What is Leptomeningeal Carcinomatosis?
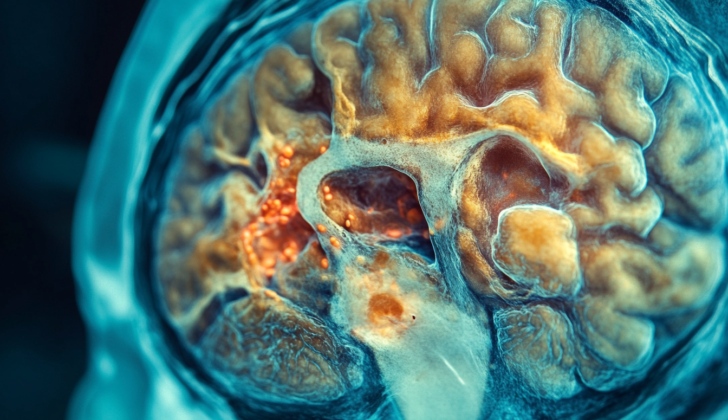
Leptomeningeal carcinomatosis (LC), or “leptomeningeal metastasis” or “carcinomatosis meningitis,” refers to a condition where cancer affects specific parts of the brain known as the pia and arachnoid mater, with a space called the subarachnoid space in between. It first came into medical knowledge in the late 19th century, and many researches have been conducted since then.
This disease occurs when solid tumors, including brain tumors, and blood-related cancers spread to affect the leptomeninges (layers covering the brain). However, this condition is not very common and usually occurs late in the disease’s progression, being seen in 5% to 8% of solid tumor cases and 5% to 15% of blood-related cancer cases. The disease is serious as it often signifies a poor outlook for the patient and has limited treatment options.
What Causes Leptomeningeal Carcinomatosis?
Most solid cancers can lead to a condition called leptomeningeal carcinomatosis (LC). The most typical types of solid cancers that involve the leptomeninges (the two innermost layers of tissue that cover the brain and spinal cord) include those from the breast, lungs, skin (melanoma), digestive tract (gastrointestinal), and brain and spinal cord (primary central nervous system tumors). The most common cause of LC is metastatic breast cancer (cancer that has spread from the breasts to other parts of the body). This is followed by lung cancer (particularly a type called small cell lung carcer) and then melanoma (a severe form of skin cancer).
Risk Factors and Frequency for Leptomeningeal Carcinomatosis
Every year in the United States, around 110,000 new cases of Leptomeningeal Carcinomatosis (LC), a type of cancer, are identified. However, real numbers may be higher because LC often goes undetected in standard medical examinations. The occurrence of LC varies between different cancer types. For example, it is found in 5% to 8% of breast cancer patients, 9% to 25% of those with lung cancer, and in up to 30% of people with melanomas, a type of skin cancer. Some research reports rates of 6% to 18% for melanomas. Moreover, the rate of LC is increasing. This is because people are likely to live longer after a cancer diagnosis due to better treatments and diagnostic procedures. However, the longer someone lives with systemic cancer (cancer that’s spread throughout the body), the greater the chance of LC developing. Usually, LC is diagnosed between 1.2 and 2 years after the detection of a solid tumor, but for blood cancers, this period is usually around 11 months.
Signs and Symptoms of Leptomeningeal Carcinomatosis
When a person with metastatic cancer gets sick, the signs and symptoms might not be specific and might not be immediately associable with their condition. The symptoms may vary, and some people may even have no symptoms at all when they’re first diagnosed. The symptoms that do appear often provide clues about where the cancer has spread in the body.
A variety of symptoms have been reported, which can be listed as follows:
- Cerebral symptoms: These can include headaches, confusion, cognitive impairment (problems with thought processes), psychiatric disorders, and seizures.
- Posterior fossa symptoms: This refers to symptoms linked to deficits in certain cranial nerves. They might include double vision, facial weakness, hearing loss, and problems with balance and coordination (ataxia).
- Vascular symptoms: These can include symptoms of reduced blood flow to certain areas of the body (ischemia) or even tissue death from lack of blood flow (infarction).
- Spinal cord symptoms: They might include weakness in the limbs, loss of sensation along certain nerve pathways (dermatomal sensory loss), nerve pain (radicular pain), and problems with bladder and bowel function.
- Inflammatory reactions: Tumor cells can cause inflammation and disrupt the flow of cerebrospinal fluid (CSF), leading to a condition called hydrocephalus. This can present as nausea, vomiting, headaches that change depending on body position, and excessive sleepiness (somnolence).
Testing for Leptomeningeal Carcinomatosis
Diagnosing leptomeningeal carcinomatosis (LC), a type of cancer, can be challenging due to the limits of current diagnostic methods. The first step usually involves having an advanced MRI scan of the brain and spine, a method that can detect LC with a reliability ranging from 70% to 100%. This MRI scan helps doctors look for changes in the protective covering of your brain and spinal cord, presence of tumors, and abnormalities in the fluid-filled spaces of your brain. Another sign of LC is an abnormal enhancement of nerve roots in the spinal cord.
If it is safe for the patient, the next step often involves a procedure called a lumbar puncture (LP), which is where a small sample of the fluid that surrounds your brain and spine – known as cerebrospinal fluid (CSF) – is taken for testing. In LC, these tests usually show a slight increase in white blood cells, a decrease in glucose levels (usually less than 60 mg/dL), and an increase in protein levels (greater than 45 mg/dL). As a safety measure, if glucose levels are very low, your doctor might want to rule out any infectious diseases.
In some cases, the pressure of the CSF might be too high, and there can be issues with the test giving false negative results. To reduce this problem, doctors might take a large volume of CSF for testing (10 mL), avoid unnecessary storing of the sample, and/or obtain CSF from certain parts of the brain or spinal cord where LC is known to affect. If the first LPC test does not confirm LC but the symptoms suggest otherwise, your doctor may decide to perform additional LPC tests.
Other ways to assist in diagnosing LC include testing for specific proteins made by tumors such as CEA, alpha-fetoprotein, and beta-human chorionic gonadotropin. However, this method is only considered if all other tests are negative because it does not consistently help with diagnosing LC. High volumes of a substance called VEGF could be another clue, but more research is needed on this.
Recently, a new method involving testing for fragments of tumor DNA in CSF is being explored. This method can detect specific changes in our DNA that are associated with some cancers. Although this method shows promise, it isn’t widely used yet.
In rare cases, specific scans may be used to look at how the CSF flows around your brain and spine. If there’s no active disease elsewhere in the body, doctors may perform additional tests to gain a better understanding of the patient’s condition and help select the best treatment plan.
Treatment Options for Leptomeningeal Carcinomatosis
Despite advancements in medical therapy, the prognosis for Leptomeningeal Carcinomatosis (LC), a type of cancer that spreads to the layers covering the brain and spinal cord, remains quite poor. There aren’t many high-level research studies available that help in determining the best treatment. As a result, the current treatment methods are based on less robust studies or the opinions of experienced doctors.
Currently, the treatment focuses on improving nerve-related symptoms, enhancing quality of life, and extending survival as far as possible while minimizing any harmful side effects. Typically, radiation therapy is used to treat the larger or problematic areas of the body. Intrathecal chemotherapy, which is a method of injecting anti-cancer drugs directly into the spinal canal, usually follows radiation. Cerebrospinal fluid (CSF) flow obstruction, a condition where the fluid that surrounds the brain and spinal cord doesn’t flow properly, is often relieved by surgical procedures. However, surgery generally plays a very small role in managing LC. Treatment for the primary cancer that caused LC could also be part of the treatment plan to increase lifespan.
Additionally, palliative care and supportive treatments are given as required. These might include antidepressants for mood disorders, anxiolytics for anxiety, opioids and non-opioids for pain management, and psychostimulants to improve energy and attention. It’s important to remember that these treatments are provided alongside efforts to treat the cancer itself.
What else can Leptomeningeal Carcinomatosis be?
Patients can experience a range of symptoms, and it’s important to think about other possible medical explanations. These could include things like infection, immune system disorders, blood vessel diseases, side effects from cancer treatment, rare conditions related to cancer, and brain disorders often seen in critically ill patients. The potential diagnoses could include, but aren’t limited to:
- Brain abscess (a pocket of infection in the brain)
- Brain metastasis (cancer that has spread to the brain)
- Chemical meningitis due to chemotherapy given into the spinal fluid
- Cord compression (pressure on the spinal cord)
- Meningitis and encephalitis (inflammations of the brain and spinal cord)
- Sarcoidosis (a disease that causes cells to group together in organs)
- Steroid myopathy (muscle weakness from steroid use)
- Stroke (a blocked or burst blood vessel in the brain)
- Toxic metabolic encephalopathy (a brain disorder due to serious illness)
Surgical Treatment of Leptomeningeal Carcinomatosis
The role of surgeries in treating this illness is small. To relieve symptoms of a condition known as hydrocephalus (a buildup of fluid in the brain), a doctor might insert a ventriculoperitoneal (VP) shunt – a device that can drain excess fluid from the brain. For giving chemotherapy directly into the brain, intraventricular catheters (tubes put into a ventricle in the brain to distribute medicine) might be used. In rare cases, if there’s a large disease presence in the central nervous system (CNS – brain and spinal cord), or if the primary cause of the illness isn’t yet known, a biopsy (removal of a small tissue sample for testing) or surgery may be necessary. But, surgeries are not known to improve chances of survival with this illness.
There are potential side effects for these treatments. These can include infection, displacement of the shunt (the device moving from its original position), and failure of the catheter (the tube not working properly).
What to expect with Leptomeningeal Carcinomatosis
For individuals with LC, the typical survival time from diagnosis to death is about 4 to 6 weeks with no treatment, which can be lengthened to about 2 to 4 months with treatment. Patients diagnosed with breast cancer have a more positive outlook. Their typical survival period is between 5 to 7 months – this is longer compared to illnesses like melanoma and lung cancer where the normal survival rate is about 4 months.
Certain factors can increase the chances for a better prognosis. These include a KPS score over 70 (KPS stands for Karnofsky Performance Status, a measure of how well a patient can carry out everyday tasks), normal flow of CSF (Cerebrospinal Fluid – the fluid found in your brain and spinal cord), not having major neurological deficits, being actively treated, having a primary cancer that is sensitive to chemotherapy, and having a CSF protein level of less than 50 mg/dL at time of diagnosis.
On the flip side, there are also factors that suggest a poor prognosis. According to the US National Comprehensive Cancer Network, these include a KPS score below 60, a high burden of disease within the central nervous system (CNS, which includes the brain and the spinal cord), extensive disease spread throughout the body with few treatment options, severe impairment of neurological functions, and encephalopathy, which is a term for brain diseases that alter brain function or structure.
Possible Complications When Diagnosed with Leptomeningeal Carcinomatosis
Leptomeningeal carcinomatosis is a condition that happens due to the spread of cancer, and it’s typically seen as a complication of that spread. Many of the complications linked to it come as a result of treatment choices. Those can include a type of meningitis that’s not caused by infection, damage to bone marrow that happens because of chemotherapy applied directly in brain’s ventricles, infections related to the catheter, malpositioning of the catheter placed in the brain’s ventricles, blockage of the catheter, changes in the brain’s white matter, exposure to the Ommaya reservoir (a device used to give medications to the fluid-filled spaces in the brain), and spinal cord damage due to chemotherapy.
Common Complications:
- A type of meningitis that’s not caused by infection
- Damage to bone marrow from chemotherapy
- Infections related to the catheter
- Incorrect placement of the catheter in the brain’s ventricles
- Catheter blockage
- Changes in the brain’s white matter
- Exposure to the Ommaya reservoir
- Spinal cord damage from chemotherapy
Preventing Leptomeningeal Carcinomatosis
Patients are advised to consult a cancer doctor who is an expert in leptomeningeal metastatic disease. Leptomeningeal metastasis is a type of cancer that spreads to the layers of tissue covering the brain and spinal cord. Despite the treatment options being somewhat limited, the healthcare team will provide information about what’s available and prepare both the patient and their families for potential difficult outcomes.