What is Plasmacytoma?
Plasmacytoma is a rare type of disease that causes abnormal growth in plasma cells, which are a type of white blood cell. These abnormal growths can occur anywhere in the body, but they typically appear in the skeletal system or soft tissues as single or multiple growths. Importantly, they do not show signs of spreading throughout the body. Plasmacytoma is understood as an early form of plasma cell cancer, acting as a transitional phase between a harmless increase in these cells (monoclonal gammopathy of undetermined significance, or MGUS) and full-blown cancer (multiple myeloma, or MM).
The International Myeloma Working Group, a team of experts in this field, classify plasmacytoma into three types:
The first is Solitary Plasmacytoma, which is further divided into two types:
- Solitary plasmacytoma of bone (SPB) which originates from plasma cells in the bone marrow.
- Extramedullary plasmacytoma (EMP), which starts from plasma cells in the mucous membranes lining various parts of the body.
The second type is Multiple Solitary Plasmacytomas (MSP). This type involves many isolated abnormal growths in the body.
The solitary plasmacytoma type is the most common one, and often causes an abnormal protein to appear in the blood. This condition can spread to the soft tissues frequently and sometimes to the bones. It can be treated using surgery, radiation therapy, and chemotherapy. Treating the local area can result in a longer life span, while treating the spread disease can lead to longer periods without symptoms.
The World Health Organization (WHO) recognizes two subtypes of SPB:
- SPB with minimal bone marrow involvement – these have less than 10% abnormal cells in the marrow outside of the main growth. This type has a 20-60% chance of progressing to MM within 3 years.
- SPB with no bone marrow involvement – these have no abnormal cells in the marrow outside the main growth. This has a 10% risk of progressing to MM within 3 years.
As for the MSP type, it involves abnormal cell infiltration in one or more bone or tissue lesions. Only a few cases of this type have been reported. Medical imaging can reveal multiple growths which can lead to an MSP diagnosis. It is diagnosed in up to 5% of solitary plasmacytoma cases. It is unclear what the long-term outlook is for MSP. Treatments for this could include surgery, radiotherapy, chemotherapy, and even stem cell transplantation.
What Causes Plasmacytoma?
We don’t yet know what causes plasmacytoma, a type of cancer that affects plasma cells. However, some researchers suggest that extramedullary plasmacytoma (EMP), a specific type of this cancer, could be the result of breathing in harmful chemicals, being exposed to frequent or excessive radiation, having a viral infection, or due to certain genetic disorders in the reticuloendothelial system, which is a part of our immune system that helps ward off disease and removes waste from the body.
Risk Factors and Frequency for Plasmacytoma
Plasmacytoma is a unique condition, with the most common type being Solitary Plasmacytoma of Bone (SPB). It isn’t a frequent disease and pops up in less than 450 cases every year. SPB is found 40% more often than Extra-medullary Plasmacytoma (EMP), though they make up only a small part of all plasma cell malignancies. It typically surfaces in older people, with an average age of 55 to 60 years. Plasmacytoma is more common in African Americans, males, and seems to occur twice as much in males with SPB and three times more in those with EMP.
- Plasmacytoma is not a form of disease seen often, with less than 450 cases annually.
- SPB, the most common type of Plasmacytoma, is 40% more common than EMP.
- Both SPB and EMP make up only a small fraction of all plasma cell malignancies.
- Plasmacytoma usually occurs in older individuals, around 55 to 60 years of age.
- The disease is more commonly seen in African Americans and in males.
- The male to female case ratio is 2:1 for SPB, and 3:1 for EMP.
Signs and Symptoms of Plasmacytoma
Individuals with SPB often experience pain in bones where red bone marrow is found, for instance, ribs, the spine, thigh bone, and pelvis. Sometimes, it might manifest in less common ways, such as headaches, double vision, misalignment of the eyes, an outward-growing mass, earache, and dizziness due to its involvement in the skull. Damaged bones may also lead to compression fractures or local soft tissue damage. If the spine is significantly involved, it could affect the spinal cord or root nerves.
EMP, another form of the condition, can occur anywhere in the body, but most commonly, 80% to 90% of cases, in the head and neck region, particularly in the oral cavity, the depression behind the tonsils, nasal cavity, and the air-filled spaces around your nose, called paranasal sinuses. Symptoms may include headache, nasal discharge, difficulty swallowing, sore throat, nosebleeds, and blockage of the nasal passage.
- Headache
- Nasal discharge
- Difficulty swallowing
- Sore throat
- Nosebleeds
- Nasal obstruction
In rare instances, the larynx or voice box may be affected, leading to symptoms such as a hoarse voice, changes in vocal tone, difficulty breathing, blocked airway, and wheezing.
Although it is seldom seen, the gastrointestinal tract may be involved too, leading to upper stomach pain, coughing up blood, loss of appetite, bleeding, and abdominal discomfort. There have been less than a dozen reported cases where the part of the abdomen that carries blood and lymph vessels to the intestines (the mesentery) was involved.
Lastly, in rare cases, plasmacytoma may mimic a lung tumor and present as a lump in lung tissues or near the area that connects the lungs (perihilar) associated with swollen lymph nodes in the chest (mediastinal lymphadenopathy). Radiographically, it may appear to be damage along the air-filled spaces in the lungs (alveolar interstitial) or part of the respiratory tract (endobronchial). It could also rarely occur in the thyroid, causing it to enlarge (thyromegaly).
Testing for Plasmacytoma
When it comes to diagnosing conditions like plasmacytoma (a type of tumor that grows in plasma cells), doctors use a variety of lab tests and diagnostic techniques. One of these is checking for the presence of certain proteins called monoclonal proteins in your blood or urine. Doctors expect that no M-protein should be noticed on the lab tests for this condition. However, about half of patients may still show a small amount of M-protein.
Other parts of these tests might include checking the levels of various other substances in your blood, which should usually be within the normal range.
Another way in which the doctors check for the disease is through biopsy – a procedure where a small sample of tissue is taken from the body so it can be examined more closely. Doctors might use a method called fine-needle aspiration or they might collect the sample during a minor surgical procedure. Depending on your situation, the doctor might need to use special tools or equipment to collect the sample. For example, if the suspected tumor is in the spine, imaging methods like fluoroscopic or CT guided techniques are employed.
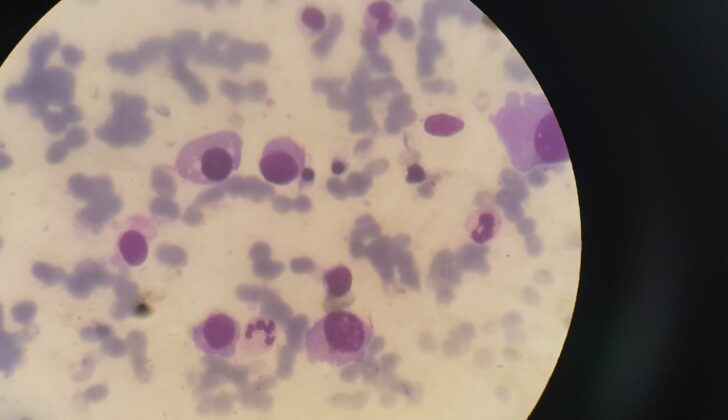
Once the sample is taken, it is investigated under a microscope. The lab checks for certain signs, like the infiltration of monoclonal cells or submucosal growth. The sample might also be tested for the presence of substances called CD138 and CD38 markers.
In addition to lab tests and biopsy, doctors also employ imaging studies to determine the diagnosis. These might involve plain film radiography (a method by which images of the bones are obtained by passing small, controlled amounts of X-ray radiation through the body), magnetic resonance imaging (MRI), or positron emission tomography (PET) scans. MRI is particularly useful as it provides clear, detailed images that help doctors measure the size of the tumor and its stage. Doctors might also use this imaging method to check whether treatment is causing the tumor to shrink.
Endoscopy, a procedure which involves the use of a flexible tube with a light and camera attached to it, is another tool doctors use to detect any associated conditions or any damage to the surrounding tissues.
Patient evaluation does not stop at diagnosing the primary condition. The next step includes ruling out other systemic diseases or conditions like multiple myeloma (a type of cancer that occurs in infection-fighting cells), by having further tests like a skeletal survey, bone marrow biopsy, flow cytometry (a technology that is used to analyse the physical and chemical characteristics of particles in a fluid as it passes through at least one laser), and checking immunoglobulins and free light chain levels.
An important part of diagnosing plasmacytoma is ruling out the presence of any end-organ damage, which means checking if the disease has impacted function of any organs like the kidneys, heart, liver, or lungs.
Treatment Options for Plasmacytoma
Plasmacytoma is a type of cancer that’s generally treated using radiation therapy, surgery, and sometimes chemotherapy. The selection of treatments will depend on the specifics of each individual case.
Radiation therapy is often the go-to treatment because plasmacytomas tend to be sensitive to this method. This form of treatment has an impressive success rate, with about 80% of cases being brought under control. Patients typically undergo radiation therapy over a course of 4 weeks, receiving several small doses which add up to a total of 40-50 Gy, a unit to measure the amount of radiation. The process uses specific techniques to target the tumor accurately, while avoiding damage to sensitive areas like the eyes and glands.
The area targeted by radiation includes the tumor itself and a small margin around it that’s tumor-free, to ensure all cancerous cells are covered. In certain cases, the whole bone might be included for treatment due to the risk of recurrence. For cases where the tumor is in the spine, the radiation field will also cover one or two vertebrae above and below the affected area. Lymph nodes might be included in the treatment field if the disease has spread there. While including unaffected lymph nodes can reduce the recurrence rate, it can also lead to an increase in related side-effects so it’s typically avoided.
Surgery can be used for diagnosis by removing partial or entire tumors. When used alongside radiation therapy for treatment purposes, it can lead to better chances of the disease not progressing further. However, where the tumors are in the head or neck region, surgery should be used sparingly, because these tumors tend to respond very well to radiation and surgical procedures in these areas can be disfiguring. Surgery can also be useful for dealing with spinal instability, fractures, or neurological issues caused by the tumor. Surgery on its own, however, can increase chances of the disease coming back.
Chemotherapy, a treatment using drugs to kill cancer cells, hasn’t shown significant benefits in controlling the disease or preventing complications in most studies. While it doesn’t reduce the chances of plasmacytoma developing into multiple myeloma, another type of cancer, it does slow down the progression towards it. Chemotherapy might be considered for tumors larger than 5cm or those not responding to radiation therapy.
In some high-risk, recurrent, or large cases of plasmacytoma, a treatment called Autologous Stem Cell Transplantation (ASCT) might be considered. This involves extracting a patient’s own stem cells, treating the patient with high-dose chemotherapy to kill the cancer cells, and finally reintroducing the stem cells back into the body. Studies conducted on patients with recurring or high-risk plasmacytoma have shown promising results from this form of treatment.
What else can Plasmacytoma be?
Differentiating plasmacytoma, a type of tumor, from similar diseases is essential for an accurate diagnosis. These diseases include:
- Multiple Myeloma (MM): A tumor of plasma cells. Plasmacytoma could develop into multiple myeloma in 2-3 years. Medical professionals distinguish plasmacytoma from multiple myeloma when the latter shows signs such as high levels of calcium in the blood, kidney failure, anemia, bone disease, multiple bone lesions, organ damage, and proteins in the blood or urine.
- Non-Hodgkin Lymphoma (NHL): This condition may show signs similar to plasmacytoma, making it challenging to distinguish between the two. Immunophenotyping, which identifies specific types of cells, can be helpful in telling them apart.
- Reactive Plasmacytosis: This condition is associated with excessive growth of certain white blood cells. Unlike plasmacytoma, reactive plasmacytosis doesn’t result in overproduction of certain light chain proteins.
- Plasmablastic Lymphoma: Marked by a tumor with plasmablastic morphology, often showing up in individuals with HIV or those with suppressed immune systems. It typically appears in the oral cavity or the other areas of the head and is associated with the Epstein-Barr virus (a common human virus).
Thorough examination and testing can allow healthcare providers to successfully tell these diseases apart.
What to expect with Plasmacytoma
The median time it takes for Solitary bone plasmacytomas (SBP) to turn into Multiple Myeloma (MM), a type of cancer, is typically 2 to 3 years. SBP has a less favourable prognosis, or predicted outcome, and is more likely to turn into MM compared to Extramedullary Plasmacytomas (EMP). Specifically, around 50% of SBP cases develop into MM, whereas only 15% of EMP cases do.
Things that can lead to a poor prognosis include local recurrence (the cancer coming back), incomplete surgery with functional damage, the cancer spreading to local lymph nodes, the development into MM, or the creation of new bone lesions with MM. Also, if the cancer cells appear abnormal (anaplastic) and move around quickly due to increased blood flow, the prognosis tends to be worse. For SBP, the factors that could worsen the prognosis include:
1. Being over 40 years old
2. The cancer growing to 5cm or more
3. Having spine lesions
4. Having neurological symptoms related to SBP
5. Receiving a certain dose of Radiotherapy (RT)
6. The presence of light chains (parts of antibodies in blood)
7. High levels of serum M protein (a marker for MM)
8. Continuation of M proteins after treatment
9. Bone marrow infiltration by clone plasma cells (cancerous blood cells invading the bone marrow)
10. Having Osteopenia (decreased bone density)
However, for EMP, the factors that could worsen the prognosis are not as clear due to the fewer cases and changing biological behavior. Some potential factors are age, tumor size and grade, whether the cancer originated in the bone or elsewhere, if the cancer has spread to regional lymph nodes, high levels of serum M-protein and light chains, and a certain dose of radiation.
Possible Complications When Diagnosed with Plasmacytoma
: Plasmacytoma, a type of tumor, can manifest anywhere in the body, causing a variety of complications.
For instance, a type of plasmacytoma called SPB often causes breakdown of the bones, which leads to bone pain, fractures, and damage to surrounding nerves and soft tissues.
A specific disorder, known as POEMS syndrome, is associated with certain types of plasmacytoma. This condition includes nerve damage (polyneuropathy), enlarged organs (organomegaly), hormone imbalances (endocrinopathy), multiple myeloma bone disease, and skin changes.
Plasma cell disorders like plasmacytoma produce a type of protein called immunoglobulins, which can reduce the body’s immune response to antigens, making the body less effective at fighting off diseases.
Kidney problems could also be linked to plasmacytoma, especially if it produces light chains, a type of protein that can cause kidney damage when they are eliminated as Bence–Jones proteins in the urine. This was observed in a 44-year-old man with a chest wall plasmacytoma. Moreover, conditions like cryoglobulinemia and amyloidosis, seen in some cases of chronic Hepatitis C and plasmacytoma, could stem from these light chain proteins.
In some instances, plasmacytoma has also been associated with bleeding in the digestive system, a condition seen in some cases of multiple myeloma. There have been rare incidents where a type of plasmacytoma called extramedullary plasmacytoma has created ulcers in the lining of the stomach, leading to severe upper gastrointestinal bleeding. These cases can also lead to obstruction and ruptures in the digestive system.
Finally, it’s worth noting that if the person is receiving treatment with a drug called melphalan, they might experience side effects such as drug toxicity. This toxicity can lead to the development of severe conditions like acute leukemia and systemic infection (sepsis), especially when the treatment reduces the number of infection-fighting white blood cells (neutropenia). There have also been reports of blood clots linked to thalidomide treatment.
- Plasmacytoma
- Bone pain, fractures, and nerve & soft tissue damage
- POEMS syndrome
- Weakened immune response
- Kidney issues
- Cryoglobulinemia and Amyloidosis
- Gastrointestinal bleeding
- Obstruction and ruptures in the digestive system
- Drug toxicity, acute leukemia, and systemic infection
- Blood clots
Recovery from Plasmacytoma
When treating a disease called plasmacytoma, patients need continuous monitoring for their entire life. The first six months involve regular check-ups every six weeks, before spacing out into less frequent appointments. These check-ups usually involve various tests including blood tests, health checks for kidney and liver, C reactive protein (a marker of inflammation in the body), erythrocyte sedimentation rate (a test that measures how quickly red blood cells settle at the bottom of a test tube, which can indicate the presence of a disease), M protein (abnormal proteins produced by cancer cells) and a skeletal bone survey (an x-ray of all the bones in the body).
According to the National Comprehensive Cancer Network, it is advised that patients should undergo imaging tests using the same techniques as those used at diagnosis, once every year for five years. Also, for patients with forms of plasmacytoma known as solitary plasmacytoma of bone (SPB) and extramedullary plasmacytoma (EMP), additional regular check-ups are advised with the orthopedics and ear, nose, throat departments respectively.
Preventing Plasmacytoma
Teaching patients about their condition is crucial because it helps them better comprehend their health issue and seek the right treatment. For those diagnosed with plasmacytoma (a type of tumor formed by plasma cells), the discussion topics include:
* Understanding the disease – This helps you grasp what plasmacytoma is and how it affects your body.
* Disease workup – This refers to the various tests and procedures doctors use to confirm a diagnosis of plasmacytoma.
* Complications of the disease – This explains the possible health problems or complications that can occur due to plasmacytoma.
* Possible treatment options and outcomes – These help you understand the different ways to treat plasmacytoma and what you might expect after going through these treatments.
* Possibility of disease recurrence and progression – This informs you about the chances that the plasmacytoma could come back or grow worse over time.
* Counseling about long term followup – This ensures that you know the importance of regular checkups with your doctor, even after treatment for plasmacytoma is completed. Regular follow-ups help monitor your health status and react promptly if the disease returns or progresses.