post-contrast T1 Vibe images are submitted. A delayed enhancing hilar mass
biopsy has proven to be cholangiocarcinoma. This mass has an increased T2 signal
in comparison to the background liver parenchyma.
What is Cholangiocarcinoma (Bile Duct Cancer)?
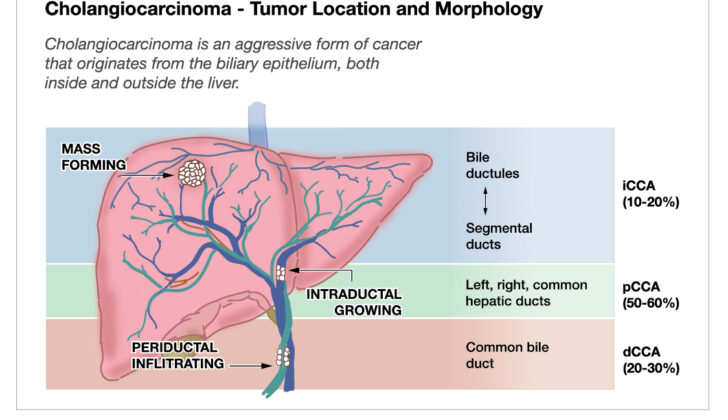
Cholangiocarcinoma is a severe form of cancer that originates from the cells lining the bile ducts in your liver. This cancer can occur in any part of the bile ducts, from those inside the liver to the end where the main bile duct enters the first section of the small intestine. This cancer is divided into two types based on where it starts: within the liver (intrahepatic cholangiocarcinoma) or outside the liver (extrahepatic cholangiocarcinoma). The outside liver type is then further divided into perihilar and distal cholangiocarcinoma. Over 95% of these cancers are known as adenocarcinomas.
Certain conditions and early-stage lesions can increase the risk of developing cholangiocarcinoma. The symptoms can vary depending on the tumor’s size and location. Diagnosing this cancer can be challenging, especially for tumors outside the liver, as existing testing methods may not always detect them. Surgery may be needed, even if the diagnosis isn’t confirmed, based on the individual’s health condition. It’s important for anyone suspected or diagnosed with cholangiocarcinoma to be checked for any spread of the cancer as about 75% of patients have cancer that cannot be surgically removed or has spread at the time of diagnosis.
A substance called Carbohydrate Antigen 19-9 (CA 19-9), which is produced by the cells lining the bile ducts, can help evaluate the severity of the condition and monitor its changes. Sadly, because this cancer is aggressive and is often diagnosed in advanced stages, the overall outlook is generally poor. Surgery is the only treatment that can potentially cure this disease, with radiation and chemotherapy being used as supplementary treatments. New therapies targeting specific aspects of this cancer are being discovered, improving patient outcomes and offering hope for better patient care in the future.
What Causes Cholangiocarcinoma (Bile Duct Cancer)?
Cholangiocarcinoma, which is a type of cancer in the bile duct, often emerges without clear causes or genetic links. However, certain risk factors can make some people more likely to develop this cancer, and these vary according to ethnicity and geographical location.
One such factor is parasitic infections. Consuming undercooked fish can result in invasion by liver flukes like Clonorchis and Opisthorchiasis. This problem is especially common in Southeast Asian regions, particularly northeastern Thailand. These parasites cause long-term inflammation in the bile ducts, which can lead to cholangiocarcinoma.
Another risk factor is auto-immune disease called primary sclerosing cholangitis. This disease constantly damages the liver and bile duct, and people with it have up to 400 times higher chance to develop cholangiocarcinoma compared to the general population. This risk is even higher if someone with the disease also has inflammatory bowel disease.
Presence of stones in the bile duct, including gallstones and others, also increases cholangiocarcinoma risk. This is especially true when the stones are larger and/or the illness lasts longer. This condition is more common in Asia and often occurs in tandem with parasitic infections.
Additionally, patients with certain types of cysts in the bile duct are more likely to develop this cancer. This includes people with choledochal cysts, biliary mucinous cystic neoplasms, and intraductal papillary biliary mucinous neoplasms. Young women are more likely to suffer from biliary mucinous cystic neoplasms, which can cause pain or other symptoms when they grow large. Similarly, intraductal papillary biliary mucinous neoplasms often contain cancer and are usually removed with surgery.
Chronic liver disease can also increase the risk of cholangiocarcinoma. This includes long-term hepatitis B or C infection, conditions causing too much iron in the liver (hemochromatosis), metabolic dysfunction-associated fatty liver disease, and any cause of cirrhosis or severe liver damage.
Lastly, lifestyle, environmental, and metabolic factors like type 2 diabetes, obesity, alcohol consumption, and cigarette smoking can increase the risk of cholangiocarcinoma. Exposure to certain hazardous substances like Thorotrast (a radioactive contrast media used in the past), asbestos, and propylene dichloride also increases this risk.
Having certain genetic conditions can make people more susceptible to cholangiocarcinoma development. This includes hereditary nonpolyposis colorectal cancer (also known as Lynch syndrome), BAP1-related tumor predisposition syndrome, multiple biliary papillomatosis, and cystic fibrosis.

Risk Factors and Frequency for Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinomas, a type of gastrointestinal cancer, makes up about 3% of all such cancers. They are the second most common type of primary liver tumors and represent 10% to 15% of all cancers in the liver and bile ducts. The number of intrahepatic cholangiocarcinomas has been increasing, likely due to better detection and identification methods, while the number of extrahepatic tumors has been decreasing. Cholangiocarcinoma rates are significantly higher in certain areas, like Thailand, compared to the United States, sometimes by up to 50 times.
The likelihood of developing cholangiocarcinoma increases as people age. It is slightly more common in men than in women, and it is most often diagnosed in people between 50 and 70 years of age.
- Perihilar cholangiocarcinoma is the most common subtype, accounting for about 50% of all cases.
- Distal cholangiocarcinoma accounts for 40% of cases.
- Intrahepatic cholangiocarcinoma is the least common, making up only 10% of cases.

and 20s, 3-minute, and 10-minute post-contrast T1 Vibe images are submitted.
There is a delayed-enhancing mass in segment 7 of the right hepatic lobe, which
biopsy has proven to be cholangiocarcinoma. This mass has increased T2 signal in
comparison to the background liver parenchyma.
Signs and Symptoms of Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinoma is a type of cancer that affects the bile ducts inside or outside the liver. The symptoms of this disease differ depending on the size and location of the tumor. People with a tumor inside the liver may experience symptoms such as nonspecific abdominal discomfort, unexplained weight loss, and extreme tiredness. Additionally, jaundice, a condition that causes yellowing of the skin and eyes, and inflammation of the bile duct, can occur if the tumor blocks the bile flow. Unfortunately, these symptoms often arise late in the disease, meaning the tumors might be large when diagnosed.
On the other hand, tumors outside of the liver are usually detected earlier due to bile duct blockage, which can cause symptoms such as jaundice, itching, pale stools, and dark urine. In advanced cases, patients may notice a palpable lump in the abdomen and a buildup of fluid, called ascites. Some patients may not show any symptoms related to the cancer until it has spread to other areas of the body; these are often discovered accidentally during imaging tests.
A physical examination of a patient suspected to have cholangiocarcinoma involves checking the patient’s nutritional status and liver function, as well as a detailed check of the abdomen. In rare instances, a tumor may be felt during the abdominal exam in the upper right area of the abdomen, a sign that the cancer has grown and possibly caused a blockage in the bile duct. If fluid accumulation in the abdomen or symptoms of high blood pressure in the liver’s blood vessels are observed, it may indicate that the disease isn’t likely to be treatable with surgery.
Testing for Cholangiocarcinoma (Bile Duct Cancer)
If someone shows symptoms that suggest they might have cholangiocarcinoma, a type of cancer affecting the bile ducts, doctors will carry out a range of tests to try and identify what’s wrong. These tests may include taking a sample of tissue from the affected area, but obtaining this sample can be challenging depending on the location of the suspected tumor. The tests we have for this are unfortunately not sensitive enough to conclusively rule out cholangiocarcinoma.
When it comes to laboratory testing, patients are likely to have a complete blood count taken, along with a comprehensive metabolic profile which checks liver function and looks at coagulation (clotting). These tests may reveal signs like anemia (low red blood cell count), abnormalities in liver function, signs of liver disease like biliary obstruction and more. We might also look for elevated enzymes that suggest damage to the liver cells. Some tumors can cause an increase in direct bilirubin and alkaline phosphatase levels, which are common in biliary obstruction cases. We also check levels of certain tumor markers (proteins produced by cancer), but some of these can be unreliable if biliary obstruction is present.
Patients will likely also have imaging tests. These can include abdominal ultrasound, which is a simple, non-invasive, cost-effective and radiation-free way to look for signs like liver mass or distension (swelling or enlargement) of the gall bladder. If this doesn’t provide a clear diagnosis, a computerized tomography (CT) scan may be done. This scan can also identify the liver anatomy and look for localized or spread disease. A chest CT is needed to check for potential spread of the disease.
Another option for imaging is a magnetic resonance imaging (MRI) scan, which can give a more detailed picture of the liver. When combined with a type of imaging that looks at the pancreatic and bile ducts (MR cholangiopancreatography, or MRCP), it can help doctors identify strictures (narrow sections), masses, and cysts more effectively. Yet another imaging tool is positron emission tomography (PET), often used to see if the disease has spread to other parts of the body. However, it’s not typically recommended for routine use when managing cholangiocarcinoma.
In addition to these imaging tests, doctors may use endoscopic techniques, such as endoscopic retrograde cholangiopancreatography (ERCP) to diagnose the disease. This is a procedure used to relieve obstruction in the bile ducts and to attempt to diagnose the disease. However, even with the help of these techniques, the chance of effectively ruling out cancer remains low. Sometimes, due to the limitations of these techniques, doctors may decide to operate even without a definite tissue diagnosis. Other techniques like Endoscopic Ultrasound (EUS) and Percutaneous Transhepatic Cholangiography (PTC) are also used to evaluate and manage the condition. However, the correct diagnosis and treatment of cholangiocarcinoma is challenging and requires a comprehensive approach.
Treatment Options for Cholangiocarcinoma (Bile Duct Cancer)
Managing cholangiocarcinoma, a type of cancer that forms in the bile ducts, is a complex process. The main purpose is to decide based on the location and spread of cancer and its impact on surrounding structures. The only definite cure is surgery, which involves either removing the part affected by cancer or transplanting the liver. Chemotherapy and radiation are used in combination with surgery as additional treatment methods.
Before Surgery:
Sometimes, cholangiocarcinoma can block the bile ducts leading to liver problems. In such cases, doctors often consider draining the bile before surgery. This is done using a procedure known as ERCP and helps prevent liver damage. However, it is debated whether bile drainage benefits all patients, as it can sometimes increase post-surgical complications. Most doctors recommend it for patients undergoing pre-surgery chemotherapy.
Knowing the volume of the liver and the part that can function properly after surgery is critical in planning the operation. If the functional part of the liver is not large enough for the patient’s health, doctors use techniques like Portal Venous Embolization, which involves blocking the blood supply to the affected part of the liver leading to growth in healthier portions.
Local Therapies:
If surgery isn’t an option due to the tumor’s size or the patient’s health condition, local therapies are used to manage the cancer. These methods can slow down the spread of cancer in the liver, improving survival rates and quality of life.
Transarterial Chemoembolization involves direct injection of chemotherapy drugs into the liver’s blood supply, followed by blocking the blood supply to starve the tumor. Transarterial Radioembolization is a similar but newer technique where radioactive materials are inserted into the tumor to expose it to high radiation dosage.
With Tumor Ablation, heat energy is applied directly to the tumor to destroy it. This can be repeated as needed.
Hepatic Artery Infusion involves surgically installing a pump that delivers chemotherapy drugs directly into the liver artery. This technique can significantly shrink the tumor, but it is not widely used because it requires a surgical procedure.
In conclusion, managing cholangiocarcinoma involves a mix of surgery, chemotherapy, radiation, and local therapies, each of which has its benefits and drawbacks. Depending on the patient’s condition and the tumor’s characteristics, doctors decide on the most effective approach.
What else can Cholangiocarcinoma (Bile Duct Cancer) be?
Cholangiocarcinoma, a type of cancer, can be tough to detect due to its generic symptoms such as yellowing of the skin and eyes (jaundice), abdominal discomfort, and exhaustion (fatigue). As a result, it can be mistaken for many other health conditions. Some of these similar health issues include:
- Choledocholithiasis (gallstones in the bile duct)
- Pancreatic cancer
- Primary sclerosing cholangitis (a liver disease that damages the bile ducts)
- Primary biliary cirrhosis (a slow damage to the liver’s bile ducts)
- Hepatocellular carcinoma (another type of liver cancer)
- Cholangitis (an infection in the bile duct)
- Cholecystitis (an inflammation of the gallbladder)
Surgical Treatment of Cholangiocarcinoma (Bile Duct Cancer)
The same basic rules that apply to liver surgery are also important to consider when dealing with a liver condition known as cholangiocarcinoma. It is essential to ensure a patient has a sufficient part of the liver unaffected by the cancer, as well as clear and normal blood flow in and out of the liver. It’s also crucial to ensure that no cancer cells remain during surgery. A technique called a ‘diagnostic laparoscopy’ should be carried out first, as some patients who seem fine on scans actually have cancer spread that can’t be seen. Up to 30% of patients could be in this situation.
Intrahepatic Cholangiocarcinoma is a type of liver cancer and the main treatment is removing as much of the tumor as possible through surgery. The long-term outlook is better if no traces of the tumor are left behind. Surgery extent can depend on where the tumor is and its size. If the tumor impacts the portal vein (a big blood vessel near the liver), this might also need work. It’s also key to examine the lymph nodes, small glands that filter the body’s fluids, in the surrounding area.
Deciding on a treatment for a different type of cancer, Perihilar Cholangiocarcinoma, can be difficult because assessing how far the cancer has spread might not always be clear. Despite high-quality scanning and endoscope techniques, the full extent of the tumor might not be obvious until during the operation. Usually, doctors will remove the part of the bile duct that the tumor affects and the part of the liver closest to the tumor, including lymph nodes nearby for examination. Doctors usually follow a system called the Bismuth-Corlette classification to determine the surgery approach. This system categorizes the tumor based on its location in the liver and helps guide surgical treatment.
For example, Types I and II tumors often involve the removal of the affected bile duct and parts of the liver near it. In some cases, a more significant part of the liver might also need removal. Type III tumors usually require removal of the affected bile duct and either the right or left part of the liver based on where the tumor is. Type IV tumors typically require a liver transplant. Pre-operative chemotherapy followed by a liver transplant has been shown to provide a survival rate of over 50% after 5 years.
For a different kind of tumor called ‘Distal Cholangiocarcinoma’, surgery involves removing parts of the pancreas and bile duct. This type of surgery is called a ‘pancreaticoduodenectomy’. To ensure there’s no part of the tumor left, it might be necessary to remove a large part of the bile duct. Occasionally, if the tumor is in the mid-duct, the tumor can be removed without any other surgery.
What to expect with Cholangiocarcinoma (Bile Duct Cancer)
The outlook for cholangiocarcinoma, a type of cancer, is generally not good. At the time of diagnosis, only about a quarter of patients have a condition that can be treated with surgery. This is especially true for tumors located within the liver and near the liver’s hilum, as they are often in a more advanced stage.
The 5-year survival rate, which is the percentage of people who live at least five years after being diagnosed, is around 8% for intrahepatic (inside the liver) cholangiocarcinoma. For extrahepatic (outside the liver) cholangiocarcinoma, the rate is slightly better but still low, at approximately 10%.
Despite the risks involved, surgery provides the best chance for a cure. However, it’s important to note that surgical procedures can often be quite challenging and may lead to serious complications.
Possible Complications When Diagnosed with Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinoma, a type of liver cancer, can lead to various complications. These problems can either be as a result of the disease itself or due to the treatments patients go through. One of the severe problems faced by patients with advanced cholangiocarcinoma includes the spreading of the disease within the liver, which can lead to liver failure. This type of cancer can also create mass-like structures that can block the bile ducts, causing several health issues such as infection of the bile duct (cholangitis), shrinking of the liver (atrophy), scar tissue in the liver (cirrhosis), and significant physical weakness (deconditioning). The disease can also spread to distant parts of the body, or spread within the abdominal cavity.
Here are the complications in a simplified list format:
- Intrahepatic metastases leading to liver failure
- Biliary obstruction causing:
- Cholangitis (bile duct infection)
- Liver atrophy (shrinking of the liver)
- Cirrhosis (scar tissue in the liver)
- Deconditioning (significant physical weakness)
- Spread of the disease to distant parts of the body
- Local spread of the disease within the abdominal cavity
Preventing Cholangiocarcinoma (Bile Duct Cancer)
Cholangiocarcinoma, a rare yet aggressive cancer, affects the bile ducts in the body. Symptoms can often be unclear, especially when the cancer starts in the liver, and can include general issues like stomach pain, weight loss, and tiredness. Another type of this cancer can occur outside the liver and may cause jaundice (a yellowing of the skin or eyes) or stomach pain.
It’s important to seek medical advice if you have any risk factors for cholangiocarcinoma, like long-term parasitic infections, a disease involving cysts in the bile ducts, or symptoms such as unexplained weight loss, decreased appetite, excessive tiredness, or any unusual yellowing of the skin or urine.
Diagnosing cholangiocarcinoma can be challenging. It often requires several different scanning techniques or hands-on procedures. Yet, notably, about a quarter of people diagnosed with cholangiocarcinoma can be fully cured.