What is Liver Cancer?
Hepatocellular carcinoma, or primary liver cancer, is the most common type of liver cancer in the United States. It’s present in three out of four cases of all primary and secondary liver cancers. The number of new cases and deaths from this type of cancer are on the rise. This increase is closely linked to chronic liver disease or cirrhosis, a condition where the liver gets progressively damaged, which is common in certain geographical locations.
What Causes Liver Cancer?
Liver cancer, specifically Hepatocellular carcinoma, often develops from chronic liver disease that can be caused by multiple risk factors. It’s particularly linked to long-term infections with hepatitis B and C viruses. Having these chronic hepatitis infections alongside other risk factors such as being infected with the hepatitis D virus, consuming alcohol, smoking cigarettes, can increase a person’s risk of getting liver cancer.
Patients who have chronic hepatitis for whatever reason—including conditions such as hemochromatosis (an iron overload disorder) or alpha-1 antitrypsin deficiency (a disorder that can cause lung and liver disease)—or who have a type of liver disease where the cause isn’t known (cryptogenic cirrhosis) also have a higher risk of developing liver cancer.
Exposure to certain environmental toxins such as aflatoxin (a harmful substance made by a type of fungus), contaminated water with blue-green algae toxins, and betel nut (a type of nut that’s commonly chewed in some cultures) can play a role in causing liver cancer.
Overuse of alcohol and metabolic syndrome (a group of conditions including high blood pressure, high blood sugar, excess body fat) have been linked to liver cancer. These conditions can cause ongoing liver damage that leads to fat build-up in the liver (steatosis), inflammation and damage of the liver (steatohepatitis), scarring of the liver (cirrhosis), and, eventually, liver cancer.
On the brighter side, certain factors have been linked to a lower risk of liver cancer. These protective factors include taking cholesterol-lowering drugs called statins and drinking coffee. Treatment of chronic hepatitis, managing metabolic syndrome, reducing iron levels, and stopping drinking alcohol can help prevent cirrhosis and, in turn, reduce the risk of developing liver cancer.
Vaccination against hepatitis B virus and screening for hepatitis C virus can also reduce the incidence of liver cancer worldwide. Professionals usually recommend regular check-ups for those who are at high risk of developing liver cancer. These liver cancer check-ups often include ultrasound scans and blood tests for a substance called alpha-fetoprotein, which can be a sign of liver cancer, every 6 to 12 months. The exact guidelines for these liver cancer screenings may vary among different medical societies or institutions.
Risk Factors and Frequency for Liver Cancer
Hepatocellular carcinoma, a type of liver cancer, is the fifth most common cancer and the second leading cause of cancer deaths globally. This form of cancer mainly results from chronic viral B (HBV) and C hepatitis (HCV) infections. In the United States, cancer data shows that the incidence rate of hepatocellular carcinoma has been increasing by 3.1% each year. Men are more likely to be affected, with 11.5 cases per 100,000 compared to 3.9 cases in women. The death rates due to this cancer have also been increasing for both genders, with males showing a 2.8% increase and females a 3.4% increase every year. Generally, hepatocellular carcinoma often affects older people after a long period of chronic liver disease.
- The occurrence and fatality rates of hepatocellular carcinoma can vary depending on the region and the race/ethnicity of the individual, mainly due to different exposure to risk factors.
- Though HBV infections are more widespread globally, HCV is responsible for 30% of hepatocellular carcinoma cases in the United States.
- Individuals born in the United States between 1945 and 1965 show a five times higher prevalence of HCV, which increases their risk of dying from liver cancer.
Signs and Symptoms of Liver Cancer
Hepatocellular carcinoma, also known as liver cancer, often does not show symptoms to start. But when symptoms do appear, they are often related to chronic liver disease. People may feel discomfort or swelling in the upper stomach area, lose weight, experience fevers, have a poor appetite, feel full quickly, and may have diarrhea. If someone with liver disease suddenly develops conditions like fluid buildup in the abdomen (ascites), confusion (encephalopathy), yellowing of skin or eyes (jaundice), or vomiting blood (hematemesis), it could imply the presence of liver cancer. Rarely, liver cancer can present with unusual symptoms due to a condition called paraneoplastic syndrome, which includes low blood sugar (hypoglycemia), high red blood cell count (erythrocytosis), high calcium levels in the blood (hypercalcemia), or severe watery diarrhea.
A physical check-up might show signs of long-term liver disease or cirrhosis, such as an enlarged liver (hepatomegaly), enlarged spleen (splenomegaly), fluid build-up in the abdomen (ascites), yellowing of skin or eyes (jaundice), or swollen veins in the abdomen (also known as the palm tree sign). These could indicate cirrhosis.
- Upper abdominal discomfort or swelling
- Weight loss
- Fever
- Poor appetite
- Feeling full quickly
- Diarrhea
- Signs of acute liver problems: ascites, encephalopathy, jaundice, or hematemesis
- Unusual symptoms due to paraneoplastic syndrome: hypoglycemia, erythrocytosis, hypercalcemia, severe watery diarrhea
- Signs of chronic liver disease or cirrhosis: hepatomegaly, splenomegaly, ascites, jaundice, swollen veins in the abdomen
Testing for Liver Cancer
If your doctor suspects or confirms liver cancer (hepatocellular carcinoma), you’ll need tests to further investigate the risk and severity. These tests will check for things like low albumin (protein levels in your blood), high bilirubin (a waste product the liver should remove), and low prothrombin (a protein needed for blood clotting). They’ll also evaluate the presence of ascites (fluid in the abdomen) and encephalopathy (brain dysfunction), in a grouping known as the Child-Pugh assessment scale.
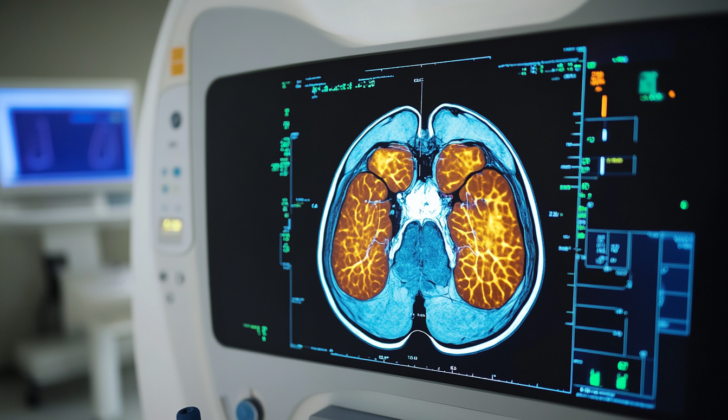
Medical professionals have developed guidelines for diagnosing solid liver lesions (abnormal tissue) based on their size. Regular ultrasound checkups often help identify people at high risk of liver cancer, and these findings are then further examined by something known as dynamic contrast-enhanced MRI (detailed images of the liver using contrasts) or four-phase CT scan (special type of X-ray that provides more detail).
If certain characteristics that imply liver cancer are not seen on the MRI, your doctor will likely recommend regular ultrasounds every three months. When the risk of liver cancer is high, if the MRI or CT scan provide clear results with specific indicators, a biopsy (removal of a small amount of tissue for testing) won’t be needed. An AFP (Alfa-FetoProtein) test could be used to raise suspicions for liver cancer, especially if the level is above 500 mcg/L. There are other approved, but less commonly used, tumor marker tests which, together with the AFP, can mean there’s a 90% chance of liver cancer.
If the diagnosis still isn’t clear, a biopsy might be recommended. If liver cancer is diagnosed, then a CT scan will be needed to check if the cancer has spread (metastasis).
There are many ways to predict how liver cancer will progress, but no single system is considered the best. The Barcelona Clinic Liver Cancer system, which includes the Child-Pugh stage (A, B, or C) and the Okuda system, is commonly used. The Okuda system considers tumor size, presence of ascites, albumin and bilirubin levels. Patients are assigned points, leading to stages I, II, and III, each with linked survival rates.
The Barcelona system further breaks down stages into:
- Early stage (A): Asymptomatic (not showing symptoms) patients who can have radical therapies to remove the tumor
- Intermediate stage (B): Asymptomatic patients with many tumors may benefit from chemoembolization (chemo delivered directly to the tumor)
- Advanced stage (C): Patients with symptoms, the cancer has entered a blood vessel, and/or has spread beyond the liver can be treated with chemotherapy
- Terminal stage (D): The disease is at an advanced stage, and only palliative care (relief from symptoms) can be offered
Patients with very early (0) and early stage (A) liver cancer may undergo surgery or liver transplant with a cure rate of 30% and a survival rate of 40% to 70% over 5 years. Depending on the stage of the cancer (I, II or III), the survival rate after surgery varies. The Cancer of the Liver Italian Program (CLIP) score helps determine survival expectations for advanced disease by considering factors like tumor size, number, and spread, AFP levels, and portal vein thrombosis (a blood clot in the liver).
Treatment Options for Liver Cancer
Surgery is considered the most effective treatment for most people with liver cancer, otherwise known as hepatocellular carcinoma. However, nearly 70% of patients are not suitable candidates for surgery. For those who are, the options usually involve either removal of a part of the liver (resection) or a liver transplant. Surgery is typically only recommended to patients who are in the early stages of liver cancer and whose liver disease is not too advanced.
Patients suitable for a transplant must meet certain criteria, such as having a single tumor smaller than 5 cm or two to three tumors no larger than 3 cm. Wait times for a transplant can extend to several months, so doctors typically use other treatments like chemoembolization or radiofrequency ablation to manage the cancer in the meantime.
If surgery is not an option, other local treatments can be explored. One method is radiofrequency ablation, which can completely get rid of the cancer in a reported 80% of cases, provided the tumors are not too large. Alternatively, transarterial chemoembolization can be used, particularly for larger or multiple tumors. This procedure involves blocking the blood vessel that is feeding the cancer tissue, which effectively starves the cancer cells of oxygen and nutrients, causing them to die.
For advanced liver cancer that’s spread to other areas, a drug called Sorafenib might be recommended. This targeted therapy blocks certain proteins that cancer cells need to grow. Another similar drug, Regorafenib, might be used if Sorafenib is no longer effective.
As an alternative to these treatments, clinical trials are continuously seeking and testing new methods to combat hepatocellular carcinoma. These include innovative treatments like immunotherapy, with drugs such as nivolumab and durvalumab, and novel approaches using small molecule tyrosine kinase inhibitors like cabozantinib.
What else can Liver Cancer be?
There are many conditions that could affect the liver, each with their own unique characteristics. These include:
- Angiosarcoma
- Cirrhosis
- Cholangiocarcinoma
- Epithelioid hemangioendothelioma
- Embryonal sarcoma
- Hepatoblastoma
- Hepatocellular carcinoma
- Hemangiomas
- Hamartoma