What is Krukenberg Tumor?
A Krukenberg tumor is named after Friedrich Ernst Krukenberg, who mistakenly identified it as a new type of ovarian cancer. However, it was later found to be a type of cancer that had spread to the ovary from another part of the body. In some parts of the world, about 10% of ovarian tumors are due to such metastatic diseases, and almost half of these are Krukenberg tumors. This type of tumor is more common in Japan, Korea, and China, making up about 18% of cases, because stomach cancer, which can cause Krukenberg tumors, is more common there.
Krukenberg tumors often originate from the stomach, but they can also start in other organs such as the appendix, breast, colon, small intestine, gallbladder, pancreas, and the urinary and reproductive system. The cancer typically spreads via the lymphatic system, which is part of the body’s immune system, but can also spread through the blood or by directly invading nearby tissues. Sometimes, the original site of the tumor can’t be found. The symptoms of a Krukenberg tumor can be the first sign of cancer. These tumors can cause symptoms like pain, bloating, fluid build-up in the abdomen (ascites), irregular vaginal bleeding, painful sexual intercourse (dyspareunia), and hormonal changes.
Treatment for Krukenberg tumors depends on the characteristics of the original cancer and unfortunately, the prognosis is generally less positive compared to other types of ovarian tumors. On average, patients live for about 14 months after diagnosis. Treatment options, including surgery and drug therapy, can extend life expectancy in some patients. To plan the most effective treatment, doctors will need to consider multiple factors, such as where the cancer originated, how far it has spread, and the patient’s general health.
What Causes Krukenberg Tumor?
A Krukenberg tumor is a specific type of cancer that usually begins in the stomach, specifically near the exit of the stomach, an area known as the pylorus. About 70% of these tumors come from this area. The next most common place for it to start is in the colon or large intestine, and it seems that the frequency of this origin is increasing.
If we combine the cases from the stomach and the colon, those two places account for roughly 90% of the origin sites of Krukenberg tumor. There are a few other places where this cancer can start, but they are less common. These include the breast and appendix. Even rarer, they can start in places like the small intestine, gallbladder, an area of the kidney known as the ureter, bladder, the biliary tract which is part of the liver, the pancreas, the ampulla of Vater which connects the pancreas to the small intestine, and the cervix.
Risk Factors and Frequency for Krukenberg Tumor
Krukenberg tumors are found in 5% to 10% of women who have stomach cancer. They often go unnoticed until the disease becomes severe. These tumors are more common in Korea, Japan, and China, accounting for 20% of all ovarian cancers due to the prevalent rate of a specific type of stomach cancer—signet-ring cell gastric cancer—in these regions.
On average, women are diagnosed with Krukenberg tumors around the age of 48, though it can occur in females anywhere from 27 to 65 years old. The condition is most common in women with primary gastrointestinal tract tumors, and less so in those with breast cancer. Younger women are more likely to develop ovarian metastases due to increased ovarian blood supply which makes the ovary more susceptible to metastatic disease. Moreover, younger women typically have a specific type of stomach cancer—signet-ring type gastric adenocarcinomas—that often spreads to the ovary.
Krukenberg tumors can be categorized into two types based on the timing of metastasis detection in relation to the diagnosis of the primary tumor:
- They can be “synchronous”, meaning the metastasis is found within 3 months of diagnosing the primary tumor.
- Or they can be “metachronous”, meaning the metastasis is detected after 3 months, often after the primary tumor’s initial treatment is complete. It’s worth noting that ovarian metastases can occur years after the primary cancer has been treated.
In 80% of the cases, Krukenberg tumors affect both ovaries and are the most common type of tumor to do so. As opposed to primary ovarian cancers, they respond less to chemotherapy. Metastases in the ovaries are also less responsive than synchronous metastases found elsewhere. For those diagnosed, the survival rate is typically less than a year.
Signs and Symptoms of Krukenberg Tumor
Krukenberg tumor is a type of cancer that can remain undetected due to a lack of symptoms until it grows larger or causes hormonal changes. The symptoms of this tumor might be the first indication of cancer. These symptoms are not specific and include various physical changes.
- Increased size of abdomen
- Fatigue
- Abdominal and pelvic pain
- Unusual bleeding from the uterus
- Excessive body hair and masculinization in women
- Pain during sexual intercourse
Some late-stage effects of this condition include fluid buildup in the abdomen (ascites), blockage of the intestine, and severe weight loss (cachexia). Additionally, the presence of Krukenberg tumor together with benign ascites and fluid in the right side of the chest is known as Pseudo-Meig’s syndrome. Also, tumor growth can lead to twisting of the ovary or fallopian tubes, a condition referred to as ovarian or adnexal torsion.
Testing for Krukenberg Tumor
Krukenberg metastasis is a type of cancer that has spread from its original location to the ovaries. Doctors often discover Krukenberg metastasis before they can diagnose where the primary, or original, tumor is located. Symptoms can be vague, which may lead your doctor to order imaging tests like a computed tomography (CT) scan initially. But, they might spot the lesion first with an ultrasound. As a follow-up, they could use CT or magnetic resonance imaging (MRI) to get clearer details about the condition in your ovaries and perhaps find where the primary cancer is.
It’s crucial to distinguish between Krukenberg metastasis and a original cancer in the ovaries because the forecast and treatments for these are quite different. In a review of Krukenberg tumor cases, researchers found that about half of these metastatic cancers were on the same side as the original tumor, two-thirds were in both ovaries, one-third were over 10 cm in diameter, and half showed peritoneal involvement, which means the cancer has spread to the membrane lining the abdominal cavity.
With an ultrasound, your doctor might see masses in the ovaries that are either solid, have fluid-filled sacs (cysts), or a mixture of both. These tumors usually have distinct borders and a pattern that resembles a moth-eaten cyst with blood vessels branching out from the center of the mass. This is different from the appearance of primary ovarian cancers, which tend not to have clear boundaries and have irregular thick sections.
A CT scan helps measure the spread of the metastatic cancer, locate the primary tumor, and find any swollen lymph nodes in your abdomen. If looking for the original cancer, doctors often check the stomach, biliary tract (the path by which bile goes from the liver to the small intestine), pancreas, colon, and appendix. If you get an MRI, Krukenberg tumors usually appear as distinct oval tumors with cystic bodies, dark areas on T2 imaging due to a reaction in the supportive tissue, and bright areas on T2 imaging due to a protein called mucin.
Biopsies, which are small tissue samples taken from any suspicious sites spotted by imaging, are crucial. National Comprehensive Cancer Network (NCCN) guidelines for investigating Krukenberg tumors suggest a thorough check of the gastrointestinal tract, including a look at the esophagus, stomach, and duodenum using an endoscope (a flexible tube with a light and camera). Doctors also test the biopsied tissue for specific protein markers.
If the tissue stain tests negative for cytokeratin 7 (CK7) and positive for cytokeratin 20 (CK20) or both proteins test positive, it suggests that the cancer has spread from the digestive tract. An increased level of a substance called carcinoembryonic antigen (CEA) in an ovarian tumor also points toward a metastatic process. Doctors can use an elevated CA‐125 level in the context of a Krukenberg tumor to assess how complete the surgical removal of the cancer was, know if metachronous metastasis (cancers that appear at different times) from a known primary cancer exists, and determine the overall forecast. A study indicated that levels of CA‐125 over 75 U/mL were connected with lower survival rates over five years.
Treatment Options for Krukenberg Tumor
Treatment approaches for Krukenberg tumors, a type of cancer, are not standardized due to the variety of tumor types they represent. However, the core strategies for treating Krukenberg tumors usually include chemotherapy and a type of surgery called cytoreductive surgery.
Krukenberg tumors tend to have a lower response rate to chemotherapy compared to tumors in other parts of the body. Hence, a surgical procedure to remove the tumor (metastasectomy) may boost the effectiveness of chemotherapy for the rest of the disease.
Medical teams combat Krukenberg tumors through a combination of chemotherapy, surgery, targeted immunotherapies, and radiation. They often look to treatment plans followed for the original tissue where the tumor came from.
Cytoreductive surgery, which aims to decrease the size of the tumor, is believed to increase the patient’s overall survival rate better than just using chemotherapy. Chemotherapy can be administered before (neoadjuvant) and/or after (adjuvant) surgery, or at the same time as the surgery via a procedure known as hyperthermia intraperitoneal chemotherapy (HIPEC), where chemotherapy is heated and directly applied into the abdominal cavity.
What else can Krukenberg Tumor be?
When identifying Krukenberg tumors, it’s important to differentiate them from other conditions such as primary ovarian cancer and metastatic processes like mucinous carcinoids. To tell them apart, medical professionals use special staining techniques, along with examining the appearance and structure of the tumors. This is crucial as different conditions require different treatments and have different impacts on a patient’s health.
- Mucinous carcinoids are confirmed by their positive reaction to chromogranin and synaptophysin stains, differentiating them from Krukenberg tumors.
- While primary ovarian cancer and Krukenberg tumors may look similar, they can be distinguished using histological and immunohistochemical analyses.
- Primary ovarian tumors often contain mucin and usually affect one ovary. These also include non-mucinous tumors like benign signet-ring stromal tumors, sclerosing stromal cell tumors, and clear cell ovarian adenocarcinoma.
- When a tubular Krukenberg tumor is suspected, it should be differentiated from other ovarian cancer types like Sertoli-Leydig cell tumors, endometrioid carcinoma, and tumors originating from Wolffian origin.
A recent comparison study found that primary ovarian cancer usually tests strongly positive for cytokeratin 7 (CK7) and negative for cytokeratin 20 (CK20), a distinction from Krukenberg tumors, which generally test positive for either or both CK20 and CK7.
Interestingly, the average age of diagnosis varies between the two conditions. Generally, primary ovarian cancer patients are usually diagnosed at around 65 years old, whereas Krukenberg patients are typically diagnosed under 50 years old.
The CA-125 tumor marker level can also provide some clues. It’s usually higher in primary ovarian cancer patients, with median levels around 652 u/mL compared to Krukenberg tumors’ median of 43 u/mL. For two other markers, CEA and CA19-9, the values are typically higher in Krukenberg tumors than in primary ovarian malignancies.
Surgical Treatment of Krukenberg Tumor
A Krukenberg tumor is a type of cancer that usually begins in the stomach or colon and spreads to the ovaries. The main treatment for Krukenberg tumor is a surgery called R0 surgical resection, which aims to remove all visible traces of the tumor and ensure no microscopic remnants are left at the surgical site.
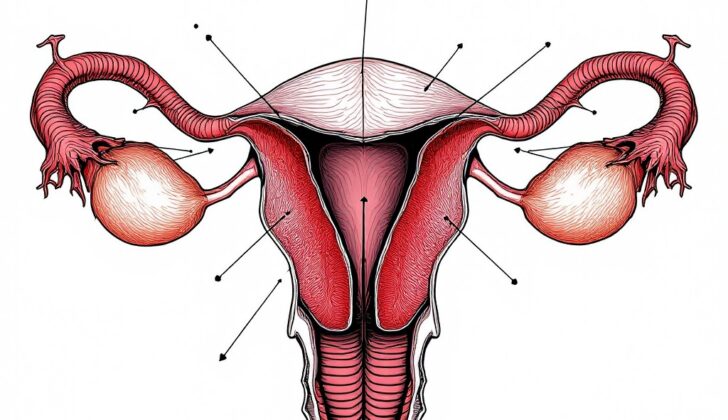
In some cases, it’s recommended to remove both ovaries, even if the disease is only found in one, to prevent its spread. Studies have shown patients with Krukenberg tumor who underwent surgeries like unliteral or bilateral salpingo-oophorectomy (removal of one or both fallopian tubes and ovaries), or total hysterectomy (removal of the uterus and cervix) along with bilateral salpingo-oophorectomy, lived a median of 17 months longer.
Patients with primary gastric or colon cancers and Krukenberg tumors showed improved survival when both the primary tumor and the spread ovary tumor are removed completely.
Research has indicated that overall survival improves for patients who have surgery to remove the Krukenberg tumor compared to just receiving chemotherapy. Further analysis showed that patients with stomach cancer and spread ovarian cancer had a significantly longer survival rate when removal of the spread ovary tumor took place before starting chemotherapy, compared to those who had simultaneous stomach and spread tumor removal after chemotherapy. Using a procedure called hyperthermic intraperitoneal chemotherapy (HIPEC), which delivers heated chemotherapy directly into the abdominal cavity, improved survival rates in patients with spread tumors in the abdomen.
What to expect with Krukenberg Tumor
Patients with Krukenberg tumors, a common type of cancer, often have a life expectancy of up to two years. The average survival time is about 14 months. The survival time can vary based on where the cancer originated. For instance, averages are 11 months for stomach cancer, about 22 months for colorectal cancer, about 31 months for breast cancer, and nearly 20 months for other types.
Patients with a Krukenberg tumor in one organ rather than in multiple locations (unilateral Krukenberg tumors) tend to have a better chance of survival, as do those who can successfully receive a surgical procedure (R0 resection) to fully remove the cancer. Colorectal cancer patients typically have better survival rates than stomach cancer patients, especially if they receive a type of chemotherapy (HIPEC) during surgery (R0 resection).
Several factors can influence survival rates. These include a surgical procedure to remove metastases (metastasectomy), presence of certain types of cells (expressive estrogen receptor beta, progesterone receptor, and signet-ring cells), and the presence of certain molecules (tyrosine kinase receptor Erb and progesterone receptor) in certain types of stomach cancer. Negative factors include developing tumors in multiple locations at once (synchronous presentation of tumors), abdominal fluid accumulation (ascites), high levels of a protein marker (CEA) and a cell protein (PD-L1), involvement of the peritoneum (lining of the abdominal cavity), and spread to blood or lymph vessels (lymphovascular invasion).
Doctors use tumor markers to track how well the treatment is working. CA-125 is one such marker which can decrease after successful tumor removal and might signal that the cancer has come back if it rises again. Rising levels before surgery could indicate that the cancer has spread, and the value of CA-125 before surgery could give clues about the patient’s prognosis (outcome).
Possible Complications When Diagnosed with Krukenberg Tumor
Problems related to Krukenberg tumors can involve twisting of the ovaries (known as ovarian torsion) and blocking of the small intestine, leading to obstruction.
Possible Conditions of Krukenberg tumors:
- Twisting of the ovaries (Ovarian Torsion)
- Blocking of the small intestine (Small Bowel Obstruction)
Preventing Krukenberg Tumor
It’s very important to understand your health conditions, especially when something as serious as Krukenberg tumors is involved. This type of tumor is not the same as a regular ovarian cancer – instead, it’s a cancer that has spread to the ovaries from another area of the body. By learning about it, you would be able to detect it earlier and know how to manage it better.
Knowing the signs and symptoms of cancers that affect the ovaries, including Krukenberg tumors, can be a real life-saver. These might include abdominal pain, bloating, unusual vaginal bleeding, changes in bowel habits, or other related symptoms. If you notice any of these, don’t put off seeing a doctor. Early detection can greatly improve the chances of successful treatment.
Understanding the risk factors for Krukenberg tumors will also help you take preventive measures. Making sure to follow doctors’ recommendations for screenings like colonoscopies and mammograms can also help in early detection. Remember, maintaining health is not just about treatments, it’s also about prevention and early detection, and the first step towards this is education.