What is Malignant Melanoma?
The number of people diagnosed with primary cutaneous melanoma, a type of skin cancer, has seen a consistent increase over the years and is the deadliest form of skin cancer. However, if it’s detected in the early stages, the survival rates for melanoma can be quite high, around 94%. From 2014 to 2018, the National Cancer Institute estimated that around 0.9 out of 100,000 people had melanoma that has spread to other parts of the body. It’s worth noting that melanomas found in mucosal tissues and the eyes typically have a worse outcome compared to other types.
In the past, melanoma was a very aggressive cancer that often didn’t respond well to conventional treatments like chemotherapy, radiation therapy, and early versions of targeted therapies. But recent developments in new combinations of targeted therapies and different types of immune-directed therapies have significantly improved both the quality of life and overall survival of patients with advanced melanoma.
Melanoma is different from other skin cancers because it can spread locally, regionally, and to distant parts of the body. The risk of it spreading is directly related to how deep the cancer has invaded the skin and whether the original cancer has broken down to form an ulcer. The early stages of cancer spread involve the cancer cells breaking away, forming new blood vessels, escaping into the bloodstream, spreading and settling in a new organ. Interestingly, here’s a curious fact: even patients who show no signs of cancer in their lymph nodes, and those with negative results in a sentinel lymph node biopsy test (a test to see if the cancer has spread to the nearest lymph nodes), can still later present with advanced disease. On a similar note, removing all the lymph nodes has not been shown to increase survival rates in patients with melanoma that has spread to the nodes. There have also been cases reported of melanoma being transferred from an organ donor to a recipient, even if the transplant happens years after the donor was diagnosed.
Typically, patients may notice an asymmetrical large skin lesion that may also itch, bleed, break down to form an ulcer, or develop additional lesions nearby. If the melanoma has spread to other parts of the body or started from a place other than the skin, patients may experience signs and symptoms related to the organ systems affected. Therefore, if a suspicious skin injury is noticed, a biopsy (sample taking) must be performed to confirm a melanoma diagnosis. The best type of biopsy to use is an excisional biopsy where the whole area is removed. Treatment of melanoma usually consists of wide local excision (surgery to remove the melanoma and some non-cancerous surrounding tissue), Mohs micrographic surgery (a specialized surgery to remove the cancer), digital amputations, or supplementary therapies, depending on the tumor’s location, depth, whether it’s ulcerated, if it has spread to the lymph nodes, and if it has metastasized (spread to other parts of the body).
What Causes Malignant Melanoma?
There are multiple factors that can lead to the development of malignant melanoma, a type of skin cancer:
Risk Factors and Frequency for Malignant Melanoma
Melanoma is the fifth most common cancer in both men and women, according to the NCI’s Surveillance, Epidemiology, and End Results (SEER) program. It’s predicted that in 2023, 97,610 new cases of melanoma will be diagnosed in the US, and there will be around 7,990 deaths related to melanoma.
Melanoma is triggered by a variety of influences, including environmental factors, genetics, and the immune system. A lot of melanoma research is devoted to kick-starting the immune system and learning more about the different signals that can lead to cancer. This has led to the creation of successful treatments targeting the immune system and specific gene pathways. Certain genes like CDKN2A, CDK4, and MC1R have been linked to an increased risk of melanoma.
Also associated with melanoma is a genetic disorder called xeroderma pigmentosum (XP). This condition prevents the body from properly fixing damage caused by UV rays, which consequently results in a high mutation rate and can lead to melanoma.

Signs and Symptoms of Malignant Melanoma
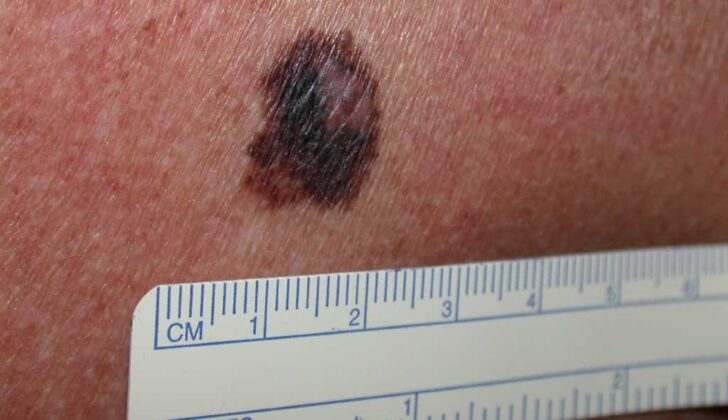
Early signs of melanoma, a type of skin cancer, can be remembered with the ABCDE rule. This is a simple way to spot changes in moles or skin growths:
- “A” stands for Asymmetry.
- “B” stands for Border. This refers to the edges of the mole, which may be irregular, ragged, notched, or blurred.
- “C” stands for Color. The color may be uneven or different shades.
- “D” stands for Diameter. The mole may be larger than 6 millimeters.
- “E” stands for Evolving. The size, shape, or color of the mole may change over time.
Dermoscopy, a special type of skin examination, can also be helpful to tell if a lesion is benign (non-cancerous) or malignant (cancerous). When melanoma is diagnosed, it’s categorized by stages based on guidelines from the American Joint Committee on Cancer (AJCC). The stage of the melanoma helps determine the treatment plan and potential outcome.
Melanomas may become itchy or start to bleed, form ulcers (sores), or grow new lesions near the original one. Patients with advanced melanoma or with melanoma that has spread to other parts of the body may have symptoms based on which organ systems are affected. It’s also crucial to check all lymph nodes as part of the examination, as melanoma can spread there.
Testing for Malignant Melanoma
For diagnosis of skin cancer, specifically melanoma, a thorough skin check under good lighting is absolutely essential. This check includes looking closely at any suspicious marks on the skin. This process can also include a special examination called a dermatoscopy, which provides a more detailed scrutiny of any odd-looking skin areas. This helps the doctor determine if the mark matches the known signs of melanoma, often summarized as the “ABCDE” rules. Nail inspections are also important because some melanomas can form under the nails and these tend to have a distinct set of features, which are summed up as the “ABCDEF” rules. Here, “F” stands for personal or family history of melanoma.
If there’s a suspicious skin spot, the next step is a biopsy, which is a test where part or all of the suspicious spot is removed for examination under a microscope. The full or partial removal, known as the excisional biopsy, is the first choice because melanoma straightforwardness directly relates to how deep it is in the skin. This biopsy will help determine the ‘stage’ of the melanoma. Staging is basically figuring out how far the melanoma has spread. Depending on the depth or stage of melanoma, the doctor may also advise further testing, like checking the closest lymph node (which is a small bean-shaped structure that helps to fight infections and disease) or potentially scheduling other imaging tests like x-rays and scans.
With regards to laboratory tests, your doctor may ask for tests such as a complete blood count, liver function tests, and something called a lactate dehydrogenase test. All these tests provide an overall picture of your health and might hint towards any potential melanoma spread.
If necessary, your doctor might also recommend imaging tests such as chest X-rays, brain scans (MRI), ultrasound, CT scans of the chest, abdomen or pelvis or something called a PET scan. These tests are to see if the melanoma has spread to other parts of the body.
Treatment Options for Malignant Melanoma
If a melanoma (a type of skin cancer) is caught early, which is the ideal scenario, doctors mostly opt for surgery to remove the cancerous tumor. They use a method called ‘wide local excision’, where not only is the tumor removed, but also some healthy tissue around it, to make sure that no cancer cells are left behind. When the biopsy shows that the cancer cells have spread close to or beyond the edges of the biopsy (positive or close margins), an additional surgery known as a sentinel lymph node biopsy may be performed if the tumor is bigger than a certain size. This helps understand if the cancer has spread to the lymph nodes.
For larger lesions where direct closing of the surgery wound is not possible, skin grafting or tissue transfers could be required as part of the reconstruction process.
In certain cases of ‘melanoma in situ’ (cancer that has not spread beyond the upper layer of the skin), a specialized surgical technique called Mohs micrographic surgery may be employed. For certain types of melanomas, such as those arising in unusual locations like under the nails (subungual), amputation of the affected digit may be needed. But, for melanoma in situ in such areas, surgeries preserving the digit could be an option.
The depth of the melanoma or the Breslow’s depth, a measure of how deep the melanoma has penetrated into the skin, is a crucial factor. Depending upon this depth and certain other features such as ulceration and lymph node involvement, additional treatments may be required after surgery.
Most health institutions currently prefer observation over completing lymph node dissection when lymph node involvement is noted. This decision is backed by research showing no significant difference in survival rates between these two approaches. However, there may be a slight improvement in disease-free survival at the expense of higher incidences of lymphedema (swelling due to damage to the lymphatic system).
Additional or adjuvant therapies could be decided based on the stage of melanoma and risk of disease recurrence. These usually include drugs like pembrolizumab, nivolumab, or dabrafenib/trametinib if a specific mutation (BRAF) is identified in the cancer cells. Also, radiation therapy could be considered depending on factors such as that location, size, and number of lymph nodes involved.
In advanced cases with borderline resectable disease, patients could potentially receive therapies before the surgery to increase the chances of successful surgical removal of the tumor. Interferon alfa is a medication, which is seldom used in these scenarios currently.
What else can Malignant Melanoma be?
When trying to diagnose malignant melanoma, a type of skin cancer, doctors also need to weigh out other conditions which have similar symptoms. These are:
- Atypical fibroxanthoma
- Pigmented basal cell carcinoma
- Blue nevus
- Epithelioid tumor
- Halo nevus
- Histiocytoid hemangioma
- Mycosis fungoides
- Pigmented spindle cell tumor
- Sebaceous carcinoma
- Dermatofibroma
- Seborrheic keratosis
- Cherry hemangioma
- Lentigo
- Subungual hematoma
By carefully going through these conditions, physicians can arrive at an accurate diagnosis of malignant melanoma.
What to expect with Malignant Melanoma
In the case of melanoma, a type of skin cancer, there are several factors which might negatively affect a patient’s chances of surviving the disease. These include having a thicker tumor, the presence of the tumor in nearby lymph nodes (known as stage III disease), a higher number of positive (cancerous) lymph nodes and the presence of the cancer in distant parts of the body (known as stage IV disease).
Other factors that contribute to a poorer prognosis include whether the tumor is located on the trunk or face (which are worse than if on extremities), and whether the tumor has signs of ulceration or regression (though this is a point of debate among doctors). Men are also found to be more at risk.
The stage of the disease at diagnosis plays a big role in patient’s survival rate. The stages of melanoma range from 0 to IV, and the 5–year survival rates reported for each stage are as follows:
- Stage 0: 99% to 100%
- Stage IA: 99%
- Stage IB: 97%
- Stage IIA: 94%
- Stage IIB: 87%
- Stage IIC: 82%
- Stage IIIA: 93%
- Stage IIIB: 83%
- Stage IIIC: 69%
- Stage IIID: 32%
- Stage IV: 34% to 52%
These statistics mean, for example, that patients diagnosed with Stage 0 melanoma have a 99% to 100% chance of surviving at least 5 years after being diagnosed.
Possible Complications When Diagnosed with Malignant Melanoma
Treating malignant melanoma typically involves a mix of surgery, in rare cases radiation therapy, adjunctive immunotherapy, or precise targeted therapies. These treatments have been shown to enhance survival rates and long-term health results for people living with melanoma, but they also come with some potential side effects.
Surgical complications can consist of bleeding, infections, nerve damage, and scar formation. Beyond the physical repercussions, the aftereffects of surgery can sometimes cause psychological issues, like stress and depression. In cases where lymph nodes are removed, it results in a heightened incidence of lymphedema, a condition of limb swelling due to lymph fluid accumulation.
A small group of patients who undergo radiation to the lymph node region, particularly in cases where there is vast involvement of lymph nodes, may experience radiation-related complications. These may encompass skin irritation, fatigue, higher probability of secondary cancers, and again, lymphedema.
Adjuvant treatments, such as immunotherapies and targeted therapies, have varying potential side effects that can make treatment more challenging. These include immunotherapy-related adverse events and targeted therapy-linked adverse events like fevers induced by medication, increased susceptibility to secondary cancers, fatigue, a higher risk of infections, and weakened immune systems.
All these prospective complications can negatively affect a patient’s quality of life as well as their ability to complete the treatment plan. In turn, this can result in a greater chance of cancer recurrence and lower survival rates. Hence, it is crucial to closely observe these side effects, carefully select appropriate treatments, and continuously monitor the patient.
Potential Side Effects:
- Bleeding
- Infections
- Nerve damage
- Scar formation
- Depression and Anxiety
- Lymphedema
- Skin irritation and fatigue from radiation
- Higher probability of secondary cancers
- Immunotherapy-related adverse events
- Fevers induced by medication
- Risk of infections
- Weakened immune systems (immunosuppression)
Preventing Malignant Melanoma
Patients should be informed and advised about crucial prevention strategies that can protect them from skin-related issues. These include:
* Protecting yourself from the sun – You can do this by wearing clothes that cover the skin and using sunscreen that has the right amount of SPF (Sun Protection Factor). SPF is a measure of how well a sunscreen will protect your skin from UVB rays, a type of sunlight that can cause sunburn and contributes to skin cancer.
* Avoiding exposure to sun during the middle of the day – The sun’s rays are strongest between 10 a.m. and 4 p.m., making this the most hazardous time for unprotected sun exposure.
* Not using tanning beds – Tanning beds emit UV rays that can be stronger than the sun and dramatically increase your risk of skin cancer.
* Scheduling yearly evaluations with a dermatologist – A dermatologist is a skin specialist who can identify suspicious spots and changes that may indicate skin conditions or diseases.
* Regularly checking your skin – Look for changes in the color, size or shape of moles, freckles or spots. If you notice anything unusual, get it checked out by a healthcare provider as soon as possible. This early detection can be key to successful treatment.