What is Leydig Cell Cancer?
Testicular cancer doesn’t happen very often, making up only 1% to 2% of all cancer diagnosed in men across the world. However, it’s the most common cancer found in men between the ages of 15 and 44. Testicular cancer can start in any of the cells in the testicles but usually falls into two main types. These are germ cell tumors, which make up about 95% of testicular cancer cases, and sex cord-stromal tumors, which make up about 5% in adults.
Out of the sex cord-stromal tumors, the most common kind are Leydig cell tumors. Leydig cells are usually found in the testicles, and they release testosterone when stimulated by a hormone called luteinizing hormone. Leydig cell tumors are mostly benign (not cancerous), with only 5% to 10% being cancerous (malignant). These tumors can show up in two age groups: just before puberty, and between the ages of 30 to 60. Because Leydig cells can produce hormones, the tumors can cause early puberty, sensitive breasts, or a condition called gynecomastia, which is when men develop enlarged breasts.
What Causes Leydig Cell Cancer?
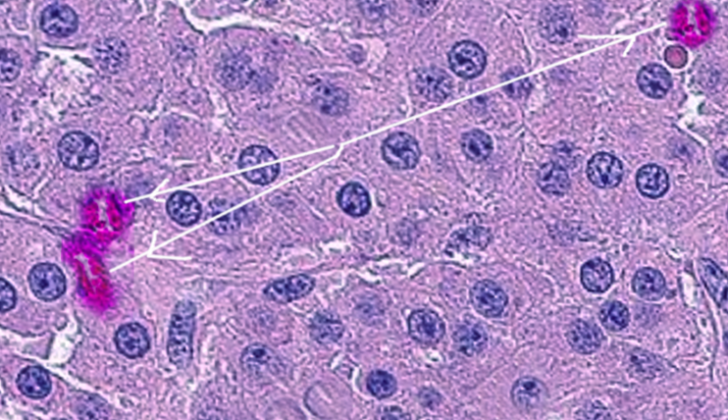
Leydig cell tumors come from Leydig cells. These cells are normally found packed between the tiny tubes in the testicles where sperm are made. Their main job is to produce testosterone – the male sex hormone, when they get a signal from another hormone called the luteinizing hormone.
Risk Factors and Frequency for Leydig Cell Cancer
Leydig cell tumors are considered a rare subtype of an uncommon tumor, making up only 1% to 3% of all testicular tumors removed each year. However, recent studies suggest that Leydig cell tumors might not be as rare as previously thought, with estimates indicating they represent 14% to 22% of all surgically removed testicular cancers. This change in incidence could be due to better ultrasound technology, which could detect smaller nodules that were previously overlooked.
Signs and Symptoms of Leydig Cell Cancer
Leydig cell tumors are a type of testicular cancer. The most common sign of these tumors, like other forms of testicular cancer, is a painless swelling in one of the testicles. This symptom is seen in about 50% of people who are eventually diagnosed with testicular cancer. When a doctor examines a patient, they will check both testicles, taking note of their size, firmness, and whether they can feel any lump. Sometimes, a benign condition called a hydrocele, where there is a fluid-filled swelling in the scrotum, can accompany a tumor and make finding a lump more difficult through a regular check-up.
Leydig cell tumors can sometimes cause symptoms because they secrete hormones like androgens and less commonly, estrogen. When these tumors occur in young boys, it can lead to precocious puberty. This condition would include early development of pubic hair and an abnormal increase in penis size and muscle growth for the child’s age.
In cases where the patients are men who have already gone through puberty, these elevated hormone levels usually don’t cause noticeable changes. However, the most common hormonal symptom for men with a Leydig cell tumor is gynecomastia, which is swelling of the breast tissues. Some men may also experience breast tenderness, loss of desire for sexual activity, difficulty with erections, the absence of sperm, infertility, or even a condition known as Cushing syndrome, which is caused by high levels of the hormone cortisol.
Testing for Leydig Cell Cancer
If a patient comes in with swelling in the testicles, a buildup of fluid around a testicle (a condition known as hydrocele), or any other unclear signs or symptoms related to the scrotum, a scrotal ultrasound should be done. This is a simple, inexpensive test that lets doctors see what’s happening inside the scrotum. A scrotal ultrasound should also be done if a patient is having difficulty getting pregnant, starts puberty earlier than expected, or develops enlarged male breasts (a condition known as gynecomastia), for no apparent reason. If blood tests show high levels of male or female hormones and there’s no known cause, a scrotal ultrasound can provide further information.
One thing an ultrasound might find is a Leydig cell tumor. This is an abnormal growth of cells in the testicles. On an ultrasound, this kind of tumor looks like a mass inside the testicle. It might look like another type of tumor called a germ cell tumor, which can be harmful. Because of this, any mass discovered within the testicles during the ultrasound should be taken seriously, as it could potentially be cancerous.
If the ultrasound reveals a lump or mass, additional blood tests for substances called tumor markers will be necessary. These are chemicals produced by tumor cells, and can include alpha-fetoprotein (AFP), quantitative beta-human chorionic gonadotropin (beta-HCG), and lactate dehydrogenase (LDH). If these markers indicate that the mass is likely to be cancerous, the patient might need further tests and might have to undergo a radical inguinal orchiectomy, which is a surgery to remove one or both testicles through an incision in the lower abdomen.
Treatment Options for Leydig Cell Cancer
The usual treatment for a lump within the testicle is a surgical procedure known as a radical inguinal orchiectomy, which involves the removal of the testicle through an incision in the groin. A biopsy to check for cancer isn’t typically performed before this surgery, unless there are unique circumstances such as only one testicle is present. Before the removal of the testicle, patients should receive advice about sperm banking, which is storing sperm for future use, such as fertility treatments.
It’s important that the removal of the testicle occurs through an incision made in the groin, rather than the lower abdomen or scrotum, to prevent any possible spread of cancer. In addition, the other testicle might also need to be biopsied if an ultrasound shows any abnormalities or if there’s a history of undescended testicle on that side.
There’s a type of testicular tumor called a Leydig cell tumour, which some experts suggest could be treated with a less radical surgery that spares the testicle if certain conditions are met. For this to happen, blood tests must all be normal, Leydig cell tumor is suspected based on symptoms (like breast enlargement, increased levels of testosterone or estrogen, infertility, etc.), the tumor is small and a frozen section (a rapid intraoperative pathological analysis) confirms it’s a Leydig cell tumor. However, Leydig cell tumors are so rare and resemble other types of testicular tumors so closely that most patients end up having the more common removal surgery.
Despite the fact that most Leydig cell tumors are benign (not cancerous) and the removal surgery is usually all the treatment needed, long-term monitoring is still recommended. There are no universally accepted guidelines for follow-up due to the rarity of this type of tumor, but it’s generally suggested that patients have regular check-ups, including various blood tests and imaging studies of the chest, abdomen, and pelvic area, every six months for at least the first two years post-diagnosis.
If a Leydig cell tumor does spread to other parts of the body, such as the lymph nodes in the back of the abdomen, liver, lungs, or bones, it generally does not respond well to chemotherapy or radiation. In this case, surgical removal of the affected areas is the only treatment option that may eliminate the disease.
What else can Leydig Cell Cancer be?
When a doctor is trying to figure out what might be causing a patient’s medical issues, they consider a variety of other conditions that might be responsible for the symptoms. This is called a “differential diagnosis.”
For example, if a patient comes in with gynecomastia (enlarged male breast tissue), the doctor might consider whether:
- The issue is a side effect of a certain drug (such as ACE inhibitors, marijuana, spironolactone, and others)
- The patient is obese
- The patient has an overactive thyroid (hyperthyroidism)
- The patient has liver disease
- The patient has a special genetic condition called Klinefelter syndrome
- An adrenal tumor is present
If a patient comes in with hypogonadism (a condition in which the body doesn’t produce enough of certain hormones), the doctor might consider whether:
- The patient has primary hypogonadism, which could be caused by Klinefelter syndrome or damage to the testicles from trauma, radiation, or infection
- The patient has secondary hypogonadism, which could be caused by a specific type of tumor (a prolactin-secreting pituitary tumor), a specific genetic disorder (Kallman syndrome), or another condition that results in low hormone production (hypogonadotropic hypogonadism)
Finally, if a doctor identifies an abnormal mass in the testicles during an ultrasound, they might consider whether:
- The mass is a germ cell tumor, which could be one of several types (seminoma, teratoma, yolk sac tumor, embryonal carcinoma, or choriocarcinoma)
- The mass is a non-germ cell tumor, which could be a Sertoli cell tumor, granulosa cell tumor, or gonadoblastoma
- The mass is an intratesticular hematoma (a collection of blood within the testicle)
What to expect with Leydig Cell Cancer
An orchiectomy, which is the surgical removal of one or both testicles, can effectively cure patients with benign Leydig cell tumors. Benign Leydig cell tumors are non-cancerous growths that begin in the testicles. After this surgery, the cancer-specific mortality rate for Leydig cell tumors is 2%, meaning 2% of patients pass away from this type of cancer. However, the 5-year survival rate, which is the percentage of people who live at least five years after the surgery, is more than 90%.
In contrast, malignant Leydig cell tumors, which are cancerous, can have diverse outcomes. The survival rate for patients with cancer spread (metastases) varies drastically, ranging from 2 months to 17 years, with an average of 2 years.
Intriguingly, even after the tumor is surgically removed, some men who initially suffered from hypogonadism may continue to experience Leydig cell dysfunction. Hypogonadism is a condition in which the body doesn’t produce enough testosterone – the hormone that plays a key role in masculine growth and development. As a result, 40% of these men may need to continue testosterone replacement therapy after the operation.
Possible Complications When Diagnosed with Leydig Cell Cancer
The complications that arise from the disease are mostly a result of a delay in diagnosis and treatment. The symptoms can extend to gynecomastia (enlarged breasts), infertility, hypogonadism (reduced functioning of the testes), or erectile dysfunction. If malignant Leydig cell tumors, a type of testicular cancer, are not treated promptly, they could spread to other parts of the body and potentially lead to death.
There’s an unfortunate trend in delays in diagnosing testicular cancer, with an average waiting period of 26 weeks before diagnosis. The delay from the patient’s side is often due to lack of awareness, feelings of embarrassment, or fear of the cancer or its implications. From a clinical perspective, physicians sometimes misinterpret testicles’ tumors as being infections, further delaying the diagnosis.
Common Complications and Causes of Delays:
- Enlarged breasts (gynecomastia)
- Infertility
- Reduced functioning of the testes (hypogonadism)
- Erectile dysfunction
- Potential spread of malignant Leydig cell tumors
- Potential death
- Patient’s lack of awareness
- Feelings of embarrassment
- Fear of cancer itself or its implications
- Physicians misdiagnosing testicle tumors as infections
Preventing Leydig Cell Cancer
For patients diagnosed with Leydig cell tumors, which are growths that occur in the testicle, it’s important to know that most of these tumors are not cancerous. Removing the affected testicle, a process called an orchiectomy, cures most cases. Finding and removing the tumor early can be crucial for maintaining fertility. This is because being exposed to too much estrogen for a long time, an effect of these tumors, can harm fertility.
It’s also crucial for patients to understand that after the tumor is removed, about 40% of men who had low levels of sex hormones might still need to use testosterone replacement therapy. This therapy is used to increase the levels of testosterone, a hormone that is important for male growth and masculine characteristics, to normal levels after surgery.