What is Hepatoblastoma?
Hepatoblastomas, which are the most common type of liver cancer in children, typically occur within the first two years of a child’s life. This cancer can be divided into two main types: epithelial type and mixed type. In the past three decades, advancements in treatment have led to chemotherapy being the standard treatment for most cases. Combining this type of chemotherapy with surgery can successfully cure the cancer in about 70% of cases, a significant increase from the 30% cure rate in the 1970s.
The outlook for a patient with hepatoblastoma depends on various factors. These include the level of a specific protein called alpha-fetoprotein in the body, the age of the child when the cancer is diagnosed, how successful the surgery was in removing the cancer, and the severity or stage of the disease at the time of diagnosis.
What Causes Hepatoblastoma?
Most tumors happen randomly, but about a third are linked with certain conditions such as Beckwith-Wiedemann and Down syndrome. Infants with low birth weight are more likely to develop a type of liver cancer called hepatoblastoma. Some studies indicate that having preeclampsia (a pregnancy complication characterized by high blood pressure) and parents who smoked during pregnancy could also increase the risk of hepatoblastoma. Other potential risk factors include oxygen therapy, certain medications such as furosemide (a diuretic), radiation, plasticizers (chemicals used to make plastics flexible), and total parenteral nutrition (feeding a person intravenously).
The most common genetic mutation seen in hepatoblastoma cases affects the Wnt signaling pathway, which is a network of proteins that pass signals into a cell through cell surface receptors. This usually results in the buildup of a protein called beta-catenin. In more differentiated types – or mature cancer cells, beta-catenin usually shows a membranous staining pattern (it’s present on the exterior). In less differentiated, or more immature cancer cells, the staining of beta-catenin is usually seen in the nucleus (the cell’s center). In severe cases, the activation of TERT (an enzyme that helps protect the ends of chromosomes) and MYC (a gene that helps control cell division) has also been observed.
Risk Factors and Frequency for Hepatoblastoma
Hepatoblastoma is a rare type of children’s cancer, making up about 1% of all such tumors. It’s slowly becoming a bit more common in North America and Europe. This condition is slightly more common in boys than girls.
Signs and Symptoms of Hepatoblastoma
Hepatoblastomas are typically experienced as a single, mild ache in the abdomen that grows quite rapidly. This condition is often found in the right side of the liver in about 55% to 60% of cases. Although these tumors can increase in size quickly, it’s rare for them to rupture or bleed. Tumors can grow up to 25 cm large. While most tumors appear alone, up to 15% of them can be multifocal, meaning there are multiple tumors. Some people might also experience non-specific symptoms like weight loss, lack of growth, or loss of appetite. Around 90% of patients observe a significant increase in alpha-fetoprotein (AFP), a substance produced by the tumor. In rare cases, a paraneoplastic syndrome, a condition that arises from the body’s response to the presence of cancer, may occur.
Testing for Hepatoblastoma
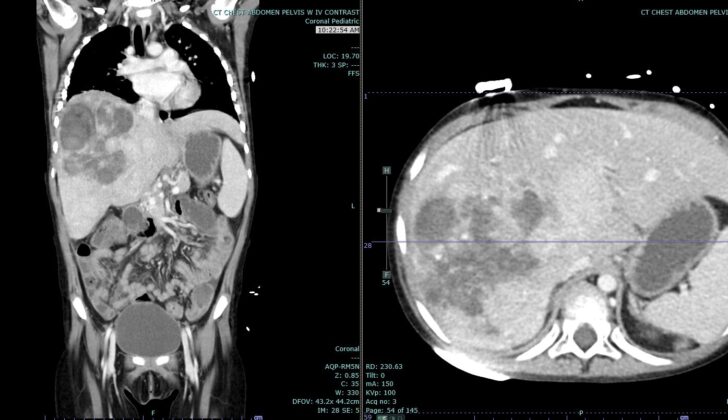
Ultrasound, alongside other imaging techniques such as computed tomography (CT) scan or magnetic resonance imaging (MRI), is used to determine the size and spread of the liver tumor and to plan for possible surgery. A CT scan of the chest could also be done to find out if the cancer has spread to the lungs, as the lungs are the most common place where this kind of cancer spreads. In fact, up to 20% of all such cases show lung spread.
After these scans, a biopsy, or a small tissue sample from the liver, may be taken. This helps doctors understand the type and characteristics of the cancer. Additionally, doctors may measure the levels of a protein called alpha-fetoprotein in your blood, as higher levels can sometimes suggest liver cancer. Your liver function would also be assessed through a series of blood tests, which would tell doctors how well your liver is working. They may also do a hepatitis panel, a series of tests that check for a hepatitis infection, which is a common cause for liver diseases and cancers.
If you are eligible, doctors might ask for your permission to use some of your biopsy sample in research studies, which can help improve our understanding and treatment of this type of cancer.
Treatment Options for Hepatoblastoma
Surgery is the primary strategy to treat cancer, with the possibility of removing the tumor determining whether pre- or post-surgery chemotherapy is needed. When patients first come to the doctor, about 60% of tumors are too big or difficult to remove surgically. If chemotherapy doesn’t make the tumor small enough to remove, a liver transplant can be an option and usually leads to a good chance of long-term survival. The usefulness of radiation therapy is not certain, but some cases that can’t be operated on respond well to it.
Alpha-fetoprotein is a substance produced by tumors. The level of this substance can be used as an indicator to track if the surgery was a success and to see if the tumor has spread to other parts of the body. Some reports suggest that there’s a higher risk of a condition called post-transplant lymphoproliferative disorder, which involves the abnormal growth of lymphocytes (a type of white blood cell), after liver transplants. This condition could occur due to the weakened immune system from the treatment for the transplant.
What else can Hepatoblastoma be?
When doctors are trying to diagnose a condition affecting the liver, they need to consider several possibilities. These include:
- Hepatocellular carcinoma (HCC) – a type of liver cancer that generally affects adults with risk factors like metabolic disorders, liver cirrhosis, or a history of childhood hepatitis B.
- Focal nodular hyperplasia – a condition often found in older children and adults.
- Hepatic adenoma – which can look similar to certain types of hepatoblastoma (a rare liver cancer found in children), but is unusual in children under 5 unless they have a metabolic disorder.
- Lymphoma – cancer that begins in the cells of the body’s immune system.
- Metastases – cancer that has spread from where it started to another part of the body.
It’s crucial for the doctor to evaluate these different conditions, as they can all present with similar symptoms.
What to expect with Hepatoblastoma
The outlook or prognosis of a medical condition can be influenced by a lot of factors. It can depend on things like the patient’s age when diagnosed, the PRETEXT group (a system used to classify how much of the liver is involved in the disease), whether the disease has spread to other parts of the body (metastases), levels of a protein called alfa fetal protein (AFP), the specific type of disease cells (histologic subtype), how much of the disease was removed during surgery (completeness of resection), and how advanced the disease was at the time of diagnosis.
One thing to point out is that certain types of disease cells have a better or worse prognosis. For example, a well-differentiated fetal subtype is linked to a better prognosis compared with small cell undifferentiated type and macrotrabecular type, which tend to have less favorable outcomes. However, this information is usually only useful before starting chemotherapy.
AFP is usually high when first diagnosed but if it goes down significantly after beginning chemotherapy, this typically suggests that the treatment is working well. Although it used to be thought that younger patients had worse outcomes, recent studies have suggested that younger patients fare just as well as older children.
That being said, children younger than 1 year of age seem to have a better outlook, and children older than 6 years have a poorer outlook. Other factors associated with a poorer prognosis include disease still present on the edges of the surgical area (resection margin), disease in multiple areas (multifocality), and disease that has spread to other parts of the body (metastases). Additionally, certain proteins like beta-catenin and EpCAM have been linked to a shorter period of survival without disease symptoms and a poorer response to chemotherapy, respectively.
Possible Complications When Diagnosed with Hepatoblastoma
- Breakage of the tumor inside the abdomen
- Complications brought about by cancer treatment drugs
- Problems that occur after undergoing a transplant surgery
- Mental and social impacts of treatment and painful procedures