What is Tracheal Cancer?
Primary tracheal tumors are rare but generally cancerous in adults, constituting approximately 0.2% of all malignant tumors. The incidence of these cancers is estimated to be around 0.1 for every 100,000 people annually. A considerable study involving 578 cases indicated that 55% of those affected were men and that squamous cell carcinoma was the most common type, making up 45% of these cases. Other types of cancers included a range of carcinomas and sarcomas. Primary tracheal tumors are usually malignant in adults (up to 90% of the time), though in children, they are only cancerous in about 10 to 30% of the cases.
However, the symptoms of these tumors are very generic, often leading to delays in diagnosis. These symptoms include shortness of breath and wheezing, which could be confused with more benign conditions like asthma, chronic obstructive pulmonary diseases, and other similar diseases. It’s important to note that not all tumors found in the trachea are primary tracheal cancers. For example, a cancer that has spread to lymph nodes near the trachea and invaded it may be misidentified as a tracheal primary cancer. A comprehensive screening using imaging and tissue sample analysis can help identify cancers that have spread, which are actually more common than primary tracheal cancers. Therefore, it’s possible that primary tracheal tumors may be even rarer than currently estimated in the general population.
What Causes Tracheal Cancer?
Since cancers of the windpipe, or trachea, are very rare, doctors are still not sure what causes most types. However, for one specific type of tracheal cancer – squamous cell carcinoma – they have identified smoking and being exposed to certain airborne cancer-causing substances, like hydrocarbons, as possible risk factors. This type of tracheal cancer is often found in people who have previously had lung cancer; in fact, about 25% of patients with squamous cell tracheal cancer have a history of lung cancer. This demonstrates why examining the airways with a bronchoscope – a thin tube with a light and camera at the end that doctors use to view the trachea and lungs – is so important for patients who had lung cancer but were successfully treated.
Risk Factors and Frequency for Tracheal Cancer
Tracheal cancers are quite rare, with only 0.1 new cases per 100,000 people each year. They make up between 0.1% and 0.4% of all new cancer diagnoses annually. There are a few different types of tracheal cancer, with squamous cell carcinoma and adenoid cystic carcinoma being the most common.
- Squamous cell carcinoma is more common in men and typically affects people between 60 and 70 years old.
- Adenoid cystic carcinoma happens to men and women equally, most frequently in people in their 40s and 50s.
- These two types account for about 66% of all primary tracheal cancers.
- The remaining 34% of cases are made up of various benign and malignant tumors.
Signs and Symptoms of Tracheal Cancer
Tracheal cancer often shows symptoms similar to those of other respiratory conditions, such as dyspnea (shortness of breath), stridor (a high-pitched wheezing sound), coughing, and hemoptysis (coughing up blood). These symptoms are a result of the irritation and obstruction in the airway. Patients may also have difficulty swallowing, or hoarseness due to the cancer pressing on nearby parts of the body.
Different types of tracheal cancer can exhibit different symptoms. For instance, squamous cell carcinoma usually involves coughing up blood and is typically detected within four to six months of showing symptoms. On the other hand, adenoid cystic carcinoma grows slowly and often causes symptoms such as shortness of breath and wheezing. Diagnosing this type of cancer can take a longer period of time.
Several factors contribute to the delay in diagnosis. One is that symptoms like cough, shortness of breath, and wheezing are common in many respiratory diseases such as chronic obstructive pulmonary disease (COPD), asthma, and bronchitis, leading doctors to initially suspect these conditions. Another factor is that the trachea has a large diameter, so symptoms of obstruction generally don’t appear until the tumor blocks 50 to 75% of it.
Interestingly, the obstructed tracheal diameter size also impacts the type of dyspnea one will experience. An obstruction smaller than 0.8 cm generally causes shortness of breath during physical exertion, while an obstruction smaller than 0.65 mm can cause shortness of breath even at rest. The third contributing factor for delayed diagnosis is that adenoid cystic cancers and other benign tumors develop slowly over months or even years, causing symptoms to progress at a gradual pace.
Doctors should be suspicious that a case might be tracheal cancer when respiratory symptoms fail to improve with initial medical treatment. Squamous cell carcinoma of the trachea is seen more often in males, between ages 60 and 70, and among smokers. On the contrary, adenoid cystic carcinomas of the trachea can occur in both genders, typically between ages 40 and 50, and aren’t associated with smoking.
Testing for Tracheal Cancer
When you first visit the doctor, they’ll start with a chest x-ray. This helps to rule out other potential issues before focusing on the possibility of a tracheal tumor. However, these tumors are rare and often difficult to see on an x-ray, so they need to look out for them specifically.
To get a clearer picture, the doctor may use a computed tomography (CT) scan. This technique has become much more advanced in recent years, and now allows for a three-dimensional view which can help detect cancer at an early stage. The scan can show things like growths, narrow areas, or thickening of the walls of the trachea. CT scans or a type of scan called positron emission tomography (PET) are also helpful for seeing how far the disease has spread, which can help determine the best treatment.
However, some types of tumors, like adenoid cystic carcinoma and slowly growing mucoepidermoid tumors, may look a bit different on PET scans.
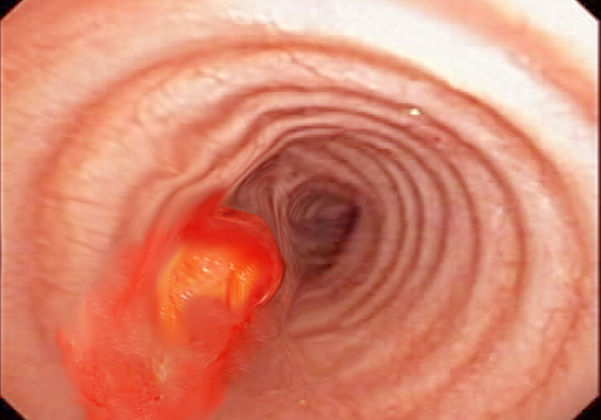
To actually see the tumor and take a tissue sample for testing, the doctor may use a procedure called bronchoscopy. This helps them to tell if the growth is malignant (cancerous) or benign (non-cancerous). Endobronchial ultrasound can help in getting a better understanding of how far the tumor extends into the wall of the trachea and whether it can be removed surgically.
Tests called spirometry can also give information about how much the tumor is affecting your breathing. Lastly, if you have changes in your voice, such as hoarseness or a weak voice, the doctor may use a laryngoscope, a medical device that allows the doctor to see your vocal cords and larynx.
Treatment Options for Tracheal Cancer
Surgery is the ideal treatment for malignant tracheal tumors, a rare and serious form of cancer that occurs in the trachea, or windpipe. However, the possibility of performing surgery safely depends on various patient-specific factors, like age, weight, and overall health condition, as well as the size and location of the tumor itself. Typically, up to half of the trachea can be removed, if necessary. The aim is not just removing the tumor, but also reconstructing the trachea to maintain normal breathing function.
Before the surgery, a series of imaging and assessment techniques, such as CT scans and ultrasound-endoscopy, are used to evaluate the tumor. The surgery involves carefully separating the trachea from nearby vital structures, removing the tumor, and then reconstructing the trachea. It’s important not to disturb the trachea’s blood supply, as this could create problems with healing after surgery. Particular ways of performing the surgery, known as release maneuvers, can be used to ease the tension in the reconstructed trachea.
Surgery can extend a patient’s life – research shows that the 5-year survival rate is 50% for those treated with surgery, compared to just 10% in those who can’t have surgery. However, because these tumors are so rare, it’s recommended that patients go to specialist centers that have extensive experience in managing them.
In those cases where the tumor is advanced and can’t be completely removed, or the surgical margins are not completely free of disease, radiation therapy may be used along with the surgery. This helps to kill any remaining cancer cells and improve patient outcomes. Radiation therapy is also a first-line treatment for patients who are not suitable for surgery.
If the tumor is causing an obstruction in the windpipe, a stent may be necessary to keep the airway open. The stent placement is usually combined with radiation therapy to counter the growing tumor.
In patients with metastatic squamous cell carcinoma, where the cancer has spread to other parts of the body, systemic therapy like immunotherapies are often used. This is similar to the treatment for lung or head and neck squamous cell carcinomas.
Because tracheal tumors can recur after surgery, regular surveillance is recommended. Endoscopic examinations allow doctors to monitor the trachea and detect any recurring or new cancers early.
What else can Tracheal Cancer be?
Here’s a simplified list of some kinds of benign or non-cancerous tumors:
- Paraganglioma
- Pyogenic ganglioma
- Benign vascular tumors
- Squamous papilloma
- Pleomorphic adenoma
- Peripheral nerve sheath tumor
- Schwannoma
- Atypical schwannoma
- Plexiform neurofibroma
- Hemangiomatous malformations
- Leiomyoma
- Plasma cell granuloma
And here’s a list of some types of malignant or cancerous tumors:
- Small cell carcinoma
- Large cell carcinoma
- Adenocarcinoma
- Adenosquamous carcinoma
- Carcinoids
- Melanoma
- Lymphoma
- Chondrosarcoma
- Spindle cell sarcoma
- Leiomyosarcoma
- Invasive fibrous tumor
- Malignant fibrous histiocytoma
- Psudosarcoma
- Mucoepidermoid carcinoma
What to expect with Tracheal Cancer
The chance of surviving primary tracheal cancer for five years depends on the type of tumor. Specifically, adenoid cystic carcinomas have a more promising outlook than squamous cell carcinomas. This is shown in the significant difference in the five-year survival rate for each (74% vs. 13%).
The better outlook of adenoid cystic carcinomas is due to the slower growth of these tumors and the fact that they take longer to progress naturally. Diagnosing and treating these tumors surgically before they spread locally or to distant parts of the body improves the outlook and increases survival chances.
Data from a large, population-based registry shows that the five-year survival rate was 4% for cancers that spread far from the original tumor (distant metastasis), 25% for cancers that spread to nearby areas (regional disease), and 47% for cancers that haven’t spread far (localized).
Possible Complications When Diagnosed with Tracheal Cancer
The complications arising from the primary growth and spread of cancer to nearby organs can bring about problems such as blockage of the airway, difficulty swallowing, and changes in voice. After surgery, there could be complications such as failure in surgical stitching to heal, infections, the return of cancer, and lowered quality of life. This is especially apparent when large parts of the windpipe have to be removed, which can significantly limit neck movement.
- Blockage of the airway
- Difficulty swallowing (dysphagia)
- Voice changes (hoarseness)
- Failure in surgical stitching to heal
- Infections after surgery
- Recurring cancer
- Lowered quality of life post-surgery
- Limited neck movement due to removal of large parts of the windpipe
Preventing Tracheal Cancer
After the treatment, it’s normal for patients to have regular check-ups. It’s important that if patients start to experience any new symptoms in between these check-ups, they tell their doctor right away. Facing an illness can also bring a range of emotions like anger, resentment, guilt, anxiety, and fear. It can be helpful to have psychological support during this time, so resources should be available to help manage these feelings.