What is Osteoblastoma?
Osteoblastoma is a rare, non-cancerous tumor that forms in the bones. It makes up about 1% of all bone tumors and between 1 to 5% of all non-cancerous bone tumors. Some also consider them to be 10% of all tumors related to the spine. In the past, people often compared osteoblastoma to another kind of bone tumor called osteoid osteoma due to their similar characteristics. However, most medical professionals now recognize them as unique, with different symptoms and behaviors.
An osteoblastoma is found most frequently in the back part of the spine and the sacrum, at the bottom of our spine, in about 30 to 40% of cases. Other popular areas include the lower jaw, where it is called a cementoblastoma, and long bones in our legs and arms, particularly in a region called the metadiaphysis.
Diagnosis is typically based on a mix of a patient’s symptoms, imaging tests like X-rays, and microscopic evaluation of the tissue. The appearance of osteoblastoma in imaging studies may differ, ranging from slow-growing to very aggressive. Generally, the outlook for patients with osteoblastoma is good, with most people becoming tumor-free after surgical treatment to scrape out (curettage) or completely remove (en bloc resection) the tumor.
If the tumor cannot be removed surgically, radiation therapy may be used. For instances that show more aggressive pictures or symptoms, it may be necessary to differentiate between osteoblastoma and two borderline bone diseases, aggressive (epithelioid) osteoblastoma, and osteoblastoma-like osteosarcoma. In rare cases, osteoblastoma can be linked to whole-body symptoms such as fever, weight loss, and a condition called diffuse periostitis, equated to toxic osteosarcoma.
What Causes Osteoblastoma?
The exact cause of a condition called osteoblastoma isn’t fully known yet. Similarly, we aren’t sure about the factors that can make a person more likely to get this condition.
Risk Factors and Frequency for Osteoblastoma
Osteoblastoma is a rare, non-cancerous bone tumor that makes up 1% of all primary bone tumors and between 1 to 5% of all non-cancerous bone tumors. This condition mainly affects teenagers and young adults, especially males. Osteoblastoma can occur in any bone, but it most commonly affects the spine and the sacrum, which is a part of the lower back. It can also commonly occur in the facial bone structures and in the long bones of the lower limbs.
Osteoblastoma occasionally affects the bones in the feet, the hand bones, and the knuckles, but these cases are less common. Just like a similar condition known as osteoid osteoma, osteoblastoma can be found in the outer layer of the bone, inside the bone, or sometimes around the bone.
- Osteoblastoma is a rare, non-cancerous bone tumor.
- This tumor represents 1% of all primary bone tumors and 1 to 5% of non-cancerous bone tumors.
- It mostly impacts teenagers and young adults, more commonly males.
- Osteoblastoma can occur in any bone, with a preference for the spine and sacrum.
- The facial bones and long bones in the lower limbs are also common sites.
- Less frequently, it can affect the bones in the feet, the hand bones, and the knuckles.
- Osteoblastoma can be located in the outer layer of the bone, inside the bone, or occasionally around the bone.
Signs and Symptoms of Osteoblastoma
Osteoblastomas are typically slow-growing and often don’t cause any noticeable symptoms. They’re frequently discovered during medical imaging for other health concerns. This sets them apart from osteoid osteoma, another bone condition that usually affects slightly younger people and causes night-time pain that can be eased by taking salicylates.
When symptoms do occur, the most common is a dull and localized pain. Some patients might experience tenderness or soft tissue swelling when the osteoblastoma is near the skin’s surface. Such mild symptoms can be nonspecific, which can delay the patient seeking medical attention. A study indicated that on average, patients experienced symptoms for six months before seeing a doctor.
Osteoblastomas in the spine can cause back pain, curvature of the spine, and pressure on the nerves. Pressure on the nerves can result in muscle weakness or even paralysis. There’s also a rare form of osteoblastoma that comes with system-wide symptoms such as fever, loss of appetite, weight loss, and widespread inflammation of the bone and surrounding tissue.
Osteoblastomas rarely affect surrounding soft tissues and don’t usually trigger inflammation or fluid buildup in nearby tissues. The prognosis for osteoblastoma is generally good, despite a risk of reoccurrence of the tumor in some cases. There have been rare reports of osteoblastomas becoming cancerous, but new genetic research contradicts these findings.
Testing for Osteoblastoma
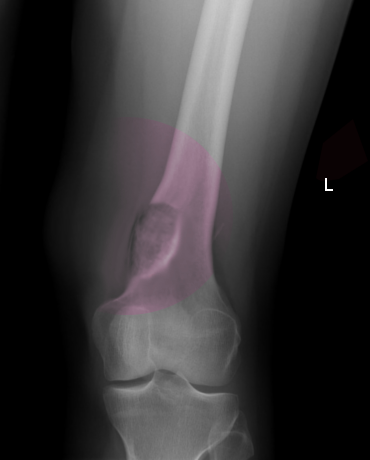
To diagnose osteoblastoma, a type of bone tumor, the doctor may use various imaging techniques such as X-ray pictures, CT (Computed Tomography) scans, and MRI (Magnetic Resonance Imaging) scans. Sometimes, osteoblastoma can be difficult to differentiate from a similar condition called osteoid osteoma when looking at these images.
Most often, the pictures from these tests show round or oval lesions (abnormal areas) that are radiolucent (appear dark on X-ray images). These lesions have well-defined edges and may show reactive sclerosis, which is a sign of increased bone formation in response to injury or disease. It’s been speculated that younger patients may have more radiolucent lesions while older patients show increased bone formation/sclerosis. In some instances, around 20% of cases, these lesions may give the wrong impression of a cancerous process.
The appearance of these lesions on X-ray images can vary and come in four distinct types. Each type can give doctors clues about the nature of the tumor and help in the diagnosis of osteoblastoma. These pictures can show if the tumor has an expanded appearance, if the bone’s outer layer (cortex) has thinned, or if the cortex has been disrupted causing destruction.
A CT scan can also aid in the diagnosis by providing more detailed images and additional information such as the exact size and position of the lesions and whether there is any disruption of the cortex. The CT scan is particularly helpful for diagnosing lesions that are difficult to see clearly on X-rays, such as those involving the spine or pelvis.
An MRI provides detailed images and can help to determine the extent of the lesions and if there are any aggressive elements. The MRI is superior to CT scans in identifying reactions in the surrounding soft tissue due to the excellent contrast resolution, although CT scans are still better at identifying the type of internal matrix (substance filling the lesion space) and the level of bone erosion.
Although not commonly used, nuclear medicine imaging techniques can also be employed for osteoblastoma diagnosis. These involve the use of certain radioactive substances which uptake in the tumor, providing further information about the tumor’s characteristics. Overall, the combination of these imaging techniques allows for a more accurate diagnosis and better treatment planning of osteoblastoma.
Treatment Options for Osteoblastoma
If you are diagnosed with osteoblastoma, which is a type of bone tumor, the main treatment you would likely receive is surgery. The type of surgery, either en bloc resection or curettage, depends on a few factors such as the position of the tumor in the bone, the clinical aspects of your situation, and the likelihood of cancer.
En bloc resection is a type of surgery where the tumor is removed all in one piece. It is usually the preferred method since it has a lower chance of the tumor coming back compared to curettage. Curettage is a type of surgery where the tumor is scraped out from the bone. Determining the exact location of the tumor during the operation and thoroughly removing it can lead to good results both clinically and when looking at images of the bone. This also helps to prevent the tumor from occurring again. However, there is still a risk of recurrence, with some studies suggesting that this can happen in as many as 1 in 4 cases. Recurrence means the tumor has come back after treatment. In some rare cases, the tumor might recur multiple times.
There is typically no definitive need for other treatments like chemotherapy or radiotherapy, which are treatments that use drugs or high-energy rays to kill cancer cells.
Because there is a chance that the tumor might come back, you may need to have regular imaging tests, like X-rays and MRI scans. These will help your doctor keep an eye on the area where the tumor used to be. Although there have been isolated reports of osteoblastoma turning into cancer, recent studies looking at genes suggest that this is not very likely.
What else can Osteoblastoma be?
While diagnosing bone conditions, similar patterns and symptoms can lead to some conditions being easily confused with others. It is crucial for doctors to carefully consider all possibilities and understand the slight differences that distinguish one from another.
Some conditions look similar to an osteoblastoma, a benign bone tumor, under the microscope and in radiology scans, they include:
- Osteoid osteoma
- Aneurysmal bone cyst
- Giant cell tumor of bone
- Osteoma with osteoblastoma-like features
- Osteoblastoma-like osteosarcoma
- Infections like Brodie abscess
Osteoid osteomas, which are generally pain-relieving, can look similar to osteoblastomas. However, they usually show up more in the legs and arms whereas osteoblastomas typically present in the spine and face, particularly the jaw.
Aneurysmal bone cysts (ABCs) can also seem like osteoblastomas but key differences involve the typical radiographic appearance, which includes an eccentric, expansive, clear lesion that often has a well-defined, thin outer layer.
Giant cell tumors are also benign tumors that can be mistaken for osteoblastomas due to their similar appearance. Keep in mind that these tumors generally affect the end area of the long bones, and women are more likely to have them than men.
Brodie abscess is a chronic type of bone infection that is most common in children and can be mistaken for osteoblastomas. The infection can lead to a clear lesion, often in the growth area of long bones like the tibia, the most common location.
There are also bone conditions that can be aggressive and often mistaken for osteoblastomas. These include osteoblastoma-like osteosarcoma and aggressive osteoblastomas. When screening these conditions, doctors look for certain features such as poorly defined margins, interrupted cortical bone, or involvement of the nearby soft tissues, something not commonly seen in conventional osteoblastomas.
Osteosarcomas, a type of bone cancer, also appear similar to osteoblastomas. However, osteosarcoma usually presents a more aggressive appearance, with specific features like compromised cortical bone and an enhancing soft tissue element, features often absent in cases of osteoblastoma.
Although these conditions may share similarities with osteoblastoma, subtle differences in their presentation help physicians diagnose accurately and subsequently determine the best course of treatment for the patient.
What to expect with Osteoblastoma
The outlook for osteoblastoma, a type of bone tumor, is largely positive, with most patients effectively cured after the first surgical procedure. Yet, it’s not uncommon for the condition to return, with reported recurrence rates of 15% to 25%.
Returns are more likely for lesions that have been treated with curettage, a procedure where a scoop or curette is used to remove tissue. This method is often used in treating spinal lesions due to the complexity and potential risks involved in doing a wider, local excision. As a result, higher recurrence rates have been observed in spinal lesions. Relapses usually happen within the first two years after treatment and are rare after that period.
Sometimes, lesions that border on being an aggressive osteoblastoma or resembling osteosarcoma (a type of cancer that starts in the bones) can be incorrectly identified as osteoblastoma. This can lead to late diagnosis and incomplete treatment. Because of the likelihood of recurrence, patients usually undergo regular imaging and health check-ups for at least two years after treatment.
While some reports suggest that osteoblastoma can turn into osteosarcoma, recent genetic studies suggest otherwise. The conversion of osteoblastoma to osteosarcoma is extremely rare, but it has been documented in a few cases.
Possible Complications When Diagnosed with Osteoblastoma
After having surgery to remove an osteoblastoma, which is a type of bone tumor, some common immediate complications can occur. These often include:
- Infections of the wound, along with infections affecting the urinary tract and lungs
- Bleeding from the surgical site
- A decrease in the stability of the surgical stabilizing framework put in place during surgery.
In some cases, the tumor can come back long after the surgery, so doctors and patients need to be prepared for this possibility. This means regularly checking for signs of the tumor returning for some time after the operation. Unfortunately, there’s no agreed-upon timeline for how long this needs to be done. The time can vary widely. However, it’s generally a good idea to continue having these check-ups until the chance of the tumor coming back becomes very slim, according to scientific literature.
Preventing Osteoblastoma
Osteoblastoma, a type of bone tumor, has a chance of coming back in about 10 to 20% of patients. Whether or not the tumor recurs largely depends on how successfully the surgeon was able to remove it without injuring any healthy tissues. The amount of time a patient needs to get back to their regular day-to-day activities can differ based on where the tumor was located and the surgical method used to remove it. If the tumor does come back, the treatment plans will still basically be the same.












