What is Diabetic Macular Edema?
The retina is a thin layer of tissue located at the back of the eye near the optic nerve. It contains cells that sense light and turns this light into signals that the brain can understand to create vision. Proper functioning of the retina is crucial for our ability to see, and any damage to it can lead to serious vision problems. The middle part of the retina, called the macula, has the highest number of light-sensing cells. Diabetes can cause a condition called macular edema, which is one of the major reasons for vision loss in the United States. The most common treatment involves using a therapy that targets a growth factor in our bodies, but researchers are developing new methods of treatment.
What Causes Diabetic Macular Edema?
Diabetes can lead to high blood sugar levels that cause the formation of harmful substances known as advanced glycation end products (AGEs). The exact reasons behind diabetic eye disease, or diabetic retinopathy, aren’t entirely clear, as it’s likely caused by a combination of different factors.
AGEs can attract and hold onto water, which may explain why fluid tends to build up in the macula – the part of the eye that provides sharp, clear, central vision. On top of that, diabetes often weakens the blood-retinal barrier (BRB), a defense mechanism that prevents harmful substances from reaching the retina. This weakening could play a crucial role in the development of a condition called macular edema, which causes blurry vision in diabetics.
Furthermore, AGEs are linked to an increase in signs of inflammation such as a specific marker called VEGF, white blood cell sticking, and an enzyme known as protein kinase C. All these factors contribute to the complexity of diabetic eye disease.
Risk Factors and Frequency for Diabetic Macular Edema
Diabetic macular edema (DME) is one of the main reasons people lose their sight around the world. It impacts over 75,000 Americans every year, and nearly 100 million people globally show some symptoms of it due to diabetes. Research indicates that around 1 in 3 diabetic patients have some signs of macular edema. People with type 1 diabetes are more likely to develop DME than those with type 2.
- For those diagnosed with diabetes, there’s a 20% chance they will develop DME in 10 years if their diabetes diagnosis was before age 30.
- If the diagnosis was after age 30, the 10-year incidence of DME rises to about 40%.
- Around 27% of patients will show symptoms of macular edema within 9 years of being diagnosed with diabetes.
Several studies focusing on different demographic groups show an increasing occurrence of DME.
Signs and Symptoms of Diabetic Macular Edema
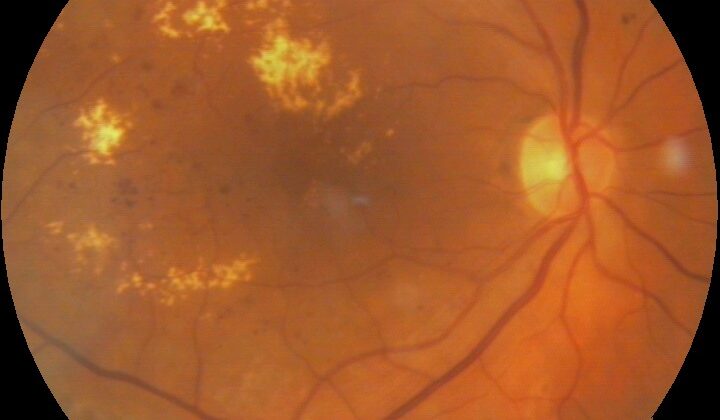
People with diabetes need to have eye check-ups more regularly than others, generally once a year. This is to detect conditions like Diabetic Macular Edema (DME), a condition where the macula (part of the eye) becomes thicker. DME can look different in different people, with the macula thickening in multiple small areas, a single area, or diffusing over a large area.
The condition is diagnosed by looking at the eye with a special instrument, comparing it to what a normal eye should look like. Professionals typically use The Early Treatment Retinopathy Study’s (ERDRS) definition, which states that DME is either a thickening of the retina or the presence of hard deposits within a certain distance from the center of the macula.
DME is considered serious enough to need medical attention if any of the following features are present:
- Thickening within 500 mm of the center of the macula
- Hard deposits within 500 mm of the center of the macula, if accompanied by thickening of nearby retinal tissue
- Zones of retinal thickening 1 disk area, part of which is within 1 disk diameter of the center of the macula
Even if only one of these features is present, DME is considered clinically significant and often, several features might be present at the same time.
Testing for Diabetic Macular Edema
Diabetic macular edema (DME) is mainly evaluated using a slit lamp and stereo fundus photography. However, there are many new methods being created and used now to better understand this condition.
One method is Fluorescein Angiography (FA), where a fluorescent dye is injected into the bloodstream. This dye helps to identify any fluid buildup in a qualitative manner. Another method, Optical Coherence Tomography (OCT), uses high-resolution imaging to examine the retina, and measure the thickness of it. OCT is less invasive than FA, so it is generally more comfortable for patients. OCT is also better than the slit lamp and stereo fundus photography at determining the thickness of the macula and pinpointing where retinal fluid is located.
Another imaging technique used is the Retinal Thickness Analyzer (RTA). RTA uses a laser beam to measure the thickness of the retina. While RTA and OCT show similar thickness results, OCT images are clearer and less affected by cloudiness in the eye’s natural lens. Despite taking longer to capture images, OCT and RTA are valuable for early DME detection. After the diagnosis, FA is helpful for further understanding of DME.
As per the early treatment diabetic retinopathy study criteria, it’s significant to note that clinically significant macular edema is present when the retina gets thicker within 500 µm of the macular center, hard exudates exist within 500 µm of the macular center with nearby retinal thickening, or retinal thickening spanning an area greater than one disc diameter, part of which is within one disc diameter of the macular center.
Treatment Options for Diabetic Macular Edema
Historically, laser photocoagulation, a type of laser treatment, has been a key method for treating diabetic macular edema, a condition that can affect the eyesight of people with diabetes. It has been found to improve vision in a subset of patients. Guidelines from the Early Treatment Diabetic Retinopathy Study outline how to use this laser treatment method. These include directly treating leaking blood vessels in the eye, and using a combination of precision and scattered laser treatments in specific cases.
However, while macular laser treatment remains a major method for addressing significant vision depletion caused by macular edema, it doesn’t cure the condition, and many times the condition doesn’t respond to the laser treatment. Removing the vitreous (a clear gel in the eye), also known as a vitrectomy, has been found to enhance the condition, but researchers are still not sure why this is the case.
New research has since led to changes in treatment guidelines. Now, the most recommended treatment involves anti-VEGF therapy. Other treatments include a lower threshold laser treatment and injections of steroids into the eye.
What else can Diabetic Macular Edema be?
Swelling in the macula (the central part of the eye’s retina), known as macular edema, can result from various conditions that include:
- High blood pressure
- Blockage in a vein of the retina
- Bursting of a tiny blood vessel cylinder (microaneurysm)
- Exposure to radiation
- Irvine-Gass syndrome, a rare condition following cataract surgery
- Growth of new blood vessels under the macula (subfoveal choroidal neovascularisation)
The reason behind the swelling is not always clear, so a detailed personal health history is an important tool for a doctor trying to identify the cause. They may ask questions about conditions like diabetes and how it is managed, dietary habits, and other health problems related to diabetes. These clues can be critical in diagnosing the source of the problem.
What to expect with Diabetic Macular Edema
The outlook for diabetic macular edema, a condition that affects vision, depends on a few key factors. The severity of the condition when it’s first detected is especially crucial. The worse the condition is at the start, the more likely it is that a person’s vision will worsen over time.
It’s also very important to manage treatments well, along with controlling diabetes and high blood pressure. These actions can help prevent diabetic macular edema from getting worse. However, the condition varies a lot between individuals so this isn’t a sure thing. In fact, 25% to 30% of people with this condition experience some degree of vision loss within three years.
Possible Complications When Diagnosed with Diabetic Macular Edema
The main problem that comes with diabetic macular edema is the ongoing and irreversible loss of vision. However, this condition’s various treatments also carry their own risks. For example:
- Laser photocoagulation treatment could lead to scar tissue accumulation and damage underneath the retina, lower vision sharpness, loss of vision in certain areas, and membrane growth on the back of the eye.
- Injections into the eye could increase the risk of infections and bleeding inside the eye, speed up the formation of cataracts, increase eye pressure (which could lead to glaucoma), and cause tears in the retina.
- Vitrectomy, which is a significant surgical procedure, can potentially lead to increased risk of eye bleeding, tears in the retina, infections inside the eye, high eye pressure, and speed up cataract development.
Recovery from Diabetic Macular Edema
Vitrectomy, even though it’s a major surgery, is usually performed as an outpatient procedure. It rarely requires general anesthesia.
Preventing Diabetic Macular Edema
Educating patients is extremely important, especially when it comes to conditions like diabetic macular edema, which is a severe complication of diabetes. By providing patients with thorough information, we can help them prevent, delay, or limit the effects of diabetes. It’s crucial for patients to understand that diabetes isn’t just a condition that affects blood sugar; it’s a disease that can impact your entire body, including organs that many people don’t realize can be affected by diabetes, such as the eyes.