What is Glioblastoma Multiforme?
Glioblastoma multiforme (GBM) is the most dangerous and widespread type of glioma, a kind of brain tumor. It’s essentially the most common primary brain tumor in adults, making up 45.2% all the primary malignant brain and central nervous system (CNS) tumors.
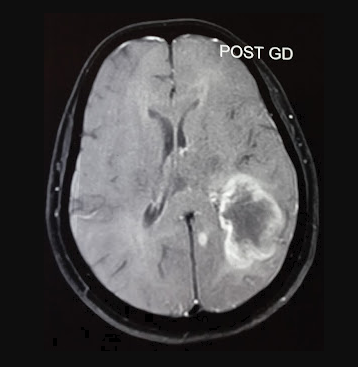
Magnetic Resonance Imaging (MRI), a form of medical imaging using strong magnetic fields and radio waves, shows some defining characteristics. These include unclear margins, a lighter center, and a darker outer area. The lighter center (seen in a T1 scan) is due to damaged tissue death, while the darker edges (seen in a T2/FLAIR scan) indicate swelling. An MR spectroscopy, another type of MRI scan used to measure biochemical changes in the brain, shows a peak of a substance called choline.
The disease is definitively diagnosed through microscopic examination of tissue, which shows irregular cells with a pattern indicating astrocytoma, a specific type of brain cancer originating in certain star-shaped brain cells called astrocytes. Rapid cell division, increased blood vessels, and tissue death are all defining characteristics of GBM. The tumor also tests positive for certain proteins (GFAP, vimentin, and S100) and shows varied indices of Ki-67, a marker of cell proliferation. Additionally, testing is recommended to determine the status of genetic changes.
Unfortunately, GBM is currently incurable with a life expectancy of around 15 months. Only about 5.5% of patients live past 5 years after being diagnosed. GBM has been classified into two variants: one with a mutation in the isocitrate dehydrogenase (IDH) gene and one without. The former bears a specific epigenetic mark known as G-CIMP.
The variant without the IDH mutation, which makes up almost 90% of all GBM, usually develops spontaneously and is found in people older than 55. Histologically, they can be further divided into giant cell, gliosarcoma, and epithelioid cell subtypes. These tend to have mutations in particular genes, EGFR, TERT, and MGMT. The IDH-mutant variants usually develop from a precursor tumor and tend to affect younger patients. They are associated with ATRX and TP53 mutations, and tend to have longer survival rates.
What Causes Glioblastoma Multiforme?
The main factor known to cause Glioblastoma (GBM), a type of brain cancer, is exposure to high doses of ionizing radiation. This is a type of energy released by atoms that can cause damage to cells and lead to cancer. A research study found a large number of people (about 17%) who had this type of brain cancer had been exposed to therapeutic radiation treatments in their past. The time between this radiation exposure and the development of GBM can range from a few years to many decades.
Interestingly, research has shown that there is a lower risk of developing gliomas (a category of brain and spinal cord tumors that includes GBM) in people with allergies and atopic diseases. An atopic disease is a type of allergic reaction that usually appears early in life, some examples include hay fever, eczema, and asthma. Furthermore, using anti-inflammatory medications for less than 10 years might have a short-term protective effect against GBM.
There isn’t substantial evidence linking GBM with lifestyle habits like smoking, drinking alcohol, using drugs, or exposure to N-nitroso compounds, which are chemicals that could potentially contribute to cancer formation.
As of now, research has not found that using mobile phones increases the risk for GBM. However, the potential risk associated with long-term use of mobile phones is still being investigated and clarified.
Risk Factors and Frequency for Glioblastoma Multiforme
Glioblastoma, often abbreviated as GBM, is the most common type of malignant brain tumor. It makes up 15% of all primary brain tumors and half of all malignant brain tumors. GBM affects roughly 35 out of a million people each year, with men being slightly more affected than women at a ratio of 1.6:1. According to 2013 data from the Central Brain Tumor Registry of the United States, the average rate of GBM is about 3.19 out of every 100,000 people. However, in the pediatric population, this rate is significantly lower at 0.85 per 100,000.
GBM is mainly diagnosed in adults and is most common in those around 64 years old. The number of cases tends to increase as individuals age, peaking between 75 and 84 years old, then declining after 85 years old. In people aged 65 and older, the rate of GBM increases to 130 per million individuals. With the population in the United States aging, the number of GBM cases is expected to rise. Currently, GBM accounts for nearly half of the 24,000 new cases of primary malignant brain tumors reported each year in the United States.
Signs and Symptoms of Glioblastoma Multiforme
Glioblastoma multiforme (GBM) is a type of brain tumor, with symptoms and signs that primarily depend on the tumor’s size and location. The symptoms are pretty much like any benign or malignant brain tumor. GBM usually shows a steady increase in neurological symptoms over a few days or weeks. Because these symptoms are not unique and could also point to an infection or other disease, doctors need to stay vigilant about the possibility of GBM.
The GBM tumor can occur in different parts of the brain, with different frequencies:
- Supratentorial (main upper part of the brain) – happens in 85% of cases, and almost 25% of these are in the frontal lobe.
- Brainstem – found in less than 5% of cases.
- Spinal cord – found in less than 5% of cases.
- Cerebellum (lower part of the brain) – happens in less than 3% of cases.
Different GBM patients may show different signs and symptoms:
- Intracranial hypertension (increased pressure within the skull) – seen in 30% of cases.
- Motor deficit (problems with movement) – happens in 20% of cases.
- Epilepsy – seen in 20% of cases.
- Altered sensorium (changes in perception or awareness) – seen in 17% of cases.
- Confusion – found in 15% of cases.
- Visual deficit (problems with vision) – happens in 13% of cases.
- Speech deficit (problems with speech) – seen in 13% of cases.
Testing for Glioblastoma Multiforme
The MRI scan of the brain may show some unclear outlines and changes in the blood-brain barrier, which is the protective layer that keeps harmful substances away from the brain. The images may reveal a specific pattern linked to a type of brain tumor called Glioblastoma Multiforme. Also, there can be areas in the brain that appear to have lowered activity (due to tissue death) and other areas that may show increased activity (due to swelling).
Another specialized brain scan, called Perfusion-weighted imaging (PWI), may show increased blood flow in the brain. This can happen because of new blood vessel formation and changes to the blood-brain barrier. Alongside, MR Spectroscopy (a kind of test that provides information about the biochemical makeup of a disease or condition) may show a spike in a compound called choline, which usually increases when the cells rapidly multiply.
Despite what the MRI and these specialized scans may show, the gold standard for making an official diagnosis is to perform a biopsy and examine the tissue under a microscope.
Doctors may also suggest testing for presence of certain specific proteins like GFAP and mutations in certain genes like IDH and O6-methylguanine-DNA methyltransferase (MGMT). These tests provide additional information that can help in managing the condition.
Treatment Options for Glioblastoma Multiforme
The treatment for glioblastoma multiforme (GBM), a type of brain cancer, typically involves a team of healthcare professionals: surgical oncologists (cancer doctors who specialize in surgery), medical oncologists (cancer doctors who focus on medicine) and radiation oncologists (cancer doctors specializing in radiation therapy). The ideal treatment starts with surgery to remove as much of the tumor as possible, followed by radiation and chemotherapy to kill any cancer cells left behind.
The goal of surgery is to remove cancer cells (a process known as cytoreduction), confirm the diagnosis through microscopic examination of the removed tissue, determine the unique genetic characteristics of the tumor, and possibly use medication-filled implants.
Greater amount of tumor removed during surgery is usually related to better outcomes. Research indicates that surgically taking out the entire visible tumor (called gross total resection) can significantly boost survival rates when compared to surgeries where only a portion of the tumor is removed. Surgical innovations and imaging techniques in the operating room have evolved to facilitate complete tumor removal while trying to preserve patient’s neurological functions.
Alongside surgery, radiation therapy, which uses high-energy beams to kill cancer cells, is employed. Different approaches include methods like laser interstitial thermal therapy, brachytherapy, gamma knife, stereotactic radiosurgery, whole brain radiotherapy, and proton beam therapy. A commonly followed protocol combines radiation therapy with a medication called temozolomide. Recent technologies like tumor-treating fields, a type of electromagnetic field therapy, have also been recommended.
Chemotherapy is another important aspect of treatment. It involves using powerful drugs to kill cancer cells. Traditional medication N-methyl-N-nitrosourea (NMU) has been replaced by drugs like procarbazine and temozolomide, which are more effective for different types of glioblastoma. Developing technologies like nanoparticles are currently being studied to better deliver these medicines to the tumor cells.
The specific treatment plan is decided according to a patient’s age, overall health and specific characteristics of their tumor. For older patients in poor general health, shorter periods of radiation therapy may be preferred to lessen the burden of treatment. Another important aspect is the genetic status of the tumor. Patients with a specific change in their tumor’s DNA, often have a superior response to temozolomide, it therefore, forms an integral part of their treatment plan.
Newer therapeutic strategies are also being explored. This includes immune checkpoint inhibitors, cancer vaccines, virus-based therapies and therapies using modified immune cells. These target the patient’s immune system to better fight the cancer. Also, therapies targeting specific molecules in the tumor are being developed, with drugs acting against specific proteins like EGFR, mTOR, VEGF, and MEK being studied.
Looking ahead, the management of GBM is anticipated to benefit from innovative approaches. These include more sophisticated in-lab models, utilization of artificial intelligence and machine learning for diagnostic and treatment decision making, and studying of microscopic particles released from tumor cells to assess response to therapy.
What else can Glioblastoma Multiforme be?
Diagnosing GBM (glioblastoma) is quite challenging because it can closely resemble other brain conditions and tumors, both in symptoms and how it appears under imaging studies. This makes it important to differentiate GBM from other brain tumors whether they are primary (originated in the brain) or metastatic (originated somewhere else and spread to the brain), infections, inflammation, and blood vessel-related diseases. The key to correctly identifying GBM rests in understanding its unique characteristics, examining patients’ detailed clinical data, and using advanced imaging techniques.
Here are some of the conditions that should be considered when diagnosing GBM:
- Single brain metastasis (cancer that has spread to the brain from another part of the body)
- Primary CNS lymphoma (a type of cancer that starts in the central nervous system)
- Cerebral abscess (a pocket of pus in the brain)
- Subacute ischemic or hemorrhagic strokes (conditions resulting from reduced or blocked blood flow to the brain)
- Resolving contusions (bruises on the brain that are healing)
- Tumefactive variants of demyelination (conditions where the protective coating of nerve cells is damaged, causing symptoms similar to a tumor)
- Radiation necrosis (tissue damage caused by radiation therapy)
- Vascular malformations (abnormal clusters of blood vessels in the brain)
- Toxoplasmosis (an infection caused by a parasite)
Surgical Treatment of Glioblastoma Multiforme
The main aim of surgery for GBM, a type of brain tumor, is to take out as much of the tumor as possible while keeping you, the patient, safe and protecting your brain’s normal functions. This can help you live longer. However, because GBM spreads into the surrounding areas, it’s not always possible to completely remove all of it.
Studies from the Surveillance, Epidemiology, and End Results Program (SEER), suggest that removing a large portion or all of the tumor can help extend life longer than just taking a biopsy (a small tissue sample for testing) or not doing surgery at all.
Deciding whether to go for a full removal, a partial removal (also known as stereotactic biopsy), or surgery to ease symptoms (also known as palliative surgery) depends on where the tumor is in your brain, your age, other health conditions you might have, and what your care goals are. Most of the time, taking out a part or all of the tumor can help doctors make a definitive diagnosis and plan the treatment.
After the surgery, you should have another scan within 24 to 48 hours. This is to check how much of the tumor was successfully removed.
What to expect with Glioblastoma Multiforme
At present, the average survival rate after being diagnosed with this particular health condition only ranges up to 1.2 years. It has been reported that the median survival time is usually 15 months, and after 5 years, only 7.2% of patients are still living.
Several factors can affect a patient’s prognosis or the likely outcome of the disease. These factors can include one’s age, their overall health status, and the extent of surgical intervention. Younger individuals, those in good health, having MGMT gene methylation, and having the IDH mutant variant tend to have better survival rates. On the other hand, the IDH-wildtype variant of the disease is more aggressive and can affect survival rates negatively.
The role of the MGMT gene and the degree of methylation of its promoter region is also significant. This degree of methylation (which is a biological process affecting gene expression) in the MGMT gene promoter can affect prognosis. This also influences how they respond to certain treatments like TMZ. In comparison, patients with a different variant of changes in the DNA, specifically in the telomerase reverse transcriptase promoter (TERTp), and chromosome 10 deletion, tend to have less favorable prognosis.
In countries with lower income, several factors like inadequate diagnosis and treatment, economic hardship, lack of trained healthcare workforce, and poor healthcare infrastructure, can seriously affect patient outcomes. Therefore, it’s crucial to identify effective treatment elements for improving responses to combat the disease.
Efforts are being made towards precision medicine, which means tailoring the treatment plan based on the patient’s specific genetic make-up. This can often involve understanding the specific genetic changes in the disease, like the IDH mutation status, a method that is enhanced by the new field of radiomics.
Possible Complications When Diagnosed with Glioblastoma Multiforme
The chance of getting an infection at the site of the surgery increases if a person has had radiation therapy or multiple surgeries. This is over and above the issues that can arise from chemotherapy and radiotherapy, which have been discussed earlier. The actual disease also carries the risk of the cancer coming back, or recurrences.
After a Gross Total Resection (GTR) – which is a surgery where all visible tumor is removed – and additional chemotherapy and radiotherapy, the recurrence mainly happens in the region just around the tumor in the brain. This region has a harmful environment containing tumor cells, along with other cells associated with blood vessel growth, reactive cells called astrocytes, cells from the immune system (glioma-associated microglia/macrophages or GAMS), lymphocytes that have infiltrated the tumor, and glioma-associated stromal cells (GASCs). Studies show that in most cases – between 80% to 90% – the cancer tends to come back within 2cm from the original tumor.
Glioblastoma Multiforme (GBM) is often accompanied by something known as pseudoprogression or radionecrosis. This appears as worsening of the tumor on MRI scans taken within 3 months after completing chemotherapy and radiation. However, this is not true progression of the tumor and is a side effect of the treatment. It’s important not to mix up pseudoprogression with actual progression of the disease – this distinction can prevent unnecessary stoppage of treatment. One of the main difference is that pseudoprogression usually doesn’t cause symptoms and a type of MR spectroscopy test shows a peak for lactate.
Sudden onset of confusion and other symptoms of brain dysfunction, known as acute encephalopathy, and radiation-induced cancers are other significant problems that can arise from radiation therapy.
Common complications:
- Infection at the site of surgery
- Relapse or recurrence of the cancer
- Pseudoprogression or radionecrosis – a side effect of treatment that appears like worsening of the disease on MRI scans but is usually without symptoms
- Acute encephalopathy – sudden onset of confusion and other symptoms
- Radiation-induced cancers
Preventing Glioblastoma Multiforme
Glioblastoma multiforme (GBM), the most common type of brain cancer, is aggressive and originates from a type of brain cell known as the glial cell. As the tumor grows, it starts to press down on the surrounding brain cells. This pressure can lead to headaches, seizures, memory issues, personality changes, vision problems, difficulty with speech, weakness, and even paralysis. Some of these symptoms may seem similar to a stroke. However, the exact cause of GBM is still unknown. Research suggests having radiation treatment early in life could increase the chance of getting GBM.
The primary way of preventing GBM is to try to manage the known risk factors and encourage early detection. Although we don’t know the exact cause of GBM, limiting exposure to risk-elements such as certain types of radiation and chemicals might lower the chances of developing the disease. It may also be beneficial to make lifestyle changes such as maintaining a healthy weight, exercising regularly, and eating a balanced diet rich in antioxidants. These factors can contribute to overall brain health and thus potentially decrease the risk of GBM.
To diagnose GBM, doctors usually carry out a scan (CT or MRI), followed by a biopsy to confirm definitively. If the scan shows typical characteristics of GBM, doctors may suspect its presence. Once diagnosed, the healthcare professionals discuss the best course of action with the patient and their family. Treatment typically includes radiotherapy and chemotherapy after surgical removal of the tumor. Despite aggressive treatment, GBM is known to have poor survival rates and a high likelihood of recurrence. Most patients survive between 1 to 2 years after the diagnosis. Because of the high recurrence rate, patients are advised to have frequent check-ups and imaging tests, even after treatment is completed.
Raising awareness about the signs of GBM and emphasizing the importance of timely medical intervention can lead to an earlier diagnosis and treatment, which may improve the chances of a better outcome for patients. Ongoing research into how GBM develops and finding new preventive measures are vital in the fight against this aggressive disease.