What is Liver Angiosarcoma?
Angiosarcoma is a severe and dangerous type of cancer. It involves the cells lining the blood or lymph vessels – tubes that carry fluids around our body. Usually, it’s found in the head and neck or the breast, but it can also be present in the liver. Though it’s relatively rare, when angiosarcoma occurs in the liver, it tends to be quite aggressive. Among the different types of rare liver tumors, this ‘primary hepatic angiosarcoma’ is the most commonly seen in adults.
What Causes Liver Angiosarcoma?
Around 75% of tumors occur with no clear reason. However, several factors are known to increase the risk of developing tumors. These include exposure to certain industrial materials like vinyl chloride, past use of a substance called colloidal thorium dioxide (Thorotrast), taking androgenic steroids, ingesting arsenic over a long period of time, and exposure to radium. Other risk factors include exposure to medicines like diethylstilbestrol, urethane, cyclophosphamide, and birth control pills. Liver angiosarcoma, a type of tumor, related to these environmental factors, can take 10 to 40 years to develop after exposure.
Vinyl chloride, used previously in making a type of plastic called polyvinyl chloride, can cause liver and kidney damage. This damage is due to a toxic byproduct called chloroethylene oxide, formed during the manufacturing process. After exposure to vinyl chloride, it typically takes around 20 years for a cancer to develop. These cancers often have changes or mutations in a gene called TP53.
Thorotrast was once used to improve the visibility in medical imaging but was soon discontinued due to its harmful effects, such as organ damage and even death. In the liver, Thorotrast is absorbed and stored by a specific type of immune cell called Kupffer cells, and it ends up stored in areas around the liver portal vein after cell death. This results in the scarring of surrounding areas and the fibrous capsule of the liver. Cancers caused by Thorotrast exposure often have changes or mutations in a gene called KRAS-2.
Finally, ingestion of arsenic over a long period initially results in a swollen liver, and can then lead to the development of fat accumulation in the liver, cell death, fibrosis (scarring), and cirrhosis (late stage of scarring).
Risk Factors and Frequency for Liver Angiosarcoma
Hepatic angiosarcoma, a type of liver cancer, is quite rare, making up only between 0.1%-2% of all primary liver cancers. Despite this, it’s still the third most common primary cancer found in the liver. This condition frequently occurs in older men, usually in their 60s or 70s. Men are affected more than women, with a ratio of 3-4 men for every woman. Interestingly, in children, girls tend to get this condition more than boys.
Signs and Symptoms of Liver Angiosarcoma
Hepatic angiosarcoma is a type of liver disease that often doesn’t have very specific symptoms. When symptoms do show up, they can include pain in the upper right side of the abdomen, weight loss, bloating, a yellowing of the skin and eyes known as jaundice, and fatigue. When examined, a doctor might notice the jaundice, fluid buildup in the abdomen (ascites), and an enlarged liver (hepatomegaly). In some cases, people might not show any symptoms at all, and the condition is only discovered when they’re getting scans or imaging for other reasons.
- Pain in the upper right side of the abdomen
- Weight loss
- Bloating
- Jaundice
- Fatigue
- Fluid buildup in the abdomen (ascites)
- Enlarged liver (hepatomegaly)
Testing for Liver Angiosarcoma
Diagnosing a type of liver cancer called hepatic angiosarcoma can be challenging. This is because the signs and symptoms are not easy to identify. In many cases, liver tumors are found by accident during abdominal imaging.
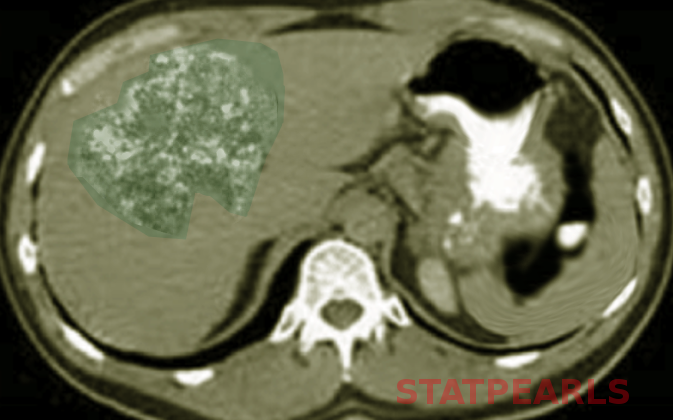
Medical imaging is a key part of identifying hepatic angiosarcoma. However, it’s not easy to tell it apart from other types of liver tumors on a scan because both have high amounts of blood vessels. Ultrasounds may show one or multiple nodules, or a single large mass in the liver, with differing appearances due to tissue death and internal bleeding in the lesions.
The most reliable method for diagnosing this type of liver cancer is contrast-enhanced computed tomography, more commonly known as a CT scan. In a CT scan, lesions appear less dense than normal with multiple patterns of enhancement. After the contrast is introduced, the lesions become the same density as regular liver tissue. Magnetic resonance imaging, or MRI, can also be employed to identify hepatic angiosarcoma, as it can reflect the bleeding, inconsistency, and high numbers of blood vessels within the lesions.
Blood tests in patients with hepatic angiosarcoma will likely show elevated liver enzymes, such as alanine transaminase and aspartate transaminase. There may also be a lower than normal count of platelets (cells that stop bleeding) and red blood cells (cells that carry oxygen), as the normal liver tissue is replaced by the tumor. The levels of certain proteins produced by tumors, known as tumor markers(AF, CEA, CA19-9, and CA125), are typically in the normal range or only slightly elevated.
To confirm a diagnosis of hepatic angiosarcoma, doctors will likely use a combination of imaging results and an examination of tissue (histological interpretation). However, it’s important for patients to understand that even when detected, this type of tumor tends to grow fast and may result in poor outcomes.
Treatment Options for Liver Angiosarcoma
Primary hepatic angiosarcoma is a severe type of liver cancer that is generally aggressive and, unfortunately, results in a poor prognosis, particularly when it’s not possible to operate. Most patients pass away within six months of diagnosis, and only approximately 3% live more than two years, even with medical intervention.
The most effective treatment in cases of single tumors is to surgically remove part or all of the liver, known as hepatic resection. However, when the cancer has spread to other parts of the body, which is referred to as metastasis, this surgery may not be possible. Liver transplants are not generally recommended for these patients because the cancer is likely to reappear and progress rapidly. The average survival time post-transplant is less than seven months.
Currently, no consistently effective chemotherapy treatment has been established. However, there has been a single report that suggested some effectiveness of combining chemotherapy drugs – 5-FU-carboplatin with either doxorubicin or ifosfamide, for patients with inoperable liver angiosarcoma that has spread to other parts of the body.
A study involving a large number of patients revealed that surgical treatment greatly improved the survival rate for patients in the early stage of liver angiosarcoma. These surgical patients also had a better prognosis compared to those who received non-surgical treatments.
Transcatheter Arterial Chemoembolization (TACE), a procedure that combines chemotherapy and a procedure to block the liver’s blood supply, can also be used for symptom relief or to control bleeding.
Unfortunately, the lack of clear-cut guidelines for optimal treatment methods involving surgery, chemotherapy, and radiation poses a challenge, as the results vary greatly from one study to another.
What else can Liver Angiosarcoma be?
When a doctor is trying to diagnose a liver condition known as hepatic angiosarcoma, there are several other conditions that may have similar symptoms and thus need to be ruled out. These include:
- Inflammatory disorders of the liver
- Benign vascular diseases of the liver
- Kaposi sarcoma
- Liver metastasis from angiosarcoma that started in other organs
- Epithelioid hemangioendothelioma
- Hepatocellular carcinoma (a type of liver cancer)
- Fibrosarcoma (a type of soft tissue tumor)
What to expect with Liver Angiosarcoma
Hepatic angiosarcoma is a fast-growing and deadly tumor. Most patients unfortunately pass away within six months of diagnosis due to liver failure or heavy bleeding. Even with surgical removal of the tumor, many patients do not survive beyond a year. If the tumor ruptures, a patient’s survival can be less than a month.
Possible Complications When Diagnosed with Liver Angiosarcoma
Liver angiosarcoma is a deadly type of cancer that can lead to death within six months due to liver failure or severe bleeding. The tumor may rupture causing hemoperitoneum, a condition in which blood fills the abdomen. If this happens, a procedure called transarterial embolization is often performed first to stabilize the patient and stop the bleeding. However, due to the rarity of this cancer, there are no solid guidelines on how to treat sudden bleeding from a liver angiosarcoma. Some patients with this type of cancer have been reported to show symptoms of disseminated intravascular coagulation, a serious condition that affects the blood’s ability to clot.
Factors to Consider:
- Quickly fatal, possible death within six months.
- Possible causes of death include liver failure or severe bleeding.
- Tumor might rupture, leading to blood filling the abdomen (hemoperitoneum).
- Transarterial embolization might be the first step to control the bleed.
- Recommendations for treating acute bleeding from liver angiosarcoma are not definite due the rarity of the cancer.
- Possible development of disseminated intravascular coagulation, a serious blood clotting issue.
Preventing Liver Angiosarcoma
Diagnosing hepatic angiosarcoma, a type of liver cancer, can be quite challenging in the early stages because the symptoms are not easy to recognize. Unfortunately, this cancer progresses rapidly and is resistant to common cancer treatments such as chemotherapy and radiation therapy. This, along with the high chance of the cancer coming back, means the outlook for patients is often poor.
The most effective treatment we know of so far is surgical resection, which involves removing the cancerous part of the liver. However, because this type of cancer is so rare, there is currently no established treatment plan.
It is known that exposure to certain environmental and chemical substances can cause this disease, as mentioned before. It’s important to discuss any known exposures with your doctor, as this can help them determine the best course of treatment for you.