What is Mediastinal Seminoma?
Mediastinal seminomas are a very uncommon type of tumor that grow in the mediastinum, the part of your chest that separates your lungs. They originate from germ cells, which are the cells that form eggs in women and sperm in men. It is very rare for these cells to form tumors outside of the ovaries or testes, with a chance of about 5% to 7%. If the tumor isn’t in the ovaries or testes, it’s considered to be extragonadal, or outside the gonads. The mediastinum and a place behind the abdomen called the retroperitoneum, are the most common sites for these tumors, with the mediastinum as the top spot. Seminomas can also occur in the lower part of the spine or in a gland in the brain (pineal gland), and these occurrences are more often seen in children.
These tumors are a rare find in the mediastinum, accounting for only 1% to 4% of all tumors discovered there. They can be either benign (non-cancerous) or malignant (cancerous), with mediastinal seminomas being cancerous.
Mediastinal seminomas often grow very slowly and don’t show distinctive symptoms. In fact, many people won’t experience any symptoms and the tumor will be discovered incidentally. These types of tumors were first identified during the late 1950s. However, since then, treatments have greatly improved and the survival rate for patients with this disease is now between 87% to 100% after 5 years, similar to the survival rate of testicular seminomas. Mediastinal seminomas respond very well to chemotherapy and radiation, so these are usually the first line of treatment. Surgery might also be a treatment option in some cases.
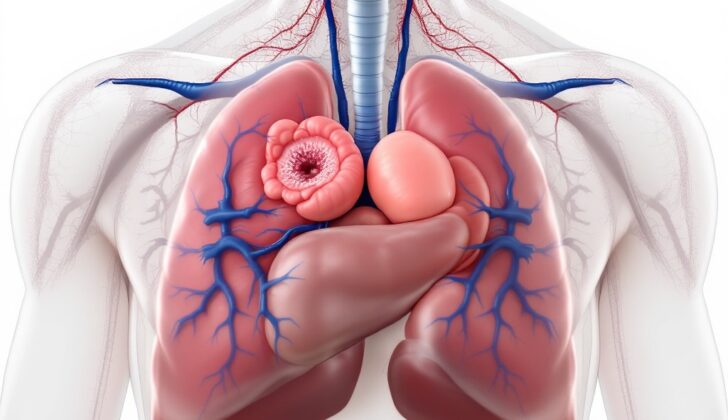
Mediastinal seminomas are generally found in the upper front part of the mediastinum, right where the innominate vein meets the superior vena cava, a large vein carrying blood towards the heart. The mediastinum is bordered by the chest wall on either side, the front and back of your chest, and your diaphragm, which helps you breathe. It can be divided into compartments, which can assist your doctor in planning a treatment course.
Due to their ability to grow quite large, these tumors may sometimes be confused with normal fat or tissue surrounding the heart. They can infiltrate, or spread into, surrounding organs early in their growth and lead to problems such as difficulty breathing when they’re large enough. If the tumor has spread outside of the chest, it was likely discovered at a later stage. Spread of the tumor generally happens through the bloodstream and mainly affects the lungs, liver, and bones. However, usually, mediastinal seminomas stay within the chest.
What Causes Mediastinal Seminoma?
Several theories exist about the development and origin of tumors in the area between the lungs, known as the mediastinum. The first theory suggests that these tumors evolve from primitive cells, known as germ cells, originating from the yolk sac or an area known as the urogenital ridge. Normally, these germ cells move to the scrotum. However, some may not make it and stay in the mediastinum or behind the abdomen, known as the retroperitoneal space.
Another theory speculates that these germ cells have the potential to develop into any type of cell but get misplaced during embryo development, leading to tumors in the mediastinum or retroperitoneal area. The exact cause of these tumors is still unknown, but research has found a higher occurrence in men with Klinefelter syndrome.
Individuals with Klinefelter syndrome have an extra X chromosome, and they tend to develop these germ cell tumors in the mediastinum about ten years earlier than those with normal genetic makeup. Further research reveals that these patients have low testosterone levels and high levels of certain hormones, like estradiol and luteinizing hormone. These hormonal imbalances suggest a problem with the germ cell line, which could disrupt the process of sperm formation and make the patient more susceptible to cancers that occur outside the gonads.
Risk Factors and Frequency for Mediastinal Seminoma
Most germ cell tumors, which are growths that start in the cells that give rise to sperm or eggs, are not cancerous. However, around 20% of these tumors are malignant, or cancerous. Seminomas, a specific type of germ cell tumor, make up about half of all malignant germ cell tumors.
These germ cell tumors can occur outside the gonads, commonly in the mediastinum—the central compartment of the thoracic cavity in your body. However, only 3-10% of all tumors found in the mediastinum are germ cell tumors, and they count for fewer than 5% of all germ cell tumors. And out of these, only 3% are found in the back section of the mediastinum, with most being found in the front section.
A type of germ cell tumor that one can find in the mediastinum is the mediastinal seminoma, which is most commonly seen in males aged between 20 and 35 years. Why it mostly affects males is not clear. These tumors are usually not discovered in patients from less developed countries until they are in their 40s, possibly due to the lack of advanced diagnostic methods in these regions. Despite the rarity of mediastinal seminomas, awareness and knowledge about this condition could increase with more research and education for both doctors and pathologists.
Signs and Symptoms of Mediastinal Seminoma
Malignant tumors like mediastinal seminomas, which are usually larger in size, can often cause noticeable symptoms due to their tendency to put pressure on surrounding organs like the heart and lungs. Despite this, many patients with a mediastinal seminoma may not show any symptoms at all. However, when symptoms do occur, they could be varied.
- Shortness of breath
- Coughing
- Chest pain
- Fast heart rate, if the tumor is affecting hormone levels
- High blood pressure, in cases where the tumor affects hormone levels
- Superior vena cava syndrome, which is a condition caused by the slow-growing nature of the tumor and can lead to swelling and redness in the face, neck, and upper body
No matter what the symptoms, it’s crucial that the patient receives a full physical exam to diagnose the condition correctly.
Testing for Mediastinal Seminoma
If your doctor thinks you may have a mediastinal tumor, which is a type of tumor located in the area between your lungs, the first step to diagnose it would be a chest X-ray. This will provide an image of your chest to help locate any masses. If the X-ray detects a mass, you may then get a contrast-enhanced chest CT scan, an MRI, or a PET scan to get a better look at the mass depending on where exactly it is and where it came from.
Mediastinal seminomas, a specific type of tumor, are typically found in the upper front (anterior-superior) part of this space between the lungs. A CT scan with contrast is usually the first choice for these types of tumors because it’s good at telling the difference between solid masses and fluid-filled ones called cysts. An MRI can then show the exact location of the tumor and if it has started to invade any adjacent structures, like the pleura – a thin tissue that covers the lungs. Mediastinal seminomas usually look homogeneous or the same throughout on CT and MRI. However, in case of bleeding or necrosis (cell death), different changes can appear in smaller areas on these images.
With mediastinal tumors, it’s also important to look at the shape of the mass and if it’s displacing or pushing on any structures within the mediastinum. This can help to further identify the type of mass. If it’s unclear whether a mediastinal tumor is malignant (cancerous) or benign (not cancerous), a PET CT scan is often suggested. You might get additional PET CT scans to check how you’re responding to treatment, like chemotherapy.
Although starting treatment based on tumor markers (labs from a blood test that can indicate cancer) alone is possible, it’s usually best to confirm the diagnosis with a tissue sample. One way to get a sample is by doing a core needle biopsy, which is when a larger needle is used to take a bigger sample. If that doesn’t get the sample needed, you might have a surgical biopsy through an anterior mediastinotomy (also known as the Chamberlain procedure).
Malignant germ cell tumors can release certain substances that can be measured in lab tests. These include alpha-fetoprotein, embryonal carcinoma components, and human chorionic gonadotropin (beta hCG). These tests, along with imaging, can help to diagnose mediastinal seminomas and assess how you’re responding to therapy. Interestingly, pure mediastinal seminomas don’t release alpha-fetoprotein. About one third of people with mediastinal seminomas have elevated levels of beta hCG. If beta hCG levels are higher than 1,000, it may suggest that there’s another type of tumor present that should be investigated.
It’s also important to rule out a gonadal germ cell tumor, which originates from the reproductive organs, in people suspected of having a mediastinal seminoma. The way these different types of tumors spread in the body, which is known as metastasis, is different. Gonadal germ cell tumors often spread to lymph nodes in the area behind the abdomen, while mediastinal germ cell tumors can spread to the lymph nodes in the neck and abdomen.
Treatment Options for Mediastinal Seminoma
Treatment of seminomas, a type of testicular cancer, has evolved over time. Traditionally, the first choice of treatment was chemotherapy and radiation, regardless of the tumor size. Generally, surgery was reserved for tumors that didn’t react to these treatments. Nowadays, it’s more common to do surgery first if the tumor is small and can be easily removed. This is usually followed by radiation therapy.
Cisplatin-based combination chemotherapy is recommended as the first course of treatment, whether or not the tumor has spread to other parts of the body. This therapy is often combined with etoposide and bleomycin. However, if the patient has any existing lung disease, they should not take Bleomycin. If this is the case, Ifosfamide can be added to the cisplatin and etoposide regimen instead. The effectiveness of the chemotherapy treatment is evaluated by measuring tumor markers, which are substances that can indicate the presence of cancer.
If the cancer has spread to other parts of the body at diagnosis, the patient should receive cisplatin-based chemotherapy for the distant disease, and radiation for the disease in the chest region. Some recent studies have found that chemotherapy is more effective as the first treatment option, due to unwanted side effects from chest radiation such as heart or lung issues, secondary cancers, and other harmful effects related to radiation exposure.
In the case of a large tumor, the first step is usually chemotherapy, and then any remaining disease is surgically removed if it seems feasible to do so based on medical imaging. After this, the patient is typically closely monitored for 6 to 12 months with repeated CT scans. Patients who do not show signs of lung metastasis and are in good health tend to have survival rates above 90% after going through chemotherapy.
In the event of a remaining mass, it is important to understand whether the mass is cancerous or necrotic (dead tissue) before deciding on a treatment approach. If the mass is more than 3cm, there’s a higher chance it may contain cancer cells. Monitoring options include regular CT scans, PET scans, or potentially an open biopsy for tissue diagnosis. If the mass grows or a biopsy confirms remaining disease, further treatment could include chemotherapy, radiation, or additional surgery.
When chemotherapy is complete, and there is a remaining mass shown in CT scan but the tumor markers have returned to normal, these patients may be eligible for surgical removal of the mass. The surgical technique depends on the location of the tumor. As the majority of seminomas occur in the front part of the chest, a common surgical approach is median sternotomy, which involves cutting through the sternum. Other potential surgical approaches include sternotomy, thoracotomy, VATS, or robotic surgery.
Throughout surgery, particular attention should be given to lung function, especially if the patient received bleomycin, which can cause lung damage. A double-lumen endotracheal tube is typically inserted in case of the need for lung resection. Decisions to remove certain structures in the chest are made carefully by the surgeon, based on their assessment of whether leaving some of the tumor is outweighed by the potential harm of removal. In certain cases where a tumor has deeply invaded a structure, the whole structure may need to be removed.
If cancerous cells remain after the surgery, chemotherapy treatment can be initiated again. The ultimate goal is to remove all cancerous tissue, while keeping intact as much healthy tissue and organ function as possible.
What else can Mediastinal Seminoma be?
When diagnosing a particular kind of tumor called mediastinal seminomas, doctors need to carry out imaging to figure out if the mass inside the body is solid or similar to a fluid-filled pocket or cyst. This is crucial because many of the masses found in this area of the body, which is the mediastinum, are typically harmless cysts or teratomas. Misidentifying a tumor as one of those could lead to insufficient treatment and unchecked tumor growth.
Secondly, it’s easy to confuse mediastinal seminomas with a type of tumor called a gonadal germ cell tumor because they often spread to specific lymph nodes in the back of the abdomen. However, a key difference is that mediastinal seminomas, which is another type of germ cell tumor, generally spread to the lungs, liver, or bones, not these specific lymph nodes.
Also, the bigger the mediastinal seminoma, the harder it is to distinguish it from surrounding body structures like thymic fat and the pericardium, which is a sac that encloses the heart.
In addition to these challenges, the following medical conditions can also have similar characteristics to mediastinal seminomas and need to be considered:
- Thymoma – a tumor that starts in the thymus
- Thymic carcinoma – a type of cancer that also begins in the thymus
- Mediastinal melanoma – a skin cancer that spreads to the mediastinum
- Lymphoma – a cancer of the lymphatic system
- Clear cell carcinoma – a type of kidney cancer, either originating here or spreading from other sites.
What to expect with Mediastinal Seminoma
Seminomas, a type of testicular cancer, can be cured regardless of their size when they are treated aggressively with radiation and chemotherapy. The initial treatment approach has shifted from solely radiation to a combination of chemotherapy that includes a drug called cisplatin.
However, the outlook for patients who have surgery for a seminoma located in the mediastinum (the area between the lungs) is not as positive. Nearly half of these tumors come back after surgery, and less than 50% of patients live longer than five years after complete tumor removal. In fact, more than 40% of patients will have the cancer come back after complete tumor removal.
But there’s positive news too. Over time, newer treatment methods have led to remission rates of more than 80%, and longer survival rates. Recent studies have shown that when cisplatin-based chemotherapy is started early, survival rates can be greater than 90%.
Possible Complications When Diagnosed with Mediastinal Seminoma
Mediastinal seminomas, or tumors in the area between the lungs, can cause serious problems. They might grow and put pressure on the heart and lungs, or spread to these vital organs. In some cases, they can even spread to distant organs, like the liver and bones.
Surgery is often used to treat these tumors, but it comes with its own potential complications, such as damaging the phrenic nerve (which plays a crucial role in breathing), causing bleeding, or leading to a condition known as pyothorax, which is a collection of pus in the chest cavity.
The bigger the tumor, the higher the risk of these complications. When seminomas get so large that they start to invade surrounding organs, it gets really challenging for doctors to tell the difference between the tumor and regular lung tissue. This means that surgeons have to be extremely careful when they choose to proceed with an operation.
Common complications include:
- Pressure on vital organs like the heart and lungs
- Spread of the tumor to other parts of the body, such as the liver and bones
Risks of surgery can include:
- Damage to the phrenic nerve
- Bleeding
- Development of pyothorax
Preventing Mediastinal Seminoma
If you have had or are currently dealing with a mediastinal seminoma – a type of cancer that develops in the area of the chest that separates the lungs – it’s recommended that you return to physical activity, eat a balanced and healthy diet, and avoid the use of any muscle-building steroids. Additionally, it’s crucial to watch out for any signs that may indicate the cancer is coming back. Such signs can include shortness of breath, coughing, a feeling of pressure in your chest, or unexplained weight loss. Don’t forget to keep all scheduled follow-up appointments with your doctor to ensure you are monitored and treated correctly.