What is Marjolin Ulcer?
A Marjolin ulcer is a type of skin cancer that develops in areas where the skin has been previously injured, in longstanding scars, or in wounds that have not healed over a long period of time. This condition is named after Jean Nicolas Marjolin, a French surgeon, who first identified it as an ulcer with thick growths, appearing within a burn scar.
The most common type of cancer found in Marjolin ulcers is called squamous cell carcinoma, even though other types of cells can also become cancerous (like in basal cell carcinoma). These cancerous growths tend to be very aggressive and often reappear after treatment, which leads to a poor overall outlook for recovery.
Preventing Marjolin ulcers through proper management of burn wounds, early detection of cancerous changes, and surgery, if feasible, are extremely important approaches for handling this condition.
What Causes Marjolin Ulcer?
Burn scars are the most common condition that can lead to the formation of Marjolin ulcers, a type of skin cancer that can develop in an old scar or area of skin damage. Statistics show that between 0.7% to 2.0% of burn scars that heal on their own can eventually develop into a Marjolin ulcer.
Other long-standing conditions of skin inflammation that can also cause Marjolin ulcers include wounds from injuries, ulceration that results from poor blood circulation (venous stasis ulcers), bone infections (osteomyelitis), bed sores (pressure ulcers), skin damage from radiation treatment (radiation dermatitis), insect stings, bites, and a chronic skin condition called hidradenitis suppurativa (which causes small, painful lumps under the skin).
In addition, people with weaker immune systems, either due to disease or medication, have a higher risk of their skin conditions turning into Marjolin ulcers.
Risk Factors and Frequency for Marjolin Ulcer
Marjolin ulcers can affect anyone, regardless of age, race, or gender. These ulcers typically develop 30 to 35 years after an initial injury, and are usually diagnosed when a person is around 59 years old. Men have a higher chance of ending up with Marjolin ulcers, as they tend to experience burns more frequently, which can lead to these ulcers. Yet, the risk doesn’t vary with race or ethnicity, since it is equally common for all groups, unlike other types of skin cancer.
- Marjolin ulcers can affect anyone, irrespective of their age, gender, or race.
- These ulcers usually appear 30 to 35 years after an initial injury.
- They are often diagnosed in individuals around 59 years of age.
- Men are more commonly affected than women, probably due to more frequent burns.
- Risk for Marjolin ulcers is consistent across all races and ethnicities.
Signs and Symptoms of Marjolin Ulcer
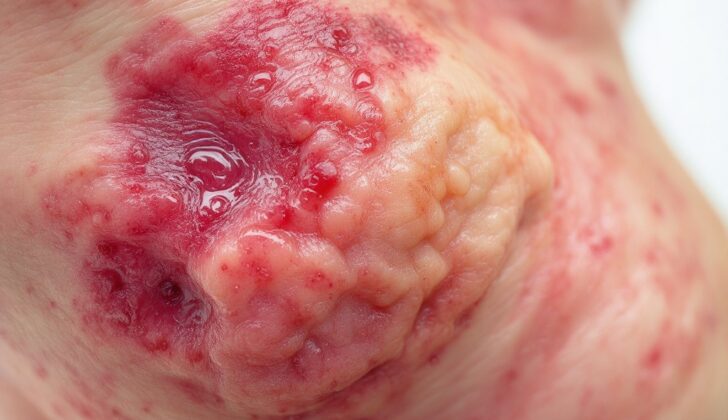
A Marjolin ulcer is a serious condition that can occur in a chronic wound or scar that isn’t healing correctly. This kind of ulcer usually looks like an open, smelly, and rapidly growing sore that might have raised edges. Other signs of Marjolin ulcers might include excessive tissue growth, bleeding, and swollen regional lymph nodes. The form of Marjolin ulcer that actually looks like an open sore is more common and tends to be more aggressive. Sometimes, an infection in the wound can be the first symptom of a Marjolin ulcer. Though they can develop anywhere on the body, these ulcers are most often found on the lower limbs, followed by the scalp, arms, torso, and face.
Doctors and other health professionals should carefully examine any old scars during routine check-ups, and take note of any changes from previous visits.
- An unhealed, hard or open lesion on a chronic wound or scar
- Sore looks open, smells foul, grows rapidly, may have raised edges
- Excessive tissue growth
- Bleeding
- Swollen regional lymph nodes
- Infection of the wound could be first symptom
- Common locations: lower limbs, scalp, arms, torso, face
- Changes in old scars should be noted during routine checkups
Testing for Marjolin Ulcer
If you have a wound or ulcer that doesn’t seem to be healing, especially if it’s on an old scar, your doctor will likely want to take a small sample of it (a biopsy) to check what’s wrong. Your doctor will also physically examine the nearby lymph nodes, which are small, bean-shaped glands that are part of your immune system.
Some healthcare providers might suggest an ultrasound of these lymph nodes because they often can be affected as well. This is also known as lymphatic mapping, and a biopsy of the ‘sentinel’ (main) lymph node may be suggested.
In addition, depending on your situation, other imaging techniques may be recommended. For instance, a chest x-ray (chest radiograph) or a brain scan (computed tomography) might be used to check for any spread of the disease (metastases).
Treatment Options for Marjolin Ulcer
The main aim of managing Marjolin ulcers, which are a type of cancerous sore that can develop in burn wounds, is through prevention. This is because burn wounds that aren’t treated and rather left to heal naturally can become more susceptible to turning cancerous. However, if such ulcers are detected, there isn’t a single recognized treatment plan. The treatment options mostly considered include Mohs surgery, wide local excision, and, in extreme cases, amputation.
Mohs surgery, a precise surgical way to remove skin cancer layer by layer, is typically considered for ulcers in visible and sensitive areas like the face, scalp, hands, feet, and chest. This method is often preferred because it tends to have a better cosmetic outcome. In contrast, amputation might be the only choice when the disease is too advanced for other surgical options.
After removing the ulcer, the resultant wound is often covered with a local flap of skin, a free flap of skin from elsewhere in the body, or a non-vascular graft which is a skin graft that does not involve blood vessels. This approach is debatable as some studies indicate a higher recurrence risk if the ulcer isn’t fully removed. Therefore, after the ulcer has been removed, it’s essential for patients to have regular follow-ups since there’s a high chance of recurrence.
Whether to conduct a lymph node dissection, which is a procedure to remove lymph nodes, is also a matter of debate. It can be considered if there are signs of positive lymph nodes, which mean cancer cells have spread to the lymph nodes, either through a physical check or ultrasound.
If surgery cannot be performed, additional treatments like radiation and chemotherapy may be necessary. Some of the suggested agents for chemotherapy include topical 5-fluorouracil, methotrexate, l-phenylalanine, and platinum-based therapy. Radiation is typically recommended for patients with cancer spread to regional lymph nodes, highly aggressive lesions, and larger lesions exceeding 10 cm in diameter.
What else can Marjolin Ulcer be?
Here are some of the medical conditions related to skin health:
- Actinic keratosis: damage from the sun or other ultraviolet rays.
- Allergic contact dermatitis: a skin allergy caused by contact with certain substances.
- Atopic dermatitis: also known as eczema, a condition making skin red and itchy.
- Atypical fibroxanthoma: a relatively rare skin tumor.
- Basal cell carcinoma: a type of skin cancer that begins in the basal cells.
- Benign cell lesions: non-cancerous skin growths.
- Bowenoid papulosis: a skin condition that could lead to cancer.
- Chemical burns: these occur when skin comes into contact with chemicals causing burns.
- Limbal dermoid: a benign, congenital tumor usually present at birth.
What to expect with Marjolin Ulcer
Marjolin ulcers, a certain type of skin lesion, can be quite aggressive and often have a poor outlook. These ulcers can develop into a spread of disease or “metastasis” in up to 27% of patients, which is much higher compared to the 3% seen in other causes of squamous cell carcinoma, a type of skin cancer.
Moreover, these ulcers have a high chance of recurring even after being surgically removed, with rates up to 50%. Certain factors can indicate a worse outlook, such as the severity of the ulcer (grade II or III), presence of metastasis, and if the ulcer is located on the lower extremity (leg).
Unfortunately, the estimated survival rate over 5 years ranges from 43 to 58% for those with Marjolin ulcers.