What is Tracheoesophageal Fistula?
Tracheoesophageal fistula (TEF) is a birth defect that’s often seen in major children’s surgery centers. It’s one of the most common ones of its type. Babies with this defect often struggle to breathe, have trouble eating, might choke, and are at risk of inhaling food or liquid into the lungs, a problem known as aspiration. Tracheoesophageal fistula is often found with other birth defects, especially those that affect the heart.
There’s another related birth defect known as esophageal atresia, which presents similarly to TEF. This can occur with or without a TEF. Essentially, esophageal atresia is a condition where the esophagus or food pipe is not properly formed and can cause similar feeding and breathing issues as TEF.
What Causes Tracheoesophageal Fistula?
The separation of the two tubes in our body, the trachea and esophagus, that form early in a baby’s development is not completely understood. But scientists believe a common cause of problems like tracheoesophageal fistula (TEF) and esophageal atresia, where the trachea (windpipe) and esophagus (food pipe) don’t form properly, could be due to an issue with the splitting of this shared early tube – the foregut – into the separate trachea and esophagus.
Around the fourth week of a baby’s development, the common tube begins to separate, with the front part becoming the respiratory tract (air passageways), and the back part becoming the esophagus (food pathway). The fistula tract, a kind of unwanted passageway that joins the trachea and esophagus, might develop from a small lung bud that fails to branch off properly. Abnormal growth in this early stage is believed to cause TEF.
The VACTERL complex refers to a group of birth defects that can also affect the same area. The term ‘VACTERL’ is an acronym for Vertebrae (spinal defects), Anal or gastrointestinal tract Atresia (blockage or abnormalities of the gut), Congenital Cardiac (heart) defects, Tracheoesophageal defects, Renal (kidney) and urinary tract anomalies, and Limb lesions (arm or leg abnormalities).
Researchers have linked issues with a gene known as Sonic Hedgehog (SHH) to esophageal atresia. Studies on mice show that disturbances in the regulation of the SHH gene can result in VACTERL-like abnormalities.
Studies on rats have also implicated the usage of Adriamycin, an antibiotic that impacts DNA integrity and creation, in causing TEF. Injecting this into pregnant rats resulted in 40% to 90% of the babies having esophageal atresia and TEF. This replicates what can happen in newborn human babies. In addition, these studies showed that such rats can also exhibit VACTERL anomalies.
Lastly, researchers have also found that Gli-2, a signaling molecule associated with the SHH gene, was decreased in the fistula tract compared to the surrounding esophagus.
Risk Factors and Frequency for Tracheoesophageal Fistula
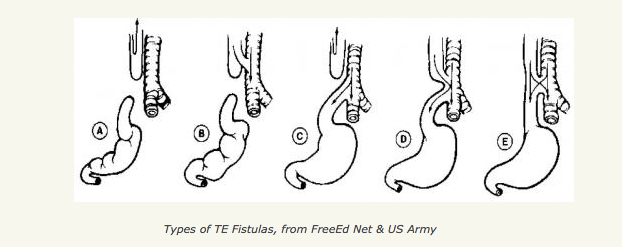
Tracheoesophageal fistula (TEF), a condition affecting the digestive and respiratory systems, does not appear to be strongly linked to genetics. It occurs in about 1 in every 3500 births. TEFs are categorized based on their physical structure, with Type C being the most common and making up 84% of cases. TEFs without esophageal atresia (a condition where the esophagus doesn’t develop properly) are less common, accounting for only 4% of cases.
The rate of TEF appears to be decreasing in Europe. It does not seem to be linked to the mother’s age unless chromosomal disorders are involved. It is often found in conjunction with other health problems. Some statistics suggest that between 38.7% and 57.3% of TEF cases are isolated, while the remainder are linked with other congenital abnormalities. Chromosomal abnormalities like trisomy (an extra chromosome) are present in 6% to 10% of TEF cases, but this excludes babies younger than 28 weeks of gestation. Also, the rare Feingold syndrome, characterized by small head and jaw size and finger abnormalities, can have an associated TEF or esophageal atresia.
In assessing the risk of TEF, doctors consider factors such as birth weight, pneumonia, and associated anomalies. Despite this, survival rate in babies with TEF and weight less than 1500 grams without major heart issues is around 97%. However, the survival rate drops to 22% if the baby is underweight and has significant cardiac problems. The risk of death is highest due to heart and chromosomal defects, and long-term respiratory issues also play a role.
Signs and Symptoms of Tracheoesophageal Fistula
In a study by Keckler and colleagues, it was found that Tracheoesophageal Fistula (TEF), a condition where there’s an abnormal connection between the trachea and esophagus, was most commonly linked with congenital heart disease in about 32.1% of the patients. However, they excluded infants with patent foramen ovale and patent ductus arteriosus. The most frequent form of heart abnormality accompanying TEF was a ventricular septal defect, found in 22.3% of patients. Surprisingly, only 7.1% of cases presented with a ventricular septal defect alone. Cyanotic heart disease, a condition causing low oxygen levels in the blood, was not common and was only found in 4.5% of patients, all of whom exhibited tetralogy of Fallot, a complex heart defect.
Another congenital defect often seen with TEF was vertebral anomalies, evident in 24% of patients. These vertebral defects usually accompany other abnormalities of the spinal column, like rib anomalies and a tethered cord. An increased risk of anastomotic leak, a complication after a surgical join, was associated with these spinal abnormalities, likely due to increased tension at the surgical site. This might be because the two ends of the esophagus could be further apart due to a higher proximal pouch in patients with these skeletal deformities.
The symptoms of TEF usually depend on whether there is esophageal atresia, a condition where the esophagus doesn’t develop properly. Two-thirds of pregnancies with this condition may experience polyhydramnios, which is an excess of amniotic fluid, although it frequently goes undetected before birth. Newborns with esophageal atresia may show symptoms just after birth, like excessive drooling, choking, breathing distress, and inability to feed. A common complication is the distension of the stomach due to the abnormal connection between the trachea and the lower part of the esophagus. This situation can lead to the backflow of stomach contents into the lungs, resulting in aspiration pneumonia and increasing illness.
Patients with H-type TEFs, where the abnormal connection is without esophagus deformation, may show symptoms early if the defect is large. These symptoms primarily include coughing and choking due to inhaled food or liquid. In some cases, however, minor H-type defects may not show symptoms in newborns, leading to a delayed diagnosis that could range from 26 days to 4 years. Patients may have a long history of mild respiratory problems associated with feeding or recurrent bouts of pneumonia. In rare cases, the diagnosis might even be delayed until adulthood.
Testing for Tracheoesophageal Fistula
Tracheoesophageal fistula (TEF), a rare condition that can affect a baby’s feeding and breathing, can sometimes be detected before birth. This is often determined by a large quantity of amniotic fluid (polyhydramnios) and the absence of a visible stomach on an ultrasound scan of the baby. However, the ability to diagnose this condition via prenatal scanning isn’t always accurate, with a success rate of about 42%.
Because TEF is often found in infants with a specific genetic disorder known as trisomy 18, doctors might order a karyotype test, which examines the baby’s chromosomes. Doctors also look for signs of heart defects on ultrasound images, as these can suggest a more severe prognosis for the baby.
If doctors think a baby may have TEF, the mother should plan to give birth in a medical center that has a neonatal intensive care unit and surgical facilities. TEF is often associated with other conditions such as VACTERL sequence, CHARGE syndrome, trisomy 18 and 21, and DiGeorge syndrome. Also, babies with esophageal atresia (a birth defect where part of the esophagus, the tube that carries food from the mouth to the stomach, doesn’t develop properly) often have other anomalies, affecting up to 65% of such cases. The risk of having another baby with non-syndromic esophageal atresia or TEF is about 1% in further pregnancies.
TFE diagnosis can also be made after the baby’s birth. The medical team may try to insert a tube from the baby’s mouth or nose down into the stomach. If the tube can’t go any further than 10 to 15 cm, this maybe becaue of esophageal atresia. This information can be confirmed with a chest X-ray which may show the inserted tube curling up in the upper part of the esophagus. The X-ray may also show a gas-filled gastrointestinal tract suggesting evidence of TEF.
Doctors may then use a procedure called fluoroscopy, which involves the use of a type of dye that can show any abnormal connections between the esophagus and the windpipe (trachea) on the X-ray. It’s important to note that certain contrast materials like barium should be avoided as they can cause lung inflammation if accidentally inhaled. After the procedure, any contrast material must be removed immediately to ensure it won’t be swallowed and breathed into the lungs.
Alternatively, doctors may also use upped gastrointestinal series, which involves using thickened contrast material that is easier to see and track on X-rays. Another method could be to inject a blue dye into the windpipe to visualize the possible abnormal connection between the esophagus and the windpipe. In some cases, three-dimensional CT scanning has also been found to be effective in diagnosing TEF.
Treatment Options for Tracheoesophageal Fistula
In 1941, an American surgeon, Cameron Haight, was the first to perform a successful repair of a tracheoesophageal fistula (TEF), which is an abnormal connection that forms between the windpipe (trachea) and the food pipe (esophagus). Nowadays, survival rates for patients with TEF have exceeded 90% in pediatric surgical centers. Therefore, the focus has shifted to reducing the side effects of treatment and improving quality of life for these patients.
The standard surgical treatment for TEF involves making a cut in the chest, closing off the abnormal connection, and reconnecting the esophagus properly. As part of the preparation for this surgery, patients may undergo an echocardiogram, a non-invasive test that checks the health of the heart, along with kidney ultrasound, spine ultrasound, and limb X-ray to rule out other associated conditions.
However, complications may include leakage from the reconnected esophagus, nerve injury leading to vocal cord paralysis, narrowing of the esophagus, a persistent abnormal upper pouch, reformation of the abnormal connection, and, in rare cases, death.
When the upper and lower parts of the esophagus are too far apart to be reconnected, other surgical techniques might be used. In 2001, two surgeons, Tom Lobe and Steve Rothenberg, performed the first minimally invasive thoracoscopic TEF repair. This method, which involves entering the body through a small incision, can cause fewer side-effects. It is preferred by some because it reduces the risk of scarring and chronic pain associated with open procedures.
Immediate care after surgery includes providing a special feeding tube and a steady suction of the upper pouch of the esophagus to prevent food or saliva from entering the lungs. If it is not possible to reconnect the esophagus, alternative reconstruction methods using organs like the stomach or large intestine can be used. These methods are not always ideal, as they can increase recurrent aspiration and chronic lung issues. However, if the esophagus is too short at birth, a staged procedure where the esophagus is progressively elongated as the baby grows can be employed.
There has also been some success with various endoscopic repair methods utilizing adhesives and lasers, which are less invasive and cause fewer side-effects, but these require more research.
Prior to surgery, infants will go through a thorough examination process, including laryngoscopy and bronchoscopy. These procedures enable doctors to examine the condition of the throat and lungs, respectively, providing key insights for planning the surgical repair.
Due to the high risk of gastroesophageal reflux disease (GERD, a chronic disease where stomach acid frequently flows back into the esophagus) after surgery, it is suggested that infants treated for TEF be routinely given a medicine that reduces stomach acid for at least a year after surgery. It is also noted that children born with TEF should be closely monitored for potential lung and digestive complications throughout childhood.
What else can Tracheoesophageal Fistula be?
When a doctor is trying to diagnose tracheoesophageal fistula (TEF) and esophageal atresia, there are other conditions that might look similar. These include:
- Esophageal stricture or diverticulum (narrowing or pouch in the esophagus)
- Pharyngeal pseudodiverticulum (a false pouch in the throat)
- Severe GERD (acid reflux disease)
- Vascular ring (a specific formation of blood vessels)
- Iatrogenic esophageal perforation (damage caused to the esophagus by a medical procedure)
- Laryngotracheoesophageal cleft (a rare birth defect that affects the throat and windpipe)
- Esophageal webs (thin tissue that can block the esophagus)
- Esophageal duplication (a rare birth defect where a second esophagus is present)
- Congenital shortened esophagus (a short esophagus present from birth)
- Tracheal agenesis or atresia (a rare birth defect where the windpipe does not develop normally)
By considering these possibilities, doctors can make sure they have the right diagnosis.
What to expect with Tracheoesophageal Fistula
The outlook for newborns with a condition called Tracheoesophageal Fistula (TEF) is generally positive. However, if an infant has both TEF and a condition called Esophageal Atresia, the outcome is more uncertain and depends on other associated problems. One study found that 87% of patients with either Esophageal Atresia or both conditions survived, although 61% of deaths were linked to heart and chromosomal abnormalities. The presence of heart disease significantly increased the risk of death.
In addition, those newborns who weighed very little at birth had lower chances of survival. The length of the gap in the esophagus, which is what Esophageal Atresia involves, can also influence the prognosis. Children with these conditions often struggle with growth; about one-third weighed below the fifth percentile at birth. However, as they age, their height and weight outcomes generally improve significantly.
Feeding abnormalities are a common issue during early childhood for these children. Some develop an aversion to eating orally due to complications such as GERD (a type of acid reflux disease), tightening of the area where the esophagus is joined (anastomotic strictures), and irregular movement of the esophagus (esophageal dysmotility). These children might need a procedure to guide a tube into the stomach (gastrostomy tube placement) for enhanced nutrition. This kind of feeding aversion is more common in children with only Esophageal Atresia, mostly because they are initially fed exclusively through a gastrostomy tube.
Respiratory complications are also frequent. Severe softening and weakening of the trachea or bronchi (tracheomalacia and bronchomalacia) occur in 10% to 20% of these infants. This can lead to a life-threatening blockage of the airway. Some babies may require a procedure to anchor the aorta (aortopexy) for stabilizing the trachea and reducing dependency on a ventilator. Further, these children may often experience recurring bronchitis and pneumonia, leading to irreversible lung damage if not treated. Wheezing, an issue for up to 40% of survivors, is persistent and does not improve with age. However, these respiratory issues generally lessen in late adolescence. Despite certain lung abnormalities detected in up to 40% of survivors, most children can lead an active daily life.
The management of these lung conditions includes the use of antibiotics, physical therapy and tailored treatment for GERD. Inhalers that deliver medications to relax the airways (bronchodilators) and reduce inflammation (steroids) are helpful for asthma symptoms. Regular lung function tests and chest CT scans are used to monitor the child’s progress.
Possible Complications When Diagnosed with Tracheoesophageal Fistula
The main problems that can arise after repairing esophageal atresia and a tracheoesophageal fistula (TEF), based on a study of 227 cases, are leaks in the surgical connection (16% of cases), narrowing of the esophagus (35%), and recurring tracheoesophageal fistulae (3%). The narrowing of the esophagus can often be successfully treated with a procedure that dilates the esophagus using a balloon. An additional 15% of cases involved a condition called tracheomalacia, with 40% of these cases necessitating further surgery. Normal food movements and delayed stomach emptying are normal issues and can contribute to GERD and aspiration. Almost half of all patients require further treatment to widen the surgical connection site due to early narrowing. Few need removal of the narrow segment of esophagus. GERD can increase the chance of esophageal narrowing, but a surgical procedure known as a fundoplication might help. Esophageal movement issues are to be expected and can be seen in 75%-100% of children after initial repair via a test called manometry. Common symptoms include difficulty swallowing, food blockages, failure to grow properly, and choking.
Chest surgery can lead to significant issues with the muscles and structure of the chest. Defects in the spine associated with the VACTERL sequence can contribute to chest or spine deformities. One report noted that 24% of patients had a winged scapula due to paralysis of the latissimus dorsi muscle (a large muscle in the back), while 20% of children showed asymmetry of the chest due to smaller-than-normal serratus anterior muscle (a muscle located at the side of the chest). If you are a female infant, the surgery may result in uneven breast development with disfigurement. Using modified axillary incisions or thoracoscopic techniques might reduce these issues.
Movement disorders and abnormal respiratory function are common after esophageal atresia and TEF repair and should be monitored. A review of long-term outcomes in adulthood after esophageal atresia repair in infancy reported the following estimated average occurrences:
- Difficulty swallowing: 50.3%
- GERD with esophagitis (a type of inflammation in the esophagus): 40.2%
- GERD without esophagitis: 56.5%
- Respiratory tract infections: 24.1%
- Asthma: 22.3%
- Wheezing: 34.7%
- Chronic cough: 14.6%
- Barrett’s esophagus (abnormal change in the cells of the lower esophagus): 6.4%
- Squamous cell esophageal cancer: 1.4%
The chance of developing Barrett’s esophagus in adulthood was four times greater than in the general population; implying an increased risk of esophageal cancer. The risk of this type of cancer is about 50 times that of the general population aged 40 and above.
Recovery from Tracheoesophageal Fistula
After surgery, tests known as laryngoscopy and bronchoscopy are done to gauge how severe the condition of a floppy windpipe, also known as tracheomalacia, is. These tests also help to find missed or reappearing abnormal connections, called fistulae.