What is Seminoma?
Testicular neoplasm, or abnormal growth in the testicle, is one of the most common causes of a lump or mass in the testicle. It affects around 5 in 100,000 men, mainly between the ages of 15-34 years. A type of testicular cancer called seminoma, which can commonly be found in the testicle or less frequently in other parts of the body such as the mediastinum, retroperitoneum, or other extra-gonadal sites (meaning outside of the reproductive organs), is one of the cancers that can be treated and cured, especially when caught early. In fact, the survival rate is over 95% when discovered in the early stages.
Types of testicular cancer, also known as testicular germ cell tumors (GCTs), have different subtypes, which include seminoma, teratoma, choriocarcinoma, embryonal, and yolk sac carcinoma. Seminoma and nonseminoma are the two main categories, and they require different treatment approaches. A tumor is classified as a ‘pure seminoma’ after detailed investigation under a microscope, known as histopathological review. However, if any elements of nonseminoma are found (even if the majority of the tumor is seminoma), the classification is changed to nonseminoma. This is important because it helps doctors decide the best treatment option.
What Causes Seminoma?
The exact cause of seminoma, a type of testicular cancer, is still not clear. However, certain factors are known to increase a person’s risk of developing this condition:
* History of cryptorchidism: Cryptorchidism is a condition where one or both testes fail to descend. If you have a history of this condition, you’re at a higher risk of developing seminoma – up to 10 to 40 times higher, in fact. Interestingly, it’s noted that an undescended testis is more likely to develop seminoma, whereas a testis that has been surgically moved down to the scrotum is more likely to develop a different type of cancer.
* Exposure to certain chemicals: Being exposed to specific chemicals, such as those found in plastics (organochlorines, polychlorinated biphenyls, polyvinyl chlorides, phthalates), and even substances in tobacco and marijuana, could increase your risk of developing seminoma or other types of testicular cancer.
* Having had certain infections: If you’ve had infections like mumps, this could increase your risk of developing testicular cancer.
* Other factors: Various other circumstances might increase your risk, such as having had trauma to the testes, being exposed to excessive estrogen while in the womb, having a family history of testicular tumors, suffering from certain medical conditions (like androgen insensitivity syndrome), and having had cancer in the opposite testicle.
* Genetic factors: Certain genetic changes, specifically those found in the 12p11.2-p12.1 regions of a chromosome, have been linked to seminoma. Moreover, it’s been observed that seminomas often contain activating mutations of the KIT gene.
Risk Factors and Frequency for Seminoma
Testicular germ cell tumors (GCTs) are the most common type of cancer in men aged 15 to 34 years. However, they make up less than 1% of all male cancers. Over the past 20 years, there has been an increase in testicular tumors. In the United States, the most common type of testicular cancer is testicular seminoma. It is more common in Whites than in African Americans, and the rate has been rising in the White population in recent times.
- The most common cancer in men aged 15 to 34 is testicular germ cell tumors.
- These tumors make up less than 1% of all male cancers.
- The number of testicular tumors has been increasing over the past 20 years.
- The most common type of testicular cancer in the United States is testicular seminoma.
- Whites are more likely to develop seminoma than African Americans.
- The rate of seminoma has been rising in the White population in recent times.
Signs and Symptoms of Seminoma
Seminoma, a type of testicular cancer, often shows up as a lump or painless swelling in the testes. Sometimes, the person or his partner discovers it by accident. Some men may feel a dull ache or heaviness in their lower stomach, near their buttocks, or in their scrotum. Occasionally, the first signs of this condition could be sudden pain, bloody semen, loss of appetite, or vomiting. If the disease has spread to other parts of the body, symptoms can vary based on the affected area. For example, neck lumps, coughing, difficulty breathing, gastrointestinal bleeding, or bone pain can occur. Sometimes, the cancer can affect the nerves, leading to problems with the brain, spinal cord, or peripheral nerves. A history of undescended testes and surgical correction may also be present in some of these cases.
- Lump or painless swelling in the testes
- Dull ache or heaviness in the lower abdomen, perineal area, or scrotum
- Sudden pain or bloody semen
- Loss of appetite
- Vomiting
- Neck lumps (if the disease has spread to the neck)
- Coughing or difficulty breathing (if the disease spread to the lungs)
- Stomach bleeding (if the disease spread to the stomach or duodenum)
- Bone pain (if the disease spread to the bones)
- Problems due to nerve involvement (if the disease spread to the brain, spinal cord, or peripheral nerves)
- History of undescended testes and surgical correction
Testing for Seminoma
If your doctor suspects there might be a growth on one of your testicles (a testicular mass), they’ll need to run a few tests and scans. This is called your ‘initial workup’. The first part of this workup involves some blood tests, which measure levels of certain ‘tumor markers’, including alpha-fetoprotein (AFP), beta-human chorionic gonadotropin (beta-HCG), and lactate dehydrogenase (LDH).
These markers can tell your doctor about the nature of the growth. For example, high levels of beta-HCG and LDH, but not AFP, might indicate a kind of testicular cancer called a seminoma. LDH isn’t a very specific marker, meaning it can be raised by lots of different conditions, not just cancer. But, a high level can suggest you have a large tumor. While beta-HCG is only raised in a small proportion of people with seminomas, a high level can suggest that the cancer has spread, or ‘metastasized’. Interestingly, how high your beta-HCG level is doesn’t seem to affect chances of survival overall. Your doctor might also check for another protein called ‘placenta-like alkaline phosphatase’- especially if the tumor is large. This protein can also appear in higher levels if you’re a smoker.
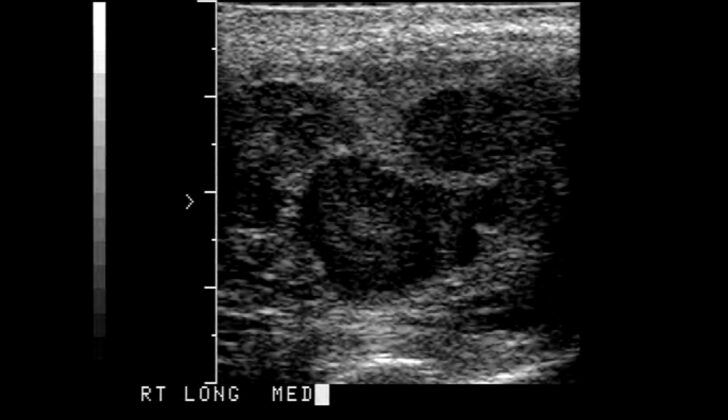
The next step in your workup is an ultrasound of your scrotum. This can help your doctor rule out other conditions that might be causing the growth. If you have a seminoma, the ultrasound will usually show a uniformly dense mass within the testicle. If the tumor is large, it might look patchy on the scan. Seminomas generally don’t contain liquid-filled regions called ‘cystic areas’, or hard nodules of calcium, called ‘calcifications’, as often as other types of testicular cancer.
To make sure that what they’re seeing is really a seminoma, your doctor will need to remove the affected testicle in a procedure called an ‘orchiectomy’. This also serves to treat the cancer. Then they’ll look at the tissue under a microscope and run tests on it to confirm the diagnosis.
If your test results suggest the cancer might have spread to other parts of you body (metastasized), or the stage of the cancer means this could be a possibility, your doctor might arrange for a series of other scans. These include a chest CT scan or x-ray, an abdominal and pelvic CT scan, an MRI of your brain, and a bone scan. If you’re given chemotherapy to treat the cancer, a type of scan called a PET scan can check if the treatment is working, and spot any recurrences of the cancer.
To understand how advanced the cancer is (its ‘stage’), your doctor will also use a specific ‘staging system’. The ones used most often come from the Americal Joint Commission on Cancer (AJCC) and the International Union Against Cancer (IUAC). However, these don’t take into account the tumor marker levels in your blood if you have a seminoma. Instead, they’re more interested in whether the cancer has spread to organs other than the lungs.
Treatment Options for Seminoma
Radical orchiectomy, a surgical procedure to remove one or both testicles, is the main treatment for all stages of seminoma, a type of testicular cancer. This surgery provides a diagnosis and also acts as a treatment. Following the surgery, additional treatments like chemotherapy or radiation may be advised based on the specific stage of the patient’s disease.
For Stage I seminoma patients, the surgery is usually all that’s needed and provides a cure in most cases. After the surgery, doctors may regularly monitor the patient or recommend additional treatment such as a one-time chemotherapy treatment or radiation. However, the use of radiation is becoming less common.
For patients with Stage II seminoma, the treatment varies based on how much the cancer has spread to the lymph nodes. The treatment mainly consists of radiation with or without chemotherapy that usually contains a drug called cisplatin.
For Stage III patients, the common treatment plan includes chemotherapy with a combination of three drugs: bleomycin, etoposide, and cisplatin (BEP). Sometimes, only two of these drugs, etoposide and cisplatin (EP), are used. In some situations, radiation could be applied. If certain patients have difficulties tolerating bleomycin, an additional drug called ifosfamide can be added to the other two drugs in a combination called VIP.
After treatment, patients need lifetime follow-ups. The frequency of these check-ups is determined by the stage of the disease and how long it’s been since treatment. These follow-ups generally include regular medical exams, blood tests to measure tumor markers (substances linked to cancer), chest x-rays, and CT scans of the abdomen, with or without CT scans of the pelvic region. These steps will help healthcare providers monitor recovery, review the effectiveness of the treatment, and ensure early detection of any signs of the disease returning.
What else can Seminoma be?
If a patient might have seminoma (a type of testicular cancer), doctors have to consider several other conditions that can look very similar when they examine tissue samples under a microscope. These include:
- Non-seminomatous germ cell tumor, which includes types like embryonal carcinoma, cholangiocarcinoma, yolk sac tumor or teratoma
- Leydig and Sertoli cell tumors
- Granulosa cell tumors
- Gonadoblastoma
- Lymphoma
- Mesothelioma
- Adenocarcinoma of the rete testis
- Epidermoid cyst
- Metastatic carcinoma (cancer that has spread from another part of the body)
- Epididymitis (inflammation of the epididymis, a tube located at the back of the testicles)
- Hydrocele (a type of scrotal swelling)
Surgical Treatment of Seminoma
Radical inguinal orchiectomy, or surgical removal of one or both testicles through the groin, is the standard treatment for diagnosing and managing testicular cancer. Doctors avoid performing a biopsy or removing the testicle through the scrotum due to the risk of spreading cancer cells along the path of lymphatic drainage, which is how fluids travel through the body to the immune system.
Spinal or general anesthesia, which blocks pain in the entire body and keeps you asleep during the procedure, may be used. A cut is made in the patient’s groin to uncover the external and internal iliac canal, which are pathways in the lower abdomen. The external iliac fascia, a layer of tissue in the abdomen, is opened up which shows the spermatic cord. The spermatic cord is then blocked off to prevent the spread of cancer cells in the body via lymphatic and venous drainage.
Next, the testicle is brought out from the scrotum and separate ties are made around the tube that carries the sperm (vas deferens) and the spermatic arteries. If necessary, removal of lymph nodes in the lower back area – also known as retroperitoneal lymph node dissection – is performed.
The external oblique fascia, a muscle in the lower abdomen, is brought back together and the skin is stitched shut in the usual way. The patient’s condition and healing are monitored through regular check-ups, and they are guided towards the next steps in treatment, such as further therapies if needed.
What to expect with Seminoma
According to data shared by the American Cancer Society, which they obtained from the Surveillance, Epidemiology, and End-Results (SEER) database, the five-year survival rates for testicular cancer are as follows:
* In its early stage (stage I), where the disease is still localized, the survival rate is 99%.
* In stage II, where the disease has spread to nearby regions, the survival rate is 96%.
* In stage III, where the disease has spread to distant parts of the body, the survival rate is 73%.
Please note that with testicular cancer, there’s a higher chance of developing other cancers due to factors like the early age of diagnosis, the high rate of successful treatment and exposure to radiation or chemotherapy. This could potentially lead to cancers such as malignant mesothelioma (a type of cancer affecting the thin tissue lining most of your internal organs), or cancers of the lung, colon, bladder, pancreas, and stomach.
Possible Complications When Diagnosed with Seminoma
People who have had testicular cancer and received radiation therapy or chemotherapy often experience long-term complications. Given these individuals often live over 40 years post-therapy, these complications can greatly affect their quality of life.
- Chemotherapy-related nerve damage: A common side effect of platinum chemotherapy is peripheral neuropathy. This condition, which might cause pain and permanent sensory changes, can occur in about 20 to 40% of patients.
- Heart problems: Testicular cancer survivors that had chemotherapy involving a drug called cisplatin are up to seven times more likely to develop heart issues.
- Infertility and low testosterone: Chemotherapy and radiation therapy to the scrotum can cause a decrease in sperm count or complete infertility. Therefore, it’s crucial to inform all patients about the possibility of storing their sperm before starting treatment. The risk of becoming infertile directly correlates with the intensity and duration of treatment. Additionally, common testicular dysfunction or hypogonadism can occur in testicular cancer survivors.
- Hearing loss: Cisplatin can also cause permanent, sensorineural hearing loss and ringing in the ears (tinnitus).
- Second type of cancer: Another potential risk from both chemotherapy and radiotherapy is the development of secondary cancers. For example, a drug called Etoposide can lead to treatment-related leukemia, and the risk increases based on the dosage.
Recovery from Seminoma
After a procedure called radical inguinal orchiectomy, patients are starting to get an additional surgery to receive a prosthetic testicle. This operation is similar to a surgery for treating an inguinal hernia. For a short period after surgery, the patient should limit their physical activity. Pain relievers may be needed for a short time to help manage any discomfort. Although complications are not common, they can occur. These can include infection in the surgical wound, building up of blood within the wound (hematoma), risks related to anesthesia, and numbness of the skin in the groin area.
For patients diagnosed with a type of testicular tumor called seminoma, it’s important to periodically check on their condition even after the tumor has been removed. This is known as surveillance.
The check-ups and scans required differ based on the patient’s clinical stage and the initial treatment they received. A chest x-ray may be advised at any time within five years if deemed necessary. If symptoms arise, a more detailed scan of the chest using a CT scanner and contrast agent may be needed. Checking for substances produced by cancerous cells, known as tumor markers, in the blood is optional during surveillance.
There’s a detailed schedule for these surveillance procedures depending on the specific situation of the patient:
If the patient had only the orchiectomy:
* In the first year, a health check-up and CT scan of the abdomen (and possibly also the pelvis) have to be done every 3-6 and at 3, 6, 12 months respectively.
* In the second and third year, similar check-ups and scans are required but can be done every 6-12 months.
* In the fourth and fifth year, the health check-up should be done annually and the CT scan every year or two.
If the patient had additional therapy (like chemotherapy or radiation) after the orchiectomy:
* For the first two years, a health check-up is needed every 6-12 months and a CT scan of the abdomen (and maybe the pelvis) is needed annually.
* In the second and third year, these procedures should be done annually.
* In the fourth and fifth year, the patient only needs a health check-up annually.
If the patient had radiation or chemotherapy after the orchiectomy and their initial diagnosis was a stage IIA or a non-bulky IIB seminoma:
* In the first year, a health check-up is needed every three months and a CT scan of the abdomen (and maybe the pelvis) is needed at three months and then every 6-12 months. A chest x-ray should also be taken every six months.
* For the second year, the health check-up and x-ray are needed every six months and a CT scan is needed annually.
* By the third year, only the health check-up and CT scan are needed, both to be done every six months.
* For the fourth and fifth year, a health check-up should be done every six months and a CT scan as needed.
If the patient has had chemotherapy for a bulky IIB, IIC, or stage III seminoma:
* In the first year, a health check-up and blood test for tumor markers every two months, a CT scan of the abdomen and pelvis every four months, and a chest x-ray every two months are needed.
* For the second year, these procedures are needed but the intervals are slightly longer – three months for the check-up and x-ray, and six months for the scan.
* For the third and fourth year, the check-up and blood test are needed every six months, the x-ray annually, and a CT scan as described before.
* By the fifth year, these procedures are needed annually, a check-up, blood test, and x-ray. The CT scan is only required as necessary.
Preventing Seminoma
Currently, there’s no reliable test to detect testicular cancer early. So, it’s crucial, especially for young people, to regularly check themselves. Early detection leaves a great chance for successful treatment. So, people with a family history of testicular cancer or a history of undescended testicles should be especially encouraged to frequently self-check.
It’s also important for all men of the age group that can father a child to think about freezing their sperm as a precautionary step. This discussion should happen before any treatments that might affect their ability to have children in the future are started. These treatments could be the removal of a testicle (orchiectomy), chemotherapy, or radiation therapy. If a patient wants to store his sperm, it can be done before or after surgery but must be completed before any radiation or chemotherapy treatment begins.