bone marrow transplantation is not typically the first offered treatment because cure rates for this type of leukemia are high with the treatments mentioned above. It is only considered for patients whose disease is resistant to other therapies or who have relapsed. Another treatment called intrathecal therapy, where drugs are injected into the space around the spinal cord, is used for high-risk patients.
What else can Acute Promyelocytic Leukemia be?
If you hear medical terms like ‘Acute Lymphoblastic Leukemia’ or ‘Acute Myeloid Leukemia’, these are types of blood cancer where the body produces too many white blood cells. ‘Aplastic anemia’ is another blood disorder where the body stops making enough new blood cells. Moving on to ‘Folic acid deficiency’, this is when your body lacks enough of the B-vitamin folic acid, which can lead to various health issues. Finally, ‘Myelodysplastic syndrome’ refers to a group of disorder where the body’s bone marrow doesn’t produce enough healthy blood cells.
What to expect with Acute Promyelocytic Leukemia
Without treatment, Acute Promyelocytic Leukemia (APL) has an extremely poor prognosis, with a typical survival period of about a month. However, modern treatments have significantly improved survival rates, with most patients achieving a full recovery and staying in remission. In a study by Lo-coco, nearly all the patients treated with a combination of ATRA (a form of therapy) and arsenic trioxide remained disease-free after two years. Even with a combination of ATRA and chemotherapy, nine out of ten patients stayed illness-free within the same period.
Without treatment, the disease is fatal, usually due to infection and a condition called hemorrhagic differentiation syndrome. The White Blood Cell (WBC) count serves as a crucial indicator of how the disease will progress. A higher count is usually associated with greater risk. Other factors influencing the prognosis include older age, male gender, elevated creatinine levels in the blood (a sign of kidney problems), and high fibrinogen levels (a protein that helps in blood clotting).
Possible Complications When Diagnosed with Acute Promyelocytic Leukemia
Differentiation Syndrome is a medical condition that often starts after the initiation of treatment agents designed to enhance cell differentiation. This syndrome is marked by a number of symptoms like fever, swelling in the peripheral parts of body, fluid accumulation in lungs, and dysfunction of multiple organs. If not identified and treated quickly, it could lead to fatal outcomes. High doses of systemic steroids are generally used as a treatment method for these cases.
Another condition, known as Hyper Leukocytosis, can occur as a side-effect of differentiation agents. This happens due to the rapid change of immature promyelocytes, which are types of cells in the blood. For severe cases of Hyper Leukocytosis, systemic steroids and chemotherapy are used as treatments.
Preventing Acute Promyelocytic Leukemia
Doctors often recommend a diet that’s low in bacteria, known as a neutropenic diet, for certain patients. This means fresh fruits or flowers, which can harbor bacteria, shouldn’t be in the person’s room.
Moreover, medical staff will keep a close eye on patients for a decrease in platelets – a condition called thrombocytopenia. This condition could potentially lead to spontaneous bleeding, so it’s critical to monitor it closely.