What is Leiomyosarcoma?
Leiomyosarcoma is a common type of cancer, known as a soft tissue sarcoma, making up 10% to 20% of all sarcoma cases. It comes from cells known as smooth muscle cells or the cells that these muscle cells come from, called mesenchymal cell precursors. Most common places where it arises are the areas in the back of the abdomen (retroperitoneum), uterus, and arms or legs, decreasing in frequency in that order.
Leiomyosarcoma’s genetic makeup is quite complex and we have yet to fully understand it. How it shows up in terms of symptoms and signs can change depending on where it comes from. How the illness turns out (prognosis) depends on where the tumor is, its size, and its grade, with the grade of the tumor significantly affecting how long a patient might live. Higher grade tumors, those that are more serious, increase the chance of the cancer spreading.
Treatment options vary and often require collaboration across different medical disciplines. Usually, the first line of treatment is surgery to remove the tumor if it’s possible, with treatments like chemotherapy and radiation often used in addition to surgery. Treatment in specialized sarcoma centers is recommended as it has been shown to improve patient’s results. Recent developments in precision medications and immunotherapy (treatments that use your immune system to fight the cancer) might improve patient outcomes in the future.
What Causes Leiomyosarcoma?
There isn’t a specific cause for a type of cancer called leiomyosarcoma, but there are certain things that may increase your chances of getting it. A key risk factor for this cancer is having previously been exposed to radiation, or having undergone radiotherapy, particularly if you were young when this happened.
There are also certain genetic conditions which might make it more likely for you to develop this cancer. For example, Retinoblastoma (a disease that is caused by the deletion of the RB1 gene), and Li-Fraumeni syndrome (caused by changes in the TP53 gene), are both syndromes which might be related to developing this form of cancer.
Risk Factors and Frequency for Leiomyosarcoma
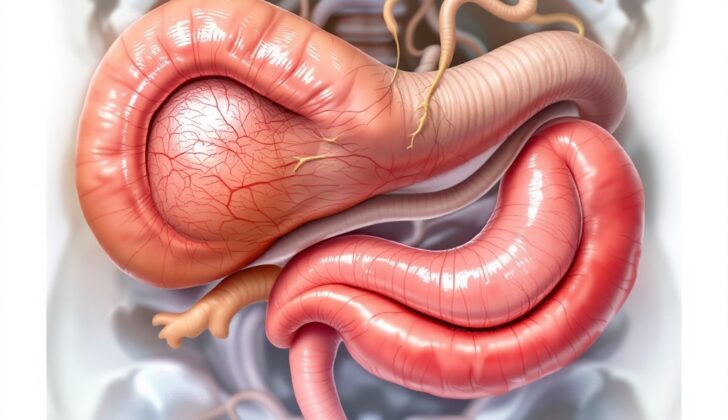
Leiomyosarcoma, a type of soft tissue sarcoma, makes up for 10% to 20% of these newly caught conditions. The improvements in the field have recently made it easier to diagnose accurately. Most often, it occurs in a part of the abdomen, followed by the uterus, limbs, and torso. It’s worth noting that within 3% to 7% of uterine cancers, leiomyosarcoma is the most prevalent, making up around 80% of all such cases.
People tend to experience leiomyosarcoma more as they age, with the highest incidence in those in their 70s. However, one type – uterine leiomyosarcoma – is most common in women around the age of menopause. If the tumors are linked to genetic syndromes, they may occur earlier in life. Furthermore, leiomyosarcoma found in the abdomen or originating from internal blood vessels is more common in women. On the other hand, leiomyosarcoma found in other areas, is more prevalent in men.
Signs and Symptoms of Leiomyosarcoma
Leiomyosarcoma is a type of cancer that can present in different ways based on where it’s located. Symptoms usually arise from the tumor pressing on nearby organs. For example, in the retroperitoneum area, a tumor can grow significantly before causing noticeable symptoms. If it’s in the uterus, it’s often found when examined under a microscope after a woman has a hysterectomy for a believed leiomyoma, a different type of benign tumor.
Testing for Leiomyosarcoma
If your doctor suspects you might have a sarcoma (a type of cancer), they will start with specific tests. These will help understand the size and location of the tumor and how to best biopsy it, which means taking a small sample of the tumor for closer examination.
Computed tomography (CT scan – an X-ray that gives detailed images of the inside of the body) and magnetic resonance imaging (MRI – a type of imaging that uses a magnetic field and radio waves to create detailed images of the inside of the body) are common tests used. While CT scans are good at examining areas in the back of your abdomen, MRI’s are useful for looking at tumors in the arms, legs, and head and neck.
Your doctor may start with the imaging test that’s most readily available. However, once a sarcoma is suspected, a type of biopsy called image-guided core needle biopsy is needed for a definite diagnosis. This biopsy uses a needle to remove a little bit of the tumor, guided by imaging such as an ultrasound or CT scan. This is different from a fine-needle aspiration, which collects cells from the tumor but doesn’t provide enough information to confirm a sarcoma diagnosis.
When doing a biopsy for a tumor you can feel, the image guidance helps make sure the sample is accurate. For tumors deep in the abdomen, the biopsy must be done in a particular way to avoid spreading the cancer cells in your abdomen. For surface tumors, it’s important to plan the biopsy and any future surgery together.
It’s recommended that patients suspected to have a type of sarcoma called soft tissue sarcoma (STS) be referred to a medical center that handles a large volume of these cases. That’s because incorrect initial tests, especially incorrect surgeries, can cause problems in tissue and potential spreading of cancer cells and make any future surgeries more complex.
A chest and abdominal CT scan are necessary due to the risk of sarcoma spreading through the bloodstream. For women with a suspected uterine leiomyosarcoma, a specific type of cancer, an endometrial biopsy, which is a sample taken from the lining of the uterus, can confirm the diagnosis. However, if this biopsy doesn’t find cancer, it doesn’t necessarily mean the patient doesn’t have leiomyosarcoma. In cases where there’s a suspected tumor in the uterus that continues to grow after menopause, it should be evaluated to ensure it’s not leiomyosarcoma.
Treatment Options for Leiomyosarcoma
Leiomyosarcoma is a rare type of cancer that can occur in many parts of the body. The way it’s managed, or treated, relies on several factors, such as where it started growing in the body, its size, its grade (which reveals how abnormal cells are and how quickly the tumor is likely to grow and spread), and the patient’s overall health.
Common treatment options are surgery for removing the tumor, radiation therapy (using high-energy beams to kill the cancer cells), and chemotherapy (using drugs to kill the cancer cells). Overseeing the treatment should ideally be a team of experienced professionals from various medical disciplines, based at a major healthcare centre that sees a lot of sarcoma patients.
The primary targets of curative treatment, or treatment designed to completely rid the body of cancer, are to remove the tumor and leave a margin of healthy tissue around it (known as surgical resection with negative margins), minimize chances of the cancer coming back locally (reducing local recurrence), enhance the patient’s daily life post-surgery (improving functional outcomes), and reduce the likelihood of the cancer spreading to distant parts of the body (reducing the risk of distant metastasis).
It’s important to highlight that radiation treatment in treating soft tissue sarcoma (STS), under which leiomyosarcoma falls, has been shown to better control local tumor growth, prolong the functioning of affected body parts, and decrease the chances of local cancer returning. However, radiation hasn’t been shown to lengthen patients’ overall survival time.
The timing of when to administer radiation treatment is also a topic of ongoing discussion among medical professionals in the case of leiomyosarcoma, whether it started in the body’s rear cavity (retroperitoneal) or limbs or torso (extremity or trunk leiomyosarcoma). Further research is being conducted in the form of major clinical trials to gather more patients and data amidst this debate.
The information on treatment is offered in subsequent sections for your reference.
What else can Leiomyosarcoma be?
Soft tissue sarcoma (also known as STS) can be tricky to identify because its symptoms are quite general and unspecific. Even its microscopic appearance during examination, which is the main way to diagnose it, requires additional testing such as immunohistochemistry, classical cytogenetics, and molecular testing to confirm the diagnosis. In fact, there are over 70 different types of sarcoma that the World Health Organization acknowledges.
There are other conditions with similar symptoms or microscopic appearances that doctors should consider when diagnosing STS:
- Meningioma
- Gastrointestinal stromal tumors
- Leiomyoma
- Dedifferentiated liposarcoma
- Endometrial stromal sarcoma
- STUMP (Smooth Muscle Tumor of Uncertain Malignant Potential)
- Inflammatory myofibroblastic tumor
- Perivascular epithelioid cell tumor
Surgical Treatment of Leiomyosarcoma
For patients diagnosed with leiomyosarcoma, a type of cancer that affects smooth muscle tissue, similar surgical principles that apply to any sarcoma are followed.
If leiomyosarcoma is located in the arms, the legs, or the trunk of the body, the primary goal of the surgery is to remove the entire tumor while also trying to keep crucial nerve and blood vessel structures intact. In the past, amputation was commonly used when the entire tumor couldn’t be neatly removed. Nevertheless, to maintain limb function or preserve important structures like the sciatic nerve (the largest nerve in your body that begins in your lower back and runs through the buttock and down the lower limb), an incomplete tumor removal is considered acceptable today. While it is associated with higher local recurrence rates (the cancer coming back), the overall survival is mainly determined by whether the cancer has spread to other parts of the body. Recent research suggests that a tumor margin with cancer cells that can only be seen under a microscope, when treated properly, won’t significantly increase the chance of the cancer spreading or decrease overall survival. If cancer cells might remain after surgery, radiations before surgery, re-resection, follow-up radiation, or close monitoring could be considered.
If leiomyosarcoma occurs in the retroperitoneum (the anatomical space in the abdominal cavity behind the abdominal lining), it often presents as large tumors and usually starts from the smooth muscle lining of medium to large veins, such as the inferior vena cava (the large vein that carries deoxygenated blood from the lower and middle body into the heart) and the gonadal veins. The major challenge here is to get a ‘negative margin’ i.e. to fully remove the tumor along with a layer of healthy cells. Removing the tumor together with any affected nearby organs is linked with the best outcome for operable tumors. Predominantly, Leiomyosarcomas compress the adjacent organs but do not invade them, therefore, it is possible to keep the organs around the tumor. Tumor rupture and spillage are usually linked with negative outcomes and should be prevented. Preoperative radiation is considered inefficient in reducing local recurrence (the cancer coming back) and improving survival in this case.
When Leiomyosarcoma affects the uterus, removing the uterus and the tumor in one piece are the standard surgical methods. While removal of both ovaries is usually suggested, in some young women who haven’t reached menopause yet, ovarian preservation can be discussed. Unlike carcinomas (cancer that starts in the skin or the tissues that line or cover internal organs), the rate of cancer spreading to the lymph nodes (a small bean-shaped structure that is part of the body’s immune system) in leiomyosarcoma is low, so a surgical procedure to remove the lymph nodes isn’t necessary. Extrauterine disease (cancer spreading beyond the uterus), if it can be removed, should be completely excised.
For disease that has metastasized (spread to other parts of the body) or recurred (come back), the current National Comprehensive Cancer Network guidelines recommend removing metastases in the lung for disease that has exclusively spread to limited areas in the lung in highly selected patients. Local recurrences should be managed with surgical resection if complete tumor removal is possible.
What to expect with Leiomyosarcoma
There are three major factors that can help predict the outcome of cancer: the cancer’s histologic grade (its cell structure), tumor size, and the depth of the tumor. The tumor’s size, whether or not it’s affecting bones or blood vessels, and the grade of the tumor significantly affect the outcome, especially in a type of cancer known as leiomyosarcoma. Tools have been developed to help calculate cancer prognosis based on these factors.
The histologic grade can independently predict the severity or aggressiveness of cancer, the likelihood of it spreading to other body parts (metastasis), and survival. Leiomyosarcoma, in particular, is an aggressive type of cancer; 90% of diagnosed patients have moderately to severely aggressive cancer, which places them at a higher risk for distant recurrence and reduced survival.
The location of the tumor also affects the outcome. Leiomyosarcomas located on extremities (arms or legs) tend to have a better prognosis than those located in the retroperitoneal region (back of the abdomen). Furthermore, tumors in the uterus or those originating from large blood vessels often have worse outcomes. The tumor’s depth, regardless of its size and grade, also correlates directly with a worse outcome.
It’s important to note that the factors determining prognosis are applicable to leiomyosarcoma found in the uterus as well. Factors such as age, stage of the disease, surgical margins (whether any cancer was left behind after surgery), tumor size, cell abnormalities, rate of cell division, lymph node involvement, and whether necrosis (cell death) is present can all influence the prognosis.
Recently, a group of scientists studied 580 patients with metastatic Soft Tissue Sarcoma (STS), a group of cancers affecting the soft tissues like fat, muscle, and blood vessels, with lung-only metastasis. The study found that patients who had cancer spread to the lining of the lungs had the worst outcomes. The best overall survival and progression-free survival (the time a patient lives with the disease without it getting worse) was observed in patients treated with a combination of three specific anticancer drugs: doxorubicin, ifosfamide, and a drug from the group of trabectedin or brostallicin.
Possible Complications When Diagnosed with Leiomyosarcoma
The complications associated with leiomyosarcoma, a type of cancer, are specific to the area of the body in which it occurs. Common problems can include pressure on surrounding areas due to the tumor’s size and rapid spreading of the cancer to other parts of the body because the tumors are aggressive.
Preventing Leiomyosarcoma
Leiomyosarcoma is a rare and aggressive type of soft tissue cancer, commonly seen in older patients. The cause of this disease is largely unknown. If patients notice soft tissue masses in areas like the abdomen or limbs, particularly if these masses are growing, they should seek a specialist for an evaluation. Tumors in the abdomen or pelvis often display vague symptoms that may vary based on their location.
Patients are strongly encouraged to seek diagnosis and treatment at a well-established hospital or medical center. The main method of treatment for this condition is surgery to remove the tumor, supplemented by radiation or chemotherapy treatments. Unfortunately, in cases where the cancer has spread to other parts of the body (metastatic disease), the illness is typically fatal and does not respond well to most treatments.
Patients are highly encouraged to participate in clinical trials. These trials are research studies conducted with patients to understand the disease better and to discover more effective treatments. These investigations are crucial in improving our understanding and treatment of this disease.