What is Thymoma?
Thymomas and thymic carcinomas are types of cancer that start in the thymus, an organ that’s in the middle of your chest. The thymus is a two-part organ that’s important for the immune system and usually shrinks after puberty. These cancers have a strong connection with an autoimmune disease called myasthenia gravis, discovered by Alfred Blalock in 1939.
The thymus gets blood supply from branches off certain arteries and is drained by veins that go into a large vein known as the superior vena cava. Thymomas can vary greatly from one case to another. This means it’s hard to tell just from someone’s medical history whether their thymoma is benign (not cancerous) or malignant (cancerous). But, malignant thymomas tend to be more aggressive than benign ones.
When it comes to survival rates, about 12.5% of patients with invasive thymomas are alive 15 years after diagnosis. For patients with non-invasive thymomas, that figure is around 47%. Most deaths related to thymomas are due to cardiac tamponade (a serious medical condition in which blood or other fluid fills up the space around the heart) or other heart and lung complications.
What Causes Thymoma?
There aren’t any recognized risk factors that may increase one’s chances of developing thymomas or thymic carcinoma, which are types of tumors that evolve in the thymus gland. The reasons why these types of tumors occur are still not clear.
However, there is a significant link between thymomas and a condition called myasthenia gravis, which is a disorder causing muscle weakness. Thymomas are also associated with other ‘paraneoplastic syndromes’. These are a group of health conditions appearing in people suffering from cancer, but they are not caused by the cancer itself. These conditions include total red cell aplasia (a severe drop in red blood cell production), polymyositis (an inflammatory muscle disease), systemic lupus erythematosus (an autoimmune disease), Cushing syndrome (disorder caused by high levels of the hormone cortisol), and the syndrome of inappropriate antidiuretic hormone secretion (a condition where excessive levels of antidiuretic hormones are produced causing water retention and low sodium levels in the blood).
It’s been found that between 30 to 40 percent of people with a thymoma also show symptoms of myasthenia gravis. Additionally, 5% of the patients have paraneoplastic syndromes.
Risk Factors and Frequency for Thymoma
Thymomas and thymic carcinomas are the most frequently occurring tumors in the space in the chest between the lungs, known as the anterior mediastinum. These types of tumors make up about 20% of all tumors found in this area. These tumors commonly appear between the ages of 40 and 60. It’s important to note that these conditions do not show a preference for any specific gender or race.
Signs and Symptoms of Thymoma
Thymomas and thymic carcinomas are types of tumors that can occur in the thymus, a small organ in the chest. People with these conditions generally experience symptoms in one of three ways:
- They are not experiencing symptoms, but the tumor is discovered during an unrelated imaging test.
- They experience symptoms like shortness of breath or a cough due to the tumor pressing on organs within the chest.
- They experience symptoms due to a condition related to the tumor, known as a paraneoplastic syndrome.
The specific symptoms of thymoma can vary. Some people have chest pain, cough, or issues related to the tumor affecting nearby organs. Thymoma can also cause symptoms related to a condition called myasthenia gravis. This is an autoimmune disorder where the body’s immune system attacks certain receptors in the muscles, leading to symptoms like double vision, drooping eyelids, trouble swallowing, weakness, or fatigue. About half of people with thymoma also have myasthenia gravis. Other associated conditions include pure red cell aplasia, a condition affecting the production of red blood cells, and various types of immune deficiency. Less than 5% of people with thymoma have syndromes like hypogammaglobulinemia or pure white cell aplasia. These syndromes can cause symptoms like frequent infections, diarrhea, and swollen lymph nodes.
Thymic carcinoma, on the other hand, tends to be more aggressive and can invade other structures in the chest. Symptoms can include cough, chest pain, and conditions like phrenic nerve palsy or superior vena cava syndrome. Less than 7% of patients with thymic carcinoma have the disease spread to other parts of the body like the kidneys, lymph nodes, liver, brain, adrenal glands, thyroid, and bones.
Testing for Thymoma
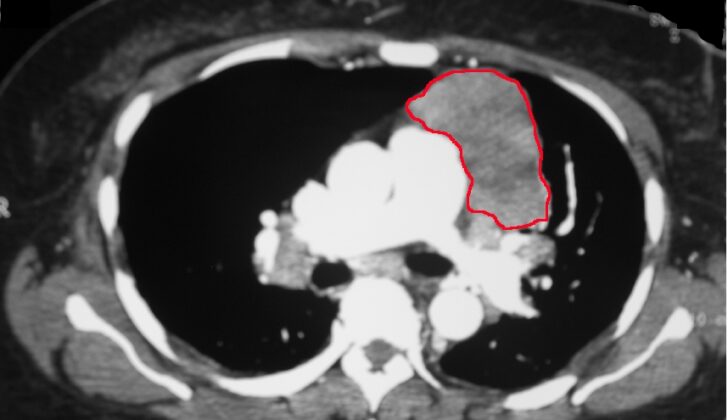
The process to diagnose a thymoma or a thymic carcinoma, which are types of tumors in the thymus gland in the chest, typically begins with an imaging test like a CT scan or an MRI of the chest. These tests can help in assessing whether the tumor can be surgically removed. Thymic carcinomas often reveal certain features like areas of dead tissue, cystic changes, or hardening due to calcium buildup. On the other hand, thymomas usually appear smooth with well-defined edges.
A CT scan of the chest can provide more information about the tumor and how it relates to other structures in the central part of the chest, known as the mediastinum. An MRI can help distinguish between solid and cystic masses. PET scans are also useful in distinguishing between benign (non-cancerous) thymomas and thymic carcinomas. Well-differentiated thymomas are usually PET-negative (not highlighted on the PET scan), while thymic carcinomas are often PET-positive (highlighted on the PET scan).
Blood tests are important too. These include markers for germ cell tumors (beta-hCG and AFP) and lymphoma (LDH and CBC) as both germ cell tumors and lymphomas are considered possible causes of a mass in the front part of the mediastinum. Lung function tests and a cardiac stress test should also be recommended for anyone being considered for surgery to remove the tumor. This will help decide if their heart and lung health can withstand a major surgical procedure involving removal of the thymus.
To definitively identify a thymic tumor, a sample of the tumor tissue is needed. This can be through surgical removal if the tumor is small and encased or larger tumors that can be safely removed. Otherwise, a biopsy (taking tissue samples) is done either percutaneously (through the skin) or through an open procedure when the tumor isn’t amenable to surgery, if the tumor needs treatment before surgery (called neoadjuvant therapy), or if surgery is not suitable due to age or existing health conditions. The percutaneous biopsy procedure makes use of CT-guidance and can involve a fine needle aspiration or a core needle biopsy. An open biopsy can be performed in various ways like thoracoscopy (inserting a small camera into the chest), mediastinoscopy (a procedure to examine the mediastinum), anterior mediastinotomy, or at times via endobronchial ultrasound. Accurate identification of the tumor type and the extent of the disease is pivotal in choosing the most suitable treatment approach.
Treatment Options for Thymoma
Thymic tumors are treated through several methods including radiation therapy with chemotherapy, steroids, immunotherapy, tyrosine kinase inhibitors (medications that block signals needed for tumors to grow), and surgery. It’s crucial to have a team of different healthcare professionals discuss and decide on the treatment plan for these tumors.
Till now, no definitive guide exists to manage these tumors, based on randomized controlled trials – scientific studies where people are randomly put into one of two or more treatment groups.
If you have a type of cancer that can be removed, such as a contained tumor or one that extends into areas that can be removed (like the pericardium which is the sac around the heart, the pleura which is the lining of the lungs, or a part of the lung), surgery is the recommended step because a complete tumor removal is possible. Usual treatment includes removing the entire thymus gland and surrounding lymph nodes. Long-term survival largely depends on complete tumor removal.
Sometimes, it might appear as though the tumor has spread, but it may actually be due to an inflammation-related fibrous reaction that resembles tumor invasion. This should be marked by the surgeon for further examination by the pathologist. If patients with myasthenia gravis (a long-term condition causing muscle weakness) require surgery, they should be carefully assessed beforehand, and their condition needs to be well-managed before surgery. Anesthesiologists, who are responsible for patient comfort and vital functions during surgery, should plan cautiously on putting the patient to sleep, intubation (tube placement for breathing), and awakening from anesthetic drugs.
Some patients may have tumors that can potentially be removed, but these may be invading critical areas such as the innominate vein (large blood vessel near the heart), phrenic nerves (nerves essential for breathing), or the heart and major blood vessels. These patients need a combination of therapies – pre-surgery chemotherapy and post-surgery radiation therapy. After chemotherapy, their condition is reassessed to see if surgery can be done. If it can, surgery is advised. Surgical approaches can involve removing part of, or an entire lung, followed by radiation therapy. Unfortunately, if their condition is deemed not suitable for surgery, the patient could go through a process of tumor debulking (removing as much of the tumor as possible) and radiation therapy. In cases of thymic carcinoma and ongoing disease post-surgery, patients should receive chemotherapy combined with radiation therapy.
Patients with tumors that can’t be removed, due to extensive spread to the pleura and pericardium (lining around the lung and heart), great vessel (major blood vessels of the body), heart, windpipe, or distant organ metastases (spread of cancer from the original site to other parts of the body), should receive systemic therapies such as radiation therapy alone or combined with chemotherapy. Patients not fit for surgery, considering their age or multiple health issues, might also be eligible for these treatments. The chosen therapy should be based on the extent of their disease, symptoms, and general performance status. Chemotherapy combined with radiation therapy has been seen to improve long-term survival and symptoms in some patients. Radiation therapy alone can relieve thoracic (chest related) symptoms like difficulty in breathing and coughing with a total dose of 60 or more Gy (unit of radiation dose). Chemotherapy is used as the primary symptom-easing therapy for widespread disease.
Lastly, in situations where the disease returns, surgical removal is recommended for localized recurrence (spread of cancer to nearby areas) and has shown to extend survival. In cases of more extensive recurrence, chemotherapy or symptom-easing radiation therapy is recommended.
What else can Thymoma be?
When trying to diagnose thymomas and thymic carcinomas, doctors will consider a range of possible conditions. These include:
- Thymic carcinoid tumors, which often occur in patients with a specific condition known as multiple endocrine neoplasia syndrome type 1
- Thymic cysts, which can be separated from solid tumors using a chest MRI scan
- Non-Hodgkins lymphomas, a type of blood cancer
- Germ cell tumors, especially in young males who have had previous testicular masses
- Ectopic parathyroid glands, which can be spotted using a scan known as a sestamibi scan
- Thyroid goiters, an enlargement of the thyroid gland
- Paragangliomas, although these are very rare
To identify the right condition, doctors need to order the right laboratory tests. These might include tests for germ cell markers and lymphoma markers. Doctors can also use imaging techniques to distinguish between different types of masses. For example, an MRI can show whether a mass is solid or a cyst, a sestamibi scan can find ectopic parathyroid tissue, and a thyroid scan can identify a thyroid goiter in the chest area.
Surgical Treatment of Thymoma
Before performing surgery to remove a tumor, doctors need to establish its stage and confirm that it is possible to remove the tumor. Methods used to confirm this can include taking a small sample of the tissue (biopsy), or diagnostic thoracoscopy, a procedure that uses a small camera to view the chest. It’s important to check how well a patient’s lungs and heart are working before surgery, using things like Pulmonary Function Tests (PFTs) and heart screenings. This is to ensure that the patient’s body will be able to handle the stress of surgery.
Patients with a condition called myasthenia gravis require special precautions before surgery. Myasthenia gravis is a chronic illness that weakens muscles. It’s crucial to avoid performing surgery on anyone experiencing a severe worsening of their myasthenia gravis symptoms, a state known as a myasthenic crisis. These patients should undergo a procedure called plasmapheresis before surgery and their steroid medication should be reduced. They may also need additional medication before their thymus gland removal surgery, or thymectomy.
There are three ways a doctor could perform this surgery: through a large vertical cut in the middle of the chest (median sternotomy), a horizontal cut in the neck (transverse neck incision), or minimally invasive surgery using robots (thoracoscopic surgery). When removing the thymus gland, the surgeon should avoid important nearby structures like the nerves that control the diaphragm (phrenic nerves) and the thyrothymic ligament, the tissue connecting the thymus to the thyroid gland. Sometimes, the surgeon may need to remove a portion of the layer that covers the chest cavity (mediastinal pleura), the sac around the heart (pericardium), part of the adjacent lung, a large vein in the chest (innominate vein), or one of the phrenic nerves. The best outcome is to remove all tumor (R0 resection), as this leads to the best long-term outlook. Leaving small amounts of tumor behind (R1 and R2 resections) has been linked to the tumor coming back.
Removing the lymph nodes around the thymus is also a crucial part of the surgery. Some lymph nodes are on the surface of the thymus and others are deeper. It’s generally recommended to remove both types of lymph nodes in cases of thymic cancer and thymomas, a type of tumor in the thymus, that have spread to nearby structures. In cases where the thymoma hasn’t spread, only the surface or N1 level nodes should be removed.
There can be complications after thymectomy surgery. The most common include respiratory failure which would require a breathing tube to be put in for a long period of time. This is especially common in patients with myasthenia gravis. In addition, pneumonia, fluid build-up in the chest (pleural effusion), a partially collapsed lung (atelectasis), a punctured lung (pneumothorax), and injury to the lungs can also occur. Injury to the nerves that control the diaphragm (phrenic nerves) and those that control our vocal cords (recurrent laryngeal nerves) can also occur. Infections at the surgical site or in the chest cavity (mediastinitis) can also happen. Measures can be taken to reduce these complications such as careful dissection, less traction, reduced steroid use, and more.
What to expect with Thymoma
Thymomas are tumors that grow slowly. The seriousness of this type of tumor mainly depends on how invasive it is. Contrarily, thymic carcinomas, another type of tumor, tend to be more aggressive and generally have a worse prognosis than thymomas. How advanced the disease is and whether the tumor can be completely removed also play a role in the prognosis.
A German study looked into the prognosis for different stages of thymic tumors:
* Thymomas in Masaoka stages I and II typically have an excellent prognosis.
* The prognosis is less favorable for Masaoka stage III thymomas after they have been surgically removed.
* For those with Masaoka stage III thymomas, there was a 27% chance of the tumor returning and 83% of patients survived at least 10 years.
* For Masaoka stage IV thymomas, the 10-year survival rate falls to 47%.
* There were no tumor-related deaths seen in the very early stages of the disease (Masaoka stages I and II, also known as types A, AB, or B1 disease).
* For later stages (B2, B3, or thymic carcinoma and Masaoka stages III and IV thymomas), the rate of death due to the tumor ranged from 9 to 60%.
After treatment,annual check-ups involving imaging tests are suggested even though these tests haven’t been proven to provide a clear benefit. It is generally recommended that a CT scan of the chest is performed every six months for two years, then once a year for the next five years for patients with thymic carcinoma, or for ten years for those with thymomas.
These thymic tumors often reappear in the form of nodules in the pleural tissue which is the thin layer of tissue that covers the lungs. This typically happens, on average, 8 to 68 months after treatment.
Thymic tumors are also associated with a risk of developing another type of cancer (around 17% to 28% risk after thymectomy, a surgery to remove the thymus). Data from the SEER database indicates an increased risk for specific types of cancers like B cell non-Hodgkin lymphoma (a kind of blood cancer), cancers of the gastrointestinal tract, and soft tissue sarcomas (cancer that begins in the soft tissues like muscles, tendons, fats, lymph vessels, blood vessels, and nerves).
Possible Complications When Diagnosed with Thymoma
Possible side effects of radiation include inflammation of the sac around the heart (radiation pericarditis), inflammation of the lung tissue (radiation pneumonitis), and scarring in the lung (pulmonary fibrosis). These usually occur after postoperative radiotherapy and could potentially be fatal. So, doctors need to thoroughly evaluate the potential gains versus risks before suggesting additional radiation treatment.
Common Side Effects:
- Inflammation of the sac around the heart (Radiation Pericarditis)
- Inflammation of lung tissue (Radiation Pneumonitis)
- Scarring in the lung (Pulmonary fibrosis)
- Possible death
Recovery from Thymoma
Advised treatment for those who have advanced thymomas, specifically stages III or IV, include a supplemental therapy called radiotherapy. This treatment is suggested even if the thymoma has been fully removed through surgery.
Preventing Thymoma
Individuals who have been diagnosed with myasthenia gravis, a condition that causes muscle weakness, should undergo a specific type of body scan known as a CT scan. The purpose of this test is to check a part of their chest, known as the thymus, for any abnormalities such as thymomas or thymic hyperplasia. A thymoma is a type of tumor that originates from the thymus. Thymic hyperplasia, on the other hand, is a condition where the thymus is larger than normal.
If any of these conditions are found, the patient may need to have a procedure called a thymectomy, which is the removal of the thymus. This procedure has been proven to help reduce the muscle weakness symptoms that people with myasthenia gravis often experience.