What is Leukemia?
Leukemia is a disease defined by the production of unusual white blood cells abnormally. This disease can be primary – where it starts from the bone marrow where blood cells are formed – or secondary, caused by conditions like cancer. Leukemia is categorized into four main types: acute myeloid leukemia, chronic myeloid leukemia, acute lymphoblastic leukemia, and chronic lymphocytic leukemia. Each of these types is named after the specific white blood cells affected and the speed of disease progression.
In addition, there are less common types of leukemia that develop from mature white blood cells such as B-cell and T-cell leukemias, and NK cell-related leukemias, among others. With the development of improved sequencing technologies and the identification of various disease markers, the classification of leukemia has undergone changes since 2016.
According to GLOBOCAN, a global cancer observatory, there were nearly 475,000 cases of leukemia recorded globally, with close to 68,000 cases in North America. The average rate is around 11 cases per 100,000 people.
Certain genetic conditions (like Down syndrome) or environmental factors (like exposure to radiation or some chemicals) have been associated with higher risk of developing leukemia. Other risk factors include smoking, a history of chemotherapy, or certain viral infections. Symptoms can be vague and include fever, tiredness, weight loss, bone pain, bruising, or bleeding. Doctors generally use a bone marrow biopsy to confirm the diagnosis of leukemia – this helps them to decide on the most appropriate treatment, which could include chemotherapy or stem cell transplantation.
The major types of leukemia are distinguished partly by the number of immature or dysfunctional cells, referred to as ‘blasts’. Acute leukemia involves more than 20% blasts and symptoms develop quickly, while chronic leukemia involves less than 20% blasts and symptoms appear more slowly. In some cases, chronic leukemia can transform into an acute phase, which is marked by a significantly higher number of blasts.
The four major types of leukemia include acute lymphoblastic leukemia, acute myelogenous leukemia, chronic lymphocytic leukemia, and chronic myelogenous leukemia. Acute lymphoblastic leukemia is most common in children but also affects adults. Acute myelogenous leukemia is more common and often more aggressive in adults. Chronic lymphocytic leukemia usually affects older adults and is generally slow-progressing. Chronic myelogenous leukemia involves a genetic mutation that leads to the overproduction of certain types of white blood cells. The treatment and prognosis vary depending on the specific type of leukemia.
What Causes Leukemia?
Leukemia, a type of blood cancer, can develop due to a combination of genetic and environmental factors.
Being exposed to a type of radiation called ionizing radiation can increase the chances of developing different types of leukemia. Coming into contact with a chemical called benzene is also a risk for adults, especially for a type of leukemia known as AML (acute myeloid leukemia).
If you have had chemotherapy treatments in the past, especially ones that use drugs known as alkylating agents or topoisomerase II inhibitors, you have a higher risk of getting acute leukemia later. Also, if you have had any blood cancer before, you’re at a higher risk of developing a different type of leukemia afterwards.
Certain viral infections, like the human T-cell leukemia virus and Epstein Barr virus, are linked with a subtype of leukemia called ALL (acute lymphoblastic leukemia). Furthermore, having certain genetic conditions (such as Down syndrome, Fanconi anemia, Bloom syndrome, or Li-Fraumeni syndrome) can raise your chances of developing both AML and ALL.
Risk Factors and Frequency for Leukemia
GLOBOCAN is a global research institute which tracks trends in cancer around the world. They’ve reported a global number of 474,519 cases, 67,784 of which are in North America. The average rates are around 11 cases per every 100,000 people, and about 3.2 out of every case results in death. Certain kinds of leukemia, such as ALL and AML, are seen commonly in both children and adults, whereas CML and CLL are more frequently found in older populations.
According to data from the Surveillance, Epidemiology, and End Results database, it’s anticipated that there will be approximately 61,090 new cases of leukemia in 2021. This would account for about 3.2% of all new cancer cases, making leukemia the 10th most common cancer in the United States. An estimated 23,660 deaths could result, making up about 3.9% of all cancer deaths. Since 2006, cases of leukemia have been increasing by an average of 0.6% per year, but death rates have been decreasing by an average of 1.5% per year.
Signs and Symptoms of Leukemia
Acute leukemia, a type of blood cancer that develops quickly, can present itself through a number of symptoms, which, while not specific, are usually common. These can include fever, fatigue, and bleeding. Some people may show signs like an enlarged liver or spleen, swollen lymph nodes, or musculoskeletal symptoms, especially in the spine and long bones. Adults might particularly struggle with anemia-related symptoms like shortness of breath or symptoms connected to low platelet count such as bruising easily or bleeding more than normal. In a type of acute leukemia called acute promyelocytic leukemia, symptoms may include bleeding in mucous membranes like gums, nose, or heavy menstrual bleeding.
Chronic leukemia, a slower-developing type of blood cancer, mostly occurs in adults. Quite often, many individuals with this type of cancer do not show any symptoms and only get diagnosed when a high white blood cell count is found during a routine blood test done for other reasons. Some people may show signs of an enlarged liver or spleen and swollen lymph nodes, while others might display symptoms of bleeding and bruising, although these are less common than in acute leukemia.
Testing for Leukemia
Diagnosing leukemia, a cancer affecting the blood, involves several tests. Initially, your doctor might perform a complete blood count, an overall health check through a comprehensive metabolic panel, check your liver’s functionality (liver function tests), and measure how well your blood clots (coagulation panel). These tests are usually followed by a detailed examination of your blood cells under a microscope and taking a small sample of your bone marrow for testing.
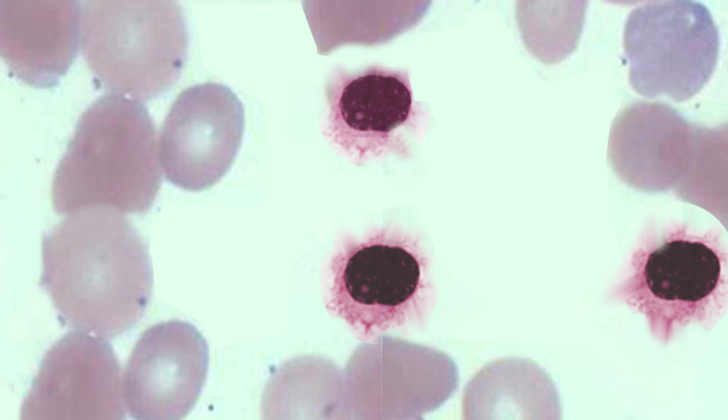
In some rare cases, leukemia can be diagnosed by looking at the cell structures alone. For instance, a type of leukemia called Acute Myeloid Leukemia (AML) is associated with a special structure called Auer rods present inside the cells. Auer rods look like red-staining, needle-like bodies spotted inside the specific type of cells called myeloblasts. However, in most instances, to differentiate between various forms of leukemia, a more detailed evaluation involving flow cytometry (a technique used to measure physical and chemical characteristics of cells), cytogenetics (study of chromosomes), and FISH testing (a method that maps the genetic material in the cells) is necessary.
For diagnosing acute types of leukemia, a bone marrow aspiration and biopsy are often essential, which involves removing and examining a small amount of bone marrow for disease. But for types of leukemia that progress slowly, termed chronic leukemias, a detailed examination of the blood itself is often enough. For instance, Chronic Myeloid Leukemia (CML) can be diagnosed by looking for a specific kind of protein fusion in the blood using a FISH analysis. Chronic Lymphocytic Leukaemia (CLL), on the other hand, can be diagnosed by looking for a specific type of B-cells (immune cells) in a peripheral blood using flow cytometry.
Treatment Options for Leukemia
If you or a loved one have leukemia, a doctor who specializes in blood disorders and cancer (a hematologist-oncologist) will guide treatment. The type of treatment used can vary a quite bit depending on the specifics of the leukemia and the person who has it, such as their age and overall health.
Specifically for a subtype of leukemia called Acute Myeloid Leukemia (AML), there is a type called Acute Promyelocytic Leukemia (APL), which requires a different treatment compared to regular AML. APL patients often present with symptoms such as unusual bleeding, coagulation (blood clotting) abnormalities, and specific blood test results. Treatment for APL begins with a specific type of medication called ATRA (all-trans-retinoic acid), which helps immature blood cells turn into mature ones, but can cause a reaction called differentiation syndrome. This syndrome can mimic a serious infection, causing fever, breathing difficulties, and swelling, among other symptoms. If APL is suspected, treatment with ATRA starts as soon as possible, without waiting for test results.
Further treatment for APL depends on whether the patient is at low, intermediate, or high risk, based on their white blood cell count and other factors. Each group receives slightly different treatments and may also receive other medications to manage symptoms and side effects.
For regular AML, the most common therapy is the ‘7+3’ regimen, which includes a 7-day course of a medication named cytarabine and a 3-day course of either daunorubicin or idarubicin. The actual treatment plan for each individual will be further refined based on molecular tests.
A certain type of leukemia referred to as ALL is classified into B or T lymphocyte variants based on the origin of the cancerous cells. The treatment regimen will depend on the presence or absence of a specific marker identified as the Ph chromosome. Depending on this status, variations of therapy can include different combinations of chemotherapy and other medications known as tyrosine kinase inhibitors.
Another type of leukemia is Chronic Myeloid Leukemia (CML). Unlike most other cancers, has seen significant success with targeted therapy that specifically targets the unique mutation found in CML. This has reduced the need for harsh chemotherapy, unless it has progressed to a more serious phase. The degree of risk poses by CML to each patient can be assessed with specialized scoring systems.
Chronic Lymphocytic Leukemia (CLL) tends to progress more slowly than other leukemias, and doesn’t always immediately require treatment. The need for treatment is based on several factors like the pace at which the leukemia is progressing and the patient’s symptoms. Once treatment commences, the guidelines are led by the knowledge of specific genetic markers and their implications. The treatment approach can range from chemotherapy for patients with a good prognosis to the use of targeted therapy for high-risk patients.
Despite the fact that chronic leukemias typically progress slowly, in rare cases, some people with CLL may suddenly develop fast-growing lymph nodes or changes in their condition that require aggressive treatment. In these cases, a biopsy (a procedure to take a sample of the swollen lymph node or bone marrow) may be done to check if the CLL has transformed into a different type of more aggressive cancer.
What else can Leukemia be?
Leukemia has a wide range of symptoms which can seem like other conditions. This makes it critical to rule out other causes that can lead to similar symptoms. These may include infections, reactions to drugs, lack of certain vitamins or nutrients, and other disorders affecting the blood cells.
When a check-up shows irregularities in the blood count, the following reasons should be considered:
- Vitamin B12 and folate deficiencies
- Lack of Copper
- Viral infections like HIV, cytomegalovirus, or Epstein-Barr virus
- Usage of certain drugs, such as chemotherapy medicines, valproic acid, ganciclovir, or mycophenolate mofetil
- Autoimmune conditions like systemic lupus erythematosus
What to expect with Leukemia
Survival rates for patients with leukemia can differ greatly, based on various factors. These factors include the specific type of leukemia, the genetic makeup of the leukemia cells, the age of the patient, and any other existing medical conditions. On a positive note, advancements in treatments have significantly improved the long-term survival rates – the cancer survival rate over five years has increased from 33% in 1975 to about 59% in 2005.
Possible Complications When Diagnosed with Leukemia
Tumor Lysis Syndrome (TLS) is an unexpected complication that can arise during chemotherapy. Essentially, it occurs when cancerous cells are killed off very rapidly, leading to an influx of cellular material within the bloodstream. This abrupt surge can overtax the kidneys and cause dangerous spikes in blood levels of potassium, phosphorus, and uric acid. To manage TLS, patients require continuous hydration, regular blood tests, and specific medicines, like allopurinol and rasburicase, to manage high uric acid levels. High potassium levels and low calcium levels can also potentially harm the heart and require immediate medical correction.
Disseminated Intravascular Coagulation (DIC) is a possible complication related to leukemia that messes with the proteins responsible for blood clotting. This issue can lead to both clot formation and bleeding. DIC is seen most often with a type of leukemia called acute promyelocytic leukemia but can develop with other leukemia subtypes as well. Patients with DIC need to be monitored closely with blood tests and often need fibrinogen (a blood clotting protein) replacement using cryoprecipitate (a blood product).
Individuals with leukemia can face a heightened risk of dangerous infections because of their compromised immune systems; this immunosuppression can be a result of chemotherapy, stem cell transplantation, or leukemia itself. Whenever a patient with weakened immunity develops a fever alongside a low neutrophil count (neutropenia), immediate checks to identify any possible infection source should be performed and treatment with antibiotics that cover a wide range of bacteria should be started.
Finally, it’s important to note that survivors of leukemia have a higher likelihood of developing other types of cancer. A long-term study on children who survived cancer found that roughly 5.6% developed some kind of cancer within 30 years of being diagnosed with leukemia. The median time to the development of this secondary cancer was found to be around nine years. Different subtypes of leukemia or lymphoma were the most common secondary cancers seen in childhood leukemia survivors.
Preventing Leukemia
Leukemia is a condition where your body produces abnormal white blood cells in the bone marrow and lymphatic tissues, which are vital parts of your immune system. This overproduction of abnormal white blood cells interferes with the creation of normal blood cells. These normal cells serve multiple roles such as fighting off infections, carrying oxygen throughout the body, and aiding in blood clotting. The abnormal cell production can happen quickly, resulting in acute leukemia, or more slowly, leading to chronic leukemia.
Common signs of leukemia include having infections repeatedly, losing weight, feeling very tired, having fevers, experiencing abdominal pain, and bleeding. There are numerous types of leukemia, and it’s really important that you see a hematologist – a doctor specializing in blood disorders – for further advice on how to treat this condition.