What is Ocular Melanoma?
Melanoma is a cancer caused by the abnormal growth of melanocytes, cells that give skin its pigment or color. One type of this is ocular melanoma, which is the second most common form of melanoma and the most frequently occurring type of cancer that starts inside the eye in adults. Roughly 85% of these cases start in the uveal tract, which includes the iris, ciliary body, and choroid, parts within the eye. The majority of these cancers start in the ciliary body or choroid. Melanoma can also start in melanocytes in the conjunctival membrane, the thin layer that covers the front of the eye. Although these cases account for less than 10% of ocular melanomas.
This cancer is most prevalent in people with light-colored eyes, and other factors such as exposure to sunlight, genetic factors, and underlying diseases can also increase the risk. People with ocular melanoma usually get diagnosed unintentionally during an eye exam, or when they go to the doctor with symptoms like blurred vision, partial sight loss, blind spots, eye pain, or floaters, which are small specks or clouds moving in your field of vision. Doctors use different tools for diagnosis like ultrasound, optical coherence tomography (a simple, painless imaging test), and fluorescein angiography (where a fluorescent dye is injected into the bloodstream to highlight the blood vessels in the back of the eye). In some cases, a biopsy (sample of tissue taken for examination) may be needed for diagnosis.
Even though initial treatment can successfully prevent cancer relapse, about half the people with eye tumors will have potential spread of cancer due to early appearance of tiny metastases. Ocular melanoma often spreads through the bloodstream, usually targeting the liver. The overall prognosis or outlook depends on things like the size and location of the tumor and the characteristics of the cancer cells. However, the choice of initial localized treatment doesn’t affect the long-term survival outcomes.
melanoma.
What Causes Ocular Melanoma?
Uveal melanoma, a type of cancer that develops in the eye, is more likely in people who have ocular or oculodermal melanocytosis (disorders that cause increased pigmentation in the skin and eyes). People with light-colored eyes, fair skin, and a tendency to burn rather than tan, tend to have a higher risk as well. However, it’s uncertain if exposure to ultraviolet light is a risk factor. Although there is a link between skin cancer and ultraviolet light, the connection isn’t as clear with this type of eye cancer. Other risk factors include skin moles, skin freckles, eye freckles, and arc welding.
Your genetics also play a part in your risk for this type of cancer. Some people have certain variations in their genes that make them more likely to develop uveal melanoma. For example, a gene known as TERT (telomerase reverse transcriptase) which regulates cell lifespan, and a gene named CLPTM1L (CLPTM1 regulator of GABA type A receptor forward trafficking) might be connected to an increased risk of uveal melanoma. These genes are thought to be located on chromosome 5p15.33. Other cancers have also been linked with variations in these genes.
The most common genetic variations found in patients with uveal melanoma are in the GNAQ and GNA11 genes, affecting around 71-93% of patients. Variations in BAP1, SF3B1, and EIF1AX genes are also common.
These genetics also affect the long-term outlook for patients. For example, people with a BAP1 mutation, or lack of BAP1 expression are at a higher risk of the cancer spreading. An EIF1AX mutation, on the other hand, is linked to a lower risk of spreading and a better overall outlook. Other factors linked to a poor prognosis include changes in chromosomes like chromosome 8q gain and chromosome 3 loss. Additional genetic variations linked to uveal melanoma are less common and include alterations in the PLCB4, CYSLTR2, RBM10, and SRSF2 genes.
Genetic mutations tied to iris melanoma (melanoma affecting the colored part of the eye) usually resemble those found in uveal melanoma, although BAP1 and SF3B1 mutations are uncommon. An alternative form of the B-Raf proto-oncogene, known as BRAF, is implicated in iris, conjunctival (white part of the eye), and skin melanomas. Conjunctival melanoma additionally involves mutations in the TERT promoter gene, as well as other genes like the NRAS and NF1. These genetic variations significantly affect prognosis. Finally, though some studies suggest a link between BRCA2 gene mutations and ocular melanoma, others have not confirmed this connection.
Risk Factors and Frequency for Ocular Melanoma
Ocular melanoma is the most common type of cancer found inside the eye in adults, making up 3% to 5% of all melanoma cases. The majority of these cases (85% to 90%) occur in the uvea, the middle layer of the eye, while 5% start in the iris and the rest originate from other parts of the eye like the ciliary body or choroid. Most people are diagnosed around the age of 62, but the disease is most common in people aged 70 to 79.
Predominantly, this disease affects white people of northern European descent. Black people are less likely to be affected, and Asian and Hispanic people have a moderate risk. Men are more likely to have ocular melanoma than women. In the US, about 5 in 1 million people are diagnosed with this disease each year. In countries with a large number of people of northern European descent, this number is slightly higher at 7.5 per 1 million people per year.
- Ocular melanoma is the most common cancer inside the eye in adults.
- About 85% to 90% of these cases occur in the uvea.
- The disease usually diagnoses around age 62, with most cases between 70 and 79.
- It primarily affects white people of northern European descent.
- Men have a 30% higher chance of having this disease compared to women.
- Approximately 5 in 1 million people in the US, and 7.5 in 1 million people in Northern European countries, are diagnosed each year.
Signs and Symptoms of Ocular Melanoma
Ocular melanoma, a type of eye tumor, can have various symptoms depending on where it’s located. Many people don’t notice any symptoms and find out they have the disease during a routine eye checkup. It often doesn’t cause any problems in the early stages, especially when located in the choroid or ciliary body parts of the eye. Iris-based melanomas might cause a noticeable growth change in a childhood mole. Melanomas on the conjunctiva can appear in previously clear areas, existing moles, or as spreading coloration due to primary acquired melanosis.
Some people with ocular melanoma may feel discomfort because of increased eye pressure or nerve involvement. Vision can also be affected, leading to symptoms like fading vision, spots in vision (scotoma), and seeing floats. These symptoms can stem from a variety of reasons such as cataract formation, melanoma growth blocking the eyesight path, retinal detachment, and bleeding within the eye.
- No noticeable symptoms in early stages
- Discomfort from increased eye pressure or nerve pressure
- Fading vision
- Seeing spots or floats
- Change in growth of a childhood mole (iris melanoma)
- Spreading coloration on the conjunctiva
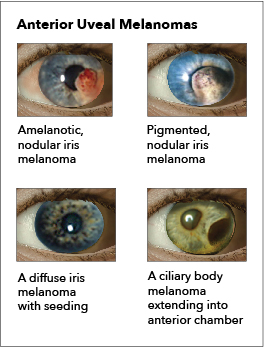
During a physical examination, doctors might find different signs based on where the melanoma is located. If it’s on the choroid part of the eye, it likely appears as a clearly defined, dome-shaped mass under the retina. This mass may have a mushroom-like growth pattern and can have different color shades.
If it’s on the iris, the color could range from yellow to brown. The iris may also get dark unilateral in people with diffused lesions.
When found in the ciliary body, the early sign could be the presence of a particular blood vessel – a sentinel vessel. Doctors will check this by dilating the patient’s pupils and inspecting the front and back of the eye. In some cases, an unexplained, unusually low eye pressure in one eye might be the only sign of a ciliary body melanoma.
Conjunctival melanomas might be attached to lower layers and spread to the outer parts of the cornea. Some people might observe coloration on the eyelids and skin. In some cases, lymph nodes near the affected eye might become enlarged.
Testing for Ocular Melanoma
Diagnosing uveal melanoma, a type of eye cancer, is usually done through an eye examination and ultrasound. In about 5% of cases, a biopsy may be needed to confirm the diagnosis. Certain signs during an examination, such as a thicker tumor, fluid under the retina, symptoms affecting vision, and certain features observed in an ultrasound, increase the suspicion of cancer.
Fundus Imaging
Using a specialist fundus camera, doctors can take photographs of the inside of your eye to estimate the size of the tumor. This also helps to spot any retinal detachment, to check whether the tumor has spread to nearby areas, and to identify any unusual pigmentation. Most melanomas show up as dome or mushroom-shaped, and they can range in color from gray to greenish-brown.
Ultrasound
Ultrasound technology is very useful in the diagnosis of ocular melanoma because it can measure and visualize the tumor and surrounding structures. However, anomalies smaller than 1mm may not be caught, and this technique might overestimate the size of the tumor. There are also chances that other conditions such as choroidal nevi, metastatic neoplasms, and choroidal hemangiomas might share similar features with melanoma on ultrasound.
Optical Coherence Tomography (OCT)
OCT builds images by processing light waves. It’s good for spotting conditions like iris melanoma, iris nevi, iris melanocytoma, and ocular surface squamous tumors. A type of OCT, called OCT angiography, improves early detection and differentiates between malignant and benign tumors by analyzing the vessels of the tumor. However, OCT can meet challenges when dealing with pigmented lesions or tumors larger than 5mm in diameter.
Fundus Fluorescein Angiography
This technique uses a dye to illuminate the retina and characterize its blood vessels. It can be useful in distinguishing pigmented and nonpigmented tumors, but it cannot definitively diagnose uveal melanoma on its own. It also helps to identify other conditions such as hemangioma, hemorrhage, or choroidal detachment.
Magnetic Resonance Imaging (MRI)
MRI helps in identifying the exact location and size of the tumor and if it has spread to nearby tissues. Its limitations include not being able to distinguish between amelanotic and melanotic melanomas, and possible distortions caused by blinking or involuntary eye movements.
Computed Tomography (CT)
CT scans are not routinely used to diagnose uveal melanoma as they do not accurately distinguish uveal melanoma from other conditions or measure the tumor size precisely. However, they are useful in confirming the diagnosis and assessing if the disease has spread.
Positron Emission Tomography and Computed Tomography (PET-CT)
PET-CT uses radioactive tracers to detect metabolic abnormalities and is excellent for spotting distant metastasis, particularly in the liver. However, it is an expensive imaging technique and also exposes the patient to significant radiation.
Laboratory Evaluation
Upon diagnosis, various blood tests are conducted to check liver function, as the liver is the most common site for metastasis. If these tests come back abnormal, an MRI of the liver may be needed. Additionally, after tumor removal, the tumor can be tested which helps determine the prognosis and monitor for any reccurence of the cancer.
Treatment Options for Ocular Melanoma
The treatment for ocular melanoma, which is a type of eye cancer, can depend on factors like the size and location of the tumor. Some methods used to treat this condition include watching and waiting, plaque radiation therapy, particle beam radiotherapy, laser treatments, local surgical removal, and enucleation (removal of the eye).
For people with small uveal melanomas (melanomas found in the middle layer of the eye), who have no symptoms, the approach may be to keep an eye on the condition and see if it progresses, especially if the tumor is less than 12 mm in diameter and 2 to 3 mm in height. During this period, regular check-ups every 2-4 months involving certain imaging techniques could be recommended. Likewise, less aggressive melanomas of the iris (the colored part of the eye) are also commonly kept under observation. If, however, the tumor grows rapidly or becomes large, various treatments, from brachytherapy and proton beam RT to local excision or even enucleation, may be considered.
Radiation therapy is commonly used to treat primary uveal melanoma and is designed to keep the eye preserved. The cancer cells of uveal melanoma can be quite resistant to radiation which is why plaque brachytherapy and charged-particle radiation therapy, are the methods used. Plaque brachytherapy involves attaching a gold-covered, dish-shaped device with a radioactive source to the eye to target the tumor. After treatment, regular check-ups are important to keep track of any complications that may arise. Charged-particle radiation therapy is an alternative that tends to be preferred when the melanoma has spread around the optic nerve or grows too big to be treated with plaque brachytherapy.
Transpupillary thermotherapy is a treatment that uses an infrared diode laser to heat the entire tumor to temperatures (around 45 to 60 °C), thereby killing off the tumor cells. This method, which is often used alongside radiation therapy, does have a risk of the cancer reappearing (around 30%) after 3 years.
Laser photocoagulation is another treatment option, but this method, which works by using high-temperature thermal energy to harm the tumor, isn’t frequently used for ocular melanoma due to the high rate of the cancer coming back and potential complications.
Local surgical removal is another approach typically reserved for conjunctival melanoma (an extremely rare form of eye cancer) because the method does pose risks of serious post-surgery complications and high recurrence of the cancer. To minimize the risk of the cancer returning, local surgical removal is generally combined with radiation therapy.
Enucleation, or the removal of the eye, doesn’t usually improve survival rates over plaque brachytherapy for most patients. Surgeons usually only consider enucleation for patients with large tumors, significant extension outside the eyeball, neovascular glaucoma, retinal detachment, low vision potential, or for patients who opt for enucleation.
For metastatic uveal melanoma, or uveal melanoma that has spread to other parts of the body, certain drugs such as tebentafusp-tebn and darovasertib, have been shown to increase overall survival. These drugs work by using the patient’s immune system to attack the cancer cells.
Patients are typically put into low, medium, or high risk categories, which helps doctors recommend a surveillance schedule for metastatic disease. These categories are determined by a series of specific traits, including the staging of the ocular melanoma, the presence of certain genetic abnormalities, and certain eye conditions. The imaging schedule recommended by doctors can range from annually for low-risk patients, every 6 to 12 months for medium-risk patients, and every 3 to 6 months for high-risk patients. Here, it’s important to note that an MRI is usually the preferred method for systemic imaging, although CT scans and ultrasounds are acceptable alternatives for low-risk patients.
What else can Ocular Melanoma be?
Ocular melanoma, which involves cancerous growth in the eye, can often be confused with other eye diseases. Although doctors can estimate what the growth might be based on its visual appearance, they can’t give an exact diagnosis without a medical test called a biopsy. Here are some of the diseases that might be confused with two types of ocular melanoma, namely, choroidal and ciliary body melanomas:
- Choroidal detachment
- Intraocular foreign body, which is when something foreign is lodged in the eye
- Chronic angle closure glaucoma, a type of eye disease that can cause sight loss
- Hyphema or bleeding in the eye
- Cavernous hemangioma, which is a type of blood vessel malformation
- Vitreous hemorrhage or bleeding into the clear gel that fills the space between the lens and the retina of the eye
- Age-related macular degeneration
- Melanocytoma, a rare, pigmented tumor
- Medulloepithelioma, a rare, malignant eye tumor
- Choroidal osteoma, a benign eye tumor
- Adenoma and Adenocarcinoma, both forms of glandular tumors
- Hamartoma of the retina and pigment epithelium
- Conditions like congenital hypertrophy and reactive hyperplasia of the retinal pigment epithelium
- Lymphoid tumor
- Hemangiopericytoma, a rare form of soft tissue cancer
- Leiomyoma and Neurofibroma, both forms of benign tumors
- Glioneuroma, tumors that affect nerve tissue
- Astrocytoma and Rhabdomyosarcoma, both forms of cancer
- Conditions like Posterior uveitis, Sarcoid nodules, Tubercular granuloma, and Uveitis (different types of inflammations in the eye)
Similarly, iris melanoma might look like the following conditions:
- Iris pigment epithelial cyst and Iris stromal cyst
- Iris nevi, small patches of freckle-like pigments
- Iris metastases, cancer that has spread to the iris
- Iridocorneal endothelial syndrome and Cogan-Reese syndrome, both are disorders of the eye
- A foreign body in the iris
- Koeppe or Busacca nodules
- Lisch nodules, small pigmented hamartomas
- Other iris tumors, such as leiomyoma and rhabdomyosarcoma
Conjunctival melanoma, a rare form of eye cancer, also need to be differentiated from conditions such as:
- Conjunctival squamous cell carcinoma, a type of skin cancer
- Conjunctival melanosis, which involves dark spots on the white part of the eye
- Conjunctival mycosis, a fungal infection of the eye
- Conjunctival seborrheic keratosis, a benign skin growth
- Acquired melanosis, a condition that results in darker patches of skin or eye tissue
- A foreign body like graphite
- Drug toxicity, such as from epinephrine
- Pseudomelanoma, a term used for lesions mimicking conjunctival melanoma
What to expect with Ocular Melanoma
Local treatment is able to stop the cancer from coming back locally in 95% of people. However, due to cancer cells that are too small to see spreading to other parts of the body, half of the people with uveal (eye) tumors will develop cancer that spreads (metastatic disease). This spread is typically deadly, with people living on average only 10 months afterward.
Several factors can negatively impact survival rates, including being older, the size of the tumor, involvement of the ciliary body (a part of the eye), the tumor spreading outside the eye, the type of cells found in the tumor, and specific patterns seen in the blood vessels of the tumor.
Studying the chromosomes of the tumor can provide some information about what might happen, particularly looking for changes in chromosomes 3 and 8. However, looking at the activity of set of genes (gene expression profiling) can provide better predictions. This technique looks at the activity of 15 genes to estimate the tumor’s likelihood of spreading. People’s tumors are then grouped as either class 1 (low likelihood of spread) or class 2 (high likelihood of spread). Additionally, looking for cancer cells or DNA in a person’s blood may also help predict the spread of the disease.
The 5-year survival rate for a type of eye cancer called conjunctival melanoma treated is 83% to 84%, and the 10-year survival rate is 69% to 80%. The overall death rate for two other types of eye cancer—choroidal melanoma and ciliary body melanoma—is 30% to 50% within 10 years, mainly due to the spread of the disease. The overall death rate for yet another type of eye cancer, iris melanoma, is 0% to 11%.
Possible Complications When Diagnosed with Ocular Melanoma
The problems that can arise from ocular melanoma, a type of eye cancer, are not restricted to the spread of the disease (metastasis) and death. There are a variety of associated issues such as losing vision, developing glaucoma, the removal of the retina, forming cataracts, uneven focus, and swelling in the retina due to fluid buildup (macular edema).
There are also potential complications after radiation therapy (RT), which can appear up to 5 years after treatment. These complications include radiation-induced damage to the retina and a new type of glaucoma. Using a specific type of drug (called an intravitreal anti-vascular endothelial growth factor) after a form of radiation therapy called brachytherapy might help to delay or slow down the beginning of macular edema and the related vision loss.
After radiation therapy, patients could also experience dry eye, bleeding inside the eye, inflammation within the eye, tissue death in the outer layer of the eye, optic nerve damage, loss of eyelashes, and issues with tear gland function. These negative effects are more likely to happen with a type of radiation therapy that uses charged particles. Other specific therapies, like heat-based therapy applied through the iris (transpupillary thermotherapy), could lead to blockage of blood vessels in the retina.
Common Complications:
- Vision loss
- Glaucoma
- Retinal detachment
- Cataract formation
- Astigmatism
- Macular edema
- Radiation-induced retinopathy
- Neovascular glaucoma
- Dry eye
- Vitreous hemorrhage
- Uveitis
- Scleral necrosis
- Optic neuropathy
- Lash loss
- Lacrimal gland dysfunction
- Retinal vascular occlusion
Preventing Ocular Melanoma
Ocular melanoma, a type of eye cancer, may still lead to death in 30-50% of patients, even if the initial cancer has been treated successfully. This is unfortunately due to the cancer spreading to other parts of the body, a process known as metastasis. Factors that may increase the risk of developing ocular melanoma include having fair skin, light-colored eyes, and being older. It’s important to detect this type of cancer early for a better chance of successful treatment.
To aid early detection, the American Academy of Ophthalmology suggests getting an eye exam where the doctor widens or dilates your pupils. This should be done by the age of 40. Other risk factors also include conditions like dysplastic nevus syndrome, a predisposition to develop many moles, having a family history of ocular melanoma, eye freckles, and exposure to certain types of welding at work. Also, carrying a mutation in a gene called BAP1 can also raise your risk.
If you’re someone who doesn’t show any symptoms but are at a risk, you are advised to get screened for cancer to help detect any signs early on. People with these risk factors may also find it helpful to have an eye doctor exam every year. One way to potentially prevent this type of cancer if you are at risk is by limiting exposure to the sun.
If you’ve been diagnosed with ocular melanoma, you should be aware that there’s a risk that the cancer could spread even years after you first found out you had cancer. It’s important to keep checking for signs of cancer spread regularly. This means it’s key to go to all follow-up appointments with your doctor, regardless of how advanced your cancer was and what kind of treatment you’ve had. How often these checks are needed can depend on how advanced the cancer was, and if it’s more likely to spread, checks can be as often as every 3 to 6 months for the first 5 years.