What is Pancreatic Cancer?
Pancreatic cancer is a type of cancer that starts in the cells that form the ducts of the pancreas, which is known as pancreatic ductal carcinoma. It is the fourth highest cause of cancer-related deaths in the United States. The survival rate over five years in the US is between 5% to 15%, and the overall survival rate is only at 6%. The only current known cure for pancreatic cancer is surgical removal of the affected part; however, only 20% of the cases are eligible for this surgery at the time of diagnosis.
It is incredibly important that different types of medical specialists work together closely to give patients the best chance of survival. These include surgeons, cancer specialists (oncologists), radiation therapy specialists (radiation oncologists), disease diagnosing specialists (pathologists), and medical imaging specialists (radiologists). Close cooperation boosts survival chances for patients whose disease can be surgically removed (resectable disease), as well as for those with disease that is uncertain for surgery (borderline resectable disease).
What Causes Pancreatic Cancer?
Smoking is a major risk factor for pancreatic cancer, causing about 20% of cases. There are other risk factors that could increase your chance of developing this type of cancer, including:
* Being over 55 years old
* Having diabetes
* Being obese
* Suffering from continuous inflammation of the pancreas (Chronic pancreatitis)
* Suffering from cirrhosis (severe scarring of the liver)
* Having a Helicobacter pylori infection – a common stomach infection
* Working in industries like dry cleaning and metalworking that expose you to certain harmful chemicals
* Being a man more than being a woman
* Being an African American more than being white
* Having a family member who had pancreatic cancer
In around 10% of cases, pancreatic cancer can be caused by genetic factors like genetic mutations or being associated with specific syndromes namely, Lynch syndrome, Peutz-Jeghers syndrome, VonHipual Lindau syndrome, and Multiple Endocrine Neoplasia type 1 (MEN1).
There are other things that could potentially increase your risk, such as drinking a lot of alcohol, consuming coffee, not exercising, eating lots of red meat, and drinking two or more fizzy drinks each day.
Risk Factors and Frequency for Pancreatic Cancer
Pancreatic cancer is a serious health concern globally, causing over 331,000 deaths each year and ranking as the seventh leading cause of cancer-related death in both men and women. The chance of surviving for five years after being diagnosed is about 5% globally.
The frequency of pancreatic cancer is highest in places like North America, Western Europe, and Australia/New Zealand. It’s least common in Middle Africa and South-Central Asia.
- Men are most likely to develop this cancer in countries like Armenia, the Czech Republic, Slovakia, Hungary, Japan, and Lithuania.
- The lowest risk for men is seen in Pakistan and Guinea.
- Women, on the other hand, have the highest rates in Northern America, Western Europe, Northern Europe, and Australia/New Zealand.
- The lowest rates for women can be found in Middle Africa and Polynesia.
The risk of getting pancreatic cancer increases with age, most frequently affecting those above 70 years old. Close to 90% of all cases are found in people over 55 years old.
Signs and Symptoms of Pancreatic Cancer
Pancreatic adenocarcinoma is a type of cancer that usually causes symptoms such as:
- Painless jaundice (yellowing of the skin and eyes) in about half of the patients, due to blockage of a duct that carries bile from the liver to the intestines by the tumor.
- Weight loss in roughly 90% of sufferers.
- Abdominal pain in around 75% of those affected.
- Physical weakness, itchy skin due to bile salts in the skin, loss of appetite, a swollen yet non-tender gallbladder that can be felt, pale stools, and dark urine.
In some cases, patients may also experience repeated episodes of deep vein thrombosis (a condition where blood clots form in the deep veins of the body), often caused by increased blood clotting tendency. Such episodes can lead doctors to check for signs of cancer.
New-onset diabetes can also be a sign of pancreatic adenocarcinoma.
In terms of laboratory findings, these may include:
- Increased levels of liver function tests.
- Increased levels of direct and total bilirubin, substances usually found in the liver and blood.
- Raised levels of amylase and lipase, enzymes produced in the pancreas.
- Elevated levels of pancreatic tumor markers (specific proteins), such as CA 19-9 and CEA.
Testing for Pancreatic Cancer
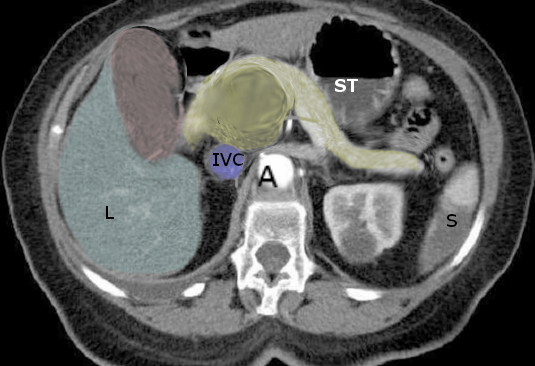
If your doctor thinks you might have pancreatic cancer, a type of imaging called multidetector computed tomography, or MDCT, is the best way to check for it and see how far it has spread within your body, including whether it’s growing into surrounding blood vessels or has spread to other parts of your body. MDCT is very accurate in predicting whether a tumor can be surgically removed or not.
MDCT involves a process called multiphase imaging, which includes a late arterial phase and a portal venous phase, all after you’re given a contrast material through an intravenous (IV) line. The late arterial phase, which is taken about 35 to 50 seconds after the contrast is injected, helps the doctor see the pancreas tissue clearly. The portal venous phase, taken at 60 to 90 seconds after the contrast injection, helps assess the veins and is best for detecting cancer that has spread to the liver or other distant parts of the body. Water is often used as an oral contrast, but barium-based contrast is generally avoided because it can interfere with the evaluation of the blood vessels.
A PET CT scan can also be helpful in detecting cancer that’s spread to distant parts of the body.
An MRI (magnetic resonance imaging) of the abdomen with IV contrast can be just as good as MDCT in determining the extent of pancreatic cancer before surgery, including whether the cancer has spread or grown into blood vessels. MRI is even better than CT at detecting cancer spread to the liver. If there’s a high suspicion of pancreatic cancer, but the CT scan doesn’t show it, then an abdominal MRI might be ordered. However, the quality of MRI images depends on your ability to hold your breath and follow instructions.
Ultrasound, however, is usually not as useful for looking at the pancreas; this is mainly because bowel gas often interferes with the images. Ultrasound can detect dilation of the bile ducts that’s often associated with cancer of the pancreas head, but it’s not very good for seeing the pancreatic mass itself.
Endoscopic ultrasound, a test done by a stomach and digestive specialist, can provide a better view of the pancreatic mass and can be used to obtain a biopsy (a small tissue sample) of the mass. In some cases, a scope is used to inject contrast dye into the bile duct and pancreatic duct; this is called endoscopic retrograde cholangiopancreatography (ERCP). This can help see where the ducts are blocked and, in some cases, placing a stent (a small tube) in the bile duct can help relieve jaundice symptoms.
How far the pancreatic cancer has spread, particularly to blood vessels and other organs, will determine whether it can be removed by surgery or not. If the cancer has spread to the liver, peritoneum (the lining of the abdomen), omentum (the fatty layer that covers the intestines), or lymph nodes outside the pancreas region, it is considered “non-resectable” or “unresectable,” meaning it can’t be completely removed. Involvement of certain blood vessels, like more than half of either the superior mesenteric artery and the celiac artery, also categorizes the cancer as non-resectable. For those with vein involvement, options for reconstruction need careful consideration. In some specific circumstances, a tumor can be categorized as “borderline” resectable, meaning surgery may be possible if certain conditions are met.
Treatment Options for Pancreatic Cancer
If the cancer of the pancreas (pancreatic adenocarcinoma) is deemed to be in an advanced stage and has spread to nearby parts of the body, it is termed as “locally advanced.” In such cases, the cancer is not curable through surgery (unresectable). Instead, doctors typically recommend starting treatment with chemotherapy or radiation therapy, designed to shrink or kill cancer cells.
The recommended surgical procedure for pancreatic cancer depends on the tumor’s location within the pancreas. If the cancer is found in the head of the pancreas, doctors typically use a technique called the Whipple procedure, medically known as a pancreaticoduodenectomy. If the cancer is detected in the body or tail of the pancreas, surgery to remove that specific part of the organ is necessary, a procedure known as distal resection.
After surgery, patients may receive treatment with a type of chemotherapy drug like 5-FU or gemcitabine, alongside radiotherapy, to kill any remaining cancer cells. The choice of treatment is, however, complex when certain blood vessels near the pancreas have cancer growth. For example, if the cancer has grown into the hepatic artery, a crucial blood vessel in the liver, then surgery may not be possible. On the other hand, if the cancer involves the superior mesenteric vein or the portal vein – blood vessels that carry blood from the gut area – surgery may still be an option, followed by reconstructing the blood vessel using a graft, a surgical technique to replace or reinforce the vessels.
If pancreatic cancer is located in the body or tail of the pancreas, the surgeon would normally opt for a distal pancreatectomy with splenectomy, a procedure to remove the tail of the pancreas and spleen. For cases where there is significant involvement of the arteries that supply the stomach and spleen (celiac and splenic arteries), a modified Appleby procedure might be conducted if the patient meets certain criteria.
For both the Whipple procedure and distal pancreatectomy with splenectomy, minimal invasive surgeries are available and have been researched. These approaches have shown to have similar outcomes in terms of survival rates and risk of complications (morbidity and mortality), rendering them a viable option for some patients.
What else can Pancreatic Cancer be?
At the point when pancreatic cancer is initially diagnosed, about 52% of patients already have the disease spread to distant parts of the body, while 23% show the cancer has spread locally.
Before performing any imaging and biopsy, doctors often consider several other potential health conditions that may be causing the symptoms. These include:
- Acute pancreatitis
- Chronic pancreatitis
- Cholangitis (an infection of the bile duct)
- Cholecystitis (inflammation of the gallbladder)
- Choledochal cyst (a cyst in the bile duct)
- Peptic ulcer disease
- Cholangiocarcinoma (bile duct cancer)
- Gastric cancer (stomach cancer)
Surgical Treatment of Pancreatic Cancer
The method of first giving chemotherapy before surgery for treatable pancreatic cancer is becoming more common at major medical centers throughout the world. The idea behind this ‘neoadjuvant’ approach is that patients are physically in their best condition to handle chemotherapy prior to any surgical procedures and are more capable of completing the full course of 4 to 6 months of chemotherapy. The belief is that tissue is better oxygenated and not yet affected by a major procedure such as the Whipple procedure, a complex operation to remove the head of the pancreas. Since many patients are unable to start or finish post-surgical chemotherapy (known as adjuvant chemotherapy), this new approach could potentially extend their survival.
However, the SWOG 1501 Trial recently evaluated this ‘neoadjuvant treatment first’ strategy in treatable pancreatic cancer, but the results were not as anticipated. Only about 73% of patients who received chemotherapy before surgery went on to have surgical removal of the tumor. It was also observed that survival rates were similar to those of patients who received chemotherapy after surgery.
What to expect with Pancreatic Cancer
The outlook for pancreatic adenocarcinoma, a type of pancreatic cancer, continues to be challenging despite improvements in cancer treatment. The survival rate over a five-year period is roughly 20%. Sadly, one year after diagnosis, the survival rate falls significantly, with about 9 out of 10 patients not surviving, even with surgery.
However, palliative surgery – which is performed to relieve symptoms and improve quality of life, rather than to cure the disease – can still provide some benefit to these patients.
Possible Complications When Diagnosed with Pancreatic Cancer
After pancreatic surgery, there can be several complications. These include:
- Pancreatic fistulas, which are abnormal connections between the pancreas and other organs
- Delayed gastric emptying, where the stomach takes too long to empty its contents
- Anastomotic leaks, which are leaks in the connections between organs made during surgery
- Bleeding
- Infections
Recovery from Pancreatic Cancer
If you have stage IV pancreatic cancer that has spread to other parts of the body, it’s crucial to have a detailed talk about treatment possibilities with your doctor. One potential treatment is chemotherapy. However, it’s important to know that, while chemotherapy can prolong life, this extension would likely be measured in months rather than years, and there could be side effects you’ll need to consider.
Nutrition plays a key role in your care plan; it can influence how well your wounds heal. So, it’s paramount to focus on maintaining a good diet throughout your treatment. It’s all about balancing managing your cancer while also considering your overall wellbeing and quality of life.
Preventing Pancreatic Cancer
Before considering surgery, it’s crucial for the doctor and patient to explore all the available treatment options. This conversation allows the patient to fully understand their choices and be involved in the decision-making process about their health care.