What is Squamous Cell Lung Cancer?
Squamous cell lung cancer is a subtype of non-small cell lung cancer (NSCLC), a group of lung cancers that are named after how the cells look under a microscope. Among this group, adenocarcinoma is the most common type, but squamous cell lung cancer also occurs quite frequently, especially in women. This has been linked to changes in patterns of cigarette smoking, but more evidence is needed to confirm this. Squamous cell lung cancers most often occur in the center of the lungs or in the main airway, which includes the left or right bronchus.
The primary cause of squamous cell lung cancer is smoking. In fact, about 80% of cases in men and 90% of cases in women are connected to smoking. This type of cancer is more strongly linked to smoking than any other type of non-small cell lung cancer. Other risk factors can include age, family history, exposure to second-hand smoke, and occupational exposures such as certain minerals, metal particles, or asbestos.
People with non-small cell lung cancers, including squamous cell lung cancer, may experience symptoms like a cough, chest pain, shortness of breath, bloody phlegm, wheezing, a hoarse voice, frequent chest infections (like bronchitis and pneumonia), weight loss, a loss of appetite, and fatigue.
Once a doctor suspects lung cancer, they often use a type of imaging test called a computed tomography (CT) scan to get a better look. If the tumor is large enough, it can often be seen on this scan. Doctors may also use other tests, including looking at the tissue under a microscope and testing the cells for certain markers, to confirm the diagnosis and figure out how advanced the cancer is. The treatment for squamous cell lung cancer can vary and will depend on the stage of the cancer. Common treatment options include surgery to remove the tumor, chemotherapy, radiation therapy, and immunotherapy, which is a type of treatment that helps your immune system fight the cancer.
What Causes Squamous Cell Lung Cancer?
About 80% of lung cancer cases in men and 90% in women are linked to smoking. Smoking is connected to a type of lung cancer called Squamous Cell Carcinoma (SCC) more than any other type. SCC risk can also increase with age, having a family history of the disease, being exposed to second-hand smoke, or coming into contact with certain materials like minerals, metal particles, and asbestos.
Risk Factors and Frequency for Squamous Cell Lung Cancer
In 2023, lung cancer was one of the most common types of cancer and the top cause of cancer-related deaths in the US according to the National Cancer Institute’s Surveillance Epidemiology and End Results database. Around 238,340 cases were reported, which made up 12% of all cancer cases in the country. Additionally, there were about 127,070 deaths from lung cancer, of which accounted for roughly 21% of all cancer-related deaths.
- About 85% of all lung cancers are a type known as NSCLCs.
- The most common subtypes of NSCLC are adenocarcinoma and squamous cell carcinoma.
- These two subtypes make up 50% and 30% of NSCLC cases, respectively.
Signs and Symptoms of Squamous Cell Lung Cancer
Non-Small Cell Lung Cancers (NSCLCs) often show a variety of symptoms which includes:
- Cough
- Chest pain
- Shortness of breath
- Blood in sputum
- Wheezing
- Hoarseness
- Recurring chest infections (like bronchitis and pneumonia)
- Weight loss
- Loss of appetite
- Fatigue
Though, in the early stages of the disease, patients with NSCLC often may not show these symptoms. The person’s social history might reveal a lot of smoking or being exposed to harmful substances at work, such as heavy metals, asbestos, and radon gas. In advanced stages of NSCLC, the cancer might spread to other parts of the body causing other symptoms such as:
- Bone pain
- Brain metastasis
- Spinal cord compression with related neurologic symptoms like headache, weakness or numbness of limbs, dizziness, and seizures.
Testing for Squamous Cell Lung Cancer
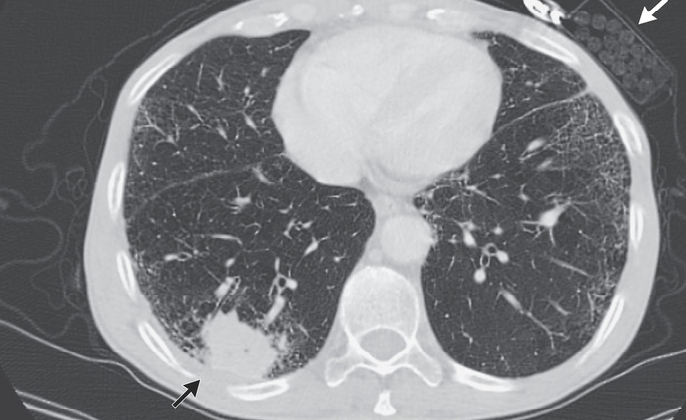
After your doctor examines you, they often use a type of scanning technology called a computed tomography (CT) scan to further investigate squamous cell carcinoma (SCC), which is a type of cancer. Your doctor will look for signs of SCC during this scan. These signs could be a space filled with gas or fluid within the mass, or a lump, which could point towards SCC. They may also find signs like lung nodules (small growths in the lungs), a wider mediastinum (the space between the lungs), lung collapse (atelectasis), enlarged lymph nodes near the lungs, or fluid in the space that surrounds the lungs.
When a patient is suspected to have lung cancer, a thorough examination is completed to assess how far the disease has spread. For small nodules found incidentally on a CT scan, doctors usually follow management guidelines from the Fleischner Society. If lung cancer is likely, your doctor may prefer to proceed with staging – assessing how far cancer has spread – before taking a tissue sample for biopsy. The benefit of this approach is identifying any areas where cancer has spread, which may be easier to biopsy, thus confirming both the diagnosis and how advanced the disease is.
High-quality imaging is vital in this process. Usually, scans known as Positron Emission Tomography (PET), combined with a CT scan, are used. However, these scans can sometimes falsely indicate the presence of cancer when in fact it’s something else. Deciding not to use PET/CT scans is a possibility when dealing with specific types of tumors or lesions. For instance, MRI brain scans are only necessary when checking for cancer that has spread to the brain in patients with stage II of the disease or higher.
Despite advancements in imaging technology, doctors sometimes use invasive procedures to examine lymph nodes in the chest (mediastinum) more accurately, given that even with PET/CT scans, they can sometimes incorrectly indicate or miss disease in the mediastinum. The need for such invasive staging procedures primarily depends on the results of your CT and PET scans. The procedure may be avoided for patients with proven metastatic disease and those with other specific conditions.
Other diagnostic procedures can also be used to sample the mediastinum, with different techniques able to reach different locations. Some of these include mediastinoscopy, video-mediastinoscopy, and video-assisted thoracic surgery. Ultrasound techniques can also be used, such as endoscopic bronchial ultrasound with needle aspiration (EBUS-NA) and esophageal ultrasound with needle aspiration (EUS-NA).
Before deciding on the best treatment, patients are usually offered a baseline pulmonary function test (PFT), especially those who might be candidates for surgery. Additionally, genetic testing for PD-L1 status and EGFR mutations is done since specific therapies can target these genetic changes. It’s worth noting that EGFR mutations in SCC are rare, and believed to occur in less than 5% of cases.
Treatment Options for Squamous Cell Lung Cancer
The treatment for cancer depends on how advanced the disease is. In the early stages (Stages I and II), surgery is the standard treatment. If the cancer mass is small, patients might not require further treatment after surgery. However, in some cases where the tumor is larger, chemotherapy might be added after surgery to ensure any remaining cancer cells are eliminated. If the patient isn’t an ideal candidate for surgery, a smaller portion of the lung might be removed instead of the whole lobe. Radiation therapy also comes into the picture if cancer cells remain in the body post-surgery or if the patient can’t undergo surgery.
Stage III cancer is usually too advanced for surgery. For these situations, a combination of chemotherapy and radiation therapy is commonly used. Recent studies also suggest including chemoimmunotherapy (a treatment that combines chemotherapy with activating the immune response) before, during, or after surgery. In more advanced Stage III cancer, chemotherapy and radiation are followed by immunotherapy, which helps the body’s immune system to fight off cancer.
In the last stage, Stage IV, the cancer has often spread to other parts of the body, and the focus of treatment shifts to making the patient comfortable (palliative care). Treatment in this stage typically involves radiation and medication.
In more specific cases, targeted therapies are used to precisely aim at the cancer cells. If the cancer shows specific genetic changes (like somatic-driven mutation), drugs designed to inhibit these changes are used. For example, drugs like erlotinib, gefitinib, and afatinib target and inhibit the mutated epidermal growth receptor in non-small cell lung cancer (NSCLC), effectively stopping cancer growth. Also, the use of immunotherapy (where drugs help the immune system fight cancer) might be considered based on several factors like the presence of certain markers on cancer cells (programmed cell death-ligand 1 or PD-L1) or pre-existence of certain genetic changes. In cases where strong reactions to drugs due to autoimmune diseases are expected, only chemotherapy is recommended.
For advanced cancers, treatment depends on additional genetic and molecular testing. A variety of therapies can be tailored to individual patients based on these tests. Based on the presence of specific markers or mutations, different combinations of chemotherapy, immunotherapy, and targeted therapy drugs can be used singly or in combination depending on individual patient factors.
What else can Squamous Cell Lung Cancer be?
When dealing with SCC (Squamous cell carcinoma) of the lung, it’s critical to distinguish it from other types of lung cancers. These include:
- Small cell lung cancers (SCLC)
- Non-small cell lung cancers (NSCLC) like adenocarcinoma
- Large cell carcinoma
Surgical Treatment of Squamous Cell Lung Cancer
Surgery is often the first choice for treating early-stage lung cancer in patients who are strong and healthy enough for it. Stage IIIA lung cancer used to be the most advanced stage that could be surgically removed.
The most common kind of surgery is an anatomic pulmonary resection, which usually involves removing a lobe of the lung. This is known as a lobectomy. There’s a less invasive way to do this called Video Assisted Thoracic Surgery (VATS), which can reduce the amount of time patients need to spend in the hospital as well as recover afterward.
Sometimes, instead of a lobectomy, doctors will do more limited resections. This might involve a segmentectomy (removing a segment of a lobe of the lung) or a wedge resection (removing a small, wedge-shaped portion of a lobe). While these surgeries may result in better lung function after surgery, they might carry a higher risk of the cancer coming back or death, especially for people who have non-small cell lung cancer that’s Stage T1N0. However, in some cases, these limited resections are necessary, such as when the patient’s lungs aren’t strong enough for a lobectomy, when lung nodules are small (2 cm or less), among others.
In some cases, if the cancer is located near the middle of the chest, has affected the main stem of the lungs, or has crossed major dividing lines within the lung, a pneumonectomy (removing the entire lung) might be needed. But this procedure can come with a higher risk of death and significantly impact lung function, so it’s usually only done when less major surgeries are not possible.
Before considering surgery for lung cancer, doctors need to carefully assess the condition of the patient’s heart, lungs, and overall health. They also need to predict what the patient’s lung capacity will be after surgery, as not doing so could lead to severe disability or even death. One way to do this is by using the CT scan of the chest that the patient would have already had.
It’s also critically important to conduct quantitative pulmonary function testing (measuring how well your lungs work) with spirometry (a test to measure the amount of air inhaled and exhaled) and to measure the lungs’ diffusion capacity (how well the lungs exchange oxygen and carbon dioxide with the blood). Predicting the functioning of the lungs after the operation is defined by these pre-surgery values, how much lung remains after surgery, and how much these parts of the lung function.
When it comes to the actual surgery, there are certain risks. Lobectomies carry a death rate of around 1.4 to 2.6 percent. Common complications include air leaks (15-25 percent), atrial fibrillation (irregular heartbeat, up to 40 percent), and pneumonia (2.5 to 6 percent). Other complications may occur less frequently. If the entire lung is removed (pneumonectomy), the risks are higher with mortality rates ranging from 5 percent to 11 percent and complication rates as high as 60 percent. These complications include bronchopulmonary fistula (an abnormal passage between the lung’s bronchi and the body’s pleural cavity), cardiac arrhythmias (heart rhythm disturbances, 19 percent), pneumonia (3.5 percent), and empyema (a collection of pus in the space between the lung and the inner surface of the chest wall, 4.8 percent).
What to expect with Squamous Cell Lung Cancer
Squamous Cell Carcinoma (SCC), a type of lung cancer, can spread to various parts of the body like the brain, spine, bones, adrenal glands, and liver. Because there are fewer key biological targets for treatment in SCC and it is often detected at late stages, the outlook for these patients is generally not promising. However, it’s important to know that in advanced stages, where there are high levels of PD-L1 (a kind of protein that prevents the immune system from attacking cancer cells), certain treatments known as ‘checkpoint inhibitors’ have shown better and longer-lasting results compared to other types of lung cancer.
Possible Complications When Diagnosed with Squamous Cell Lung Cancer
Complications from squamous cell carcinoma (SCC) of the lung may include:
- Difficulty breathing if the tumor blocks the main air passages or causes fluid to gather around the lungs (a condition known as pleural effusion)
- Bleeding in the airway, which can cause coughing up blood
- Spread of the cancer to other parts of the body, leading to pain and problems with the nervous system
Recovery from Squamous Cell Lung Cancer
It has been proven that exercising before an operation and taking part in rehabilitation programs can greatly improve the success of the operation and lessen lung complications post-surgery. However, rehabilitation focused on the lungs after surgery, without having done any exercise before surgery, seems to show only slight to fair improvement in physical activity directly following the operation. At this point, we don’t yet know the long-term effects of this on general physical ability.
Preventing Squamous Cell Lung Cancer
Teaching people how to avoid or limit certain risk factors like tobacco use and job-related diseases can help reduce the likelihood of developing squamous cell carcinoma (a type of skin cancer). This includes using equipment that protects your health while at work. It’s also vital to educate people about the importance of early cancer screening through a low-dose CT scan of the chest. This test can help identify the disease in its early stages, making it easier to treat and manage.
Patients should also be given detailed explanations about the different stages of cancer and their chances of fully recovering if the disease is identified early. Additionally, discussions about palliative care, which aims to relieve pain and other symptoms in advanced cancer stages, are important. These instructions can alleviate stress for both patients and their loved ones.