What is Diabetic Retinopathy?
Diabetic Retinopathy (DR) is an eye condition related to long-term diabetes. It causes damage to the retina, the part of the eye responsible for our sight, and can even lead to blindness. It’s a significant cause of serious vision loss in working adults, particularly in Western countries. To avoid vision loss, early detection and prompt treatment are essential. Projections suggest that, in America alone, the number of people suffering from diabetic retinopathy could reach 16 million by 2050, with about 3.4 million experiencing significant vision-threatening complications. Research trials have highlighted that managing blood sugar levels helps significantly in countering DR.
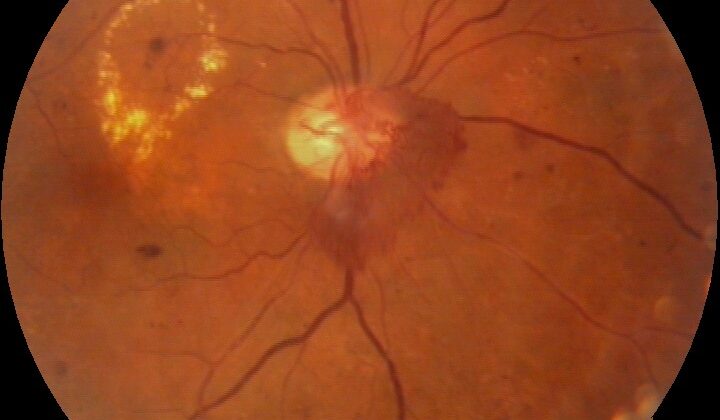
Diabetes that isn’t properly managed can lead to a host of eye issues, including cataracts, glaucoma, constant styes, and diabetic retinopathy. Diabetic retinopathy is the most common and severe amongst these, often leading to serious damage to the retina or even blindness. Factors that might worsen DR include poor control of blood sugar levels, uncontrolled high blood pressure, problems with blood fat levels, kidney disease, being male, and obesity. Eye examinations for those with DR may show features such as small balloon-like swellings in the blood vessels, leaky blood vessels causing hard deposits, swelling at the back of the eye, and new blood vessels forming due to a lack of oxygen.
Treatment might involve managing underlying health conditions, medication injected into the eye, or a laser treatment to stop leaking blood vessels. With early detection and immediate management, most DR patients can maintain decent vision.
What Causes Diabetic Retinopathy?
Diabetic retinopathy is a condition that affects people with diagnosed or undiagnosed diabetes. The chance to develop this eye problem is directly linked to a person’s age, how long they’ve had diabetes, how well they control their blood sugar levels, and their blood pressure levels.
Certain risk factors can increase the possibility of developing diabetic retinopathy. Some of them can’t be changed:
– Puberty
– Pregnancy
Others can be improved or managed:
– High blood pressure
– Obesity
– High cholesterol levels
– Poorly controlled blood sugar levels
– Kidney disease
Some new risk factors have also been identified:
– Inflammation
– Specific proteins in the body
– Hormonal influences – such as leptin and adiponectin
– Vitamin D levels
– Stress on a cellular level due to harmful substances
– Genetic factors
Risk Factors and Frequency for Diabetic Retinopathy
Diabetic retinopathy is a serious complication of diabetes and a top reason for blindness in working-age adults. According to recent data from the American Academy of Ophthalmology, almost 387 million people worldwide have diabetes, a number expected to rise to 592 million by 2035.
- About 93 million people around the globe suffer from diabetic retinopathy.
- The condition is prevalent in 77.3% of type 1 diabetes patients and 25.1% of type 2 diabetes patients.
- Of these, around 25% to 30% are likely to develop vision-threatening diabetic macular edema.
- Between 5% and 8% of patients with diabetic retinopathy will need laser treatment.
- As many as 5% of patients will need vitrectomy, which is a type of eye surgery.
Signs and Symptoms of Diabetic Retinopathy
When a person has diabetes, it’s important for medical professionals to understand their medical history. This includes how long they’ve had diabetes, what type of diabetes they have, how well their diabetes has been controlled in the past, what medication they’re taking, and whether or not they have any other health problems like obesity, kidney disease, high blood pressure, pregnancy, high cholesterol, and kidney problems.
Diabetic retinopathy is a complication of diabetes that affects the eyes. In the early stages, the person may not have any symptoms and the condition may be discovered during an eye exam. As the condition progresses, symptoms may include blurry vision, distorted vision, seeing floating spots, and vision loss.
The signs that can be observed in an eye exam for diagnosing diabetic retinopathy include:
- Microaneurysms: These are the beginner stages when an outgrowth appears around the edges of the eye and it may appear as small, round, red dots. This outgrowth may go unnoticed in the clinical examination if it is smaller than 30 µm.
- Hemorrhages: When the walls of the capillaries become weak and rupture, it may lead to dot hemorrhages in the retina.
- Hard Exudates: These are deposits of lipoprotein and lipid-filled cells which usually form a circinate ring around leaking microaneurysms.
- Cotton Wool Spots/Soft Exudates: Presence of these indicate that there are focal infarcts in the precapillary arterioles.
- IRMA (intraretinal microvascular abnormalities)
- Changes in the veins, arteries and new blood vessel formation
Diabetic retinopathy can be categorized according to the Early Treatment Diabetic Retinopathy Study (ETDRS) Classification or International Clinical Diabetic Retinopathy Disease Severity Scale. These include diagnoses such as Very Mild Nonproliferative Diabetic Retinopathy, Mild Nonproliferative Diabetic Retinopathy, Severe Nonproliferative Diabetic Retinopathy, and Proliferative Diabetic Retinopathy. The ETDRS classification also includes a special diagnosis for the end-stage vision-threatening complication known as Advanced Diabetic Eye Disease.
If Diabetic Macular Edema (DME) accompanies diabetic retinopathy, it may need to be classified separately. DME includes conditions like Focal exudative and diffuse maculopathy, Ischemic and non-ischemic maculopathy, Tractional and non-tractional maculopathy and Center involving macular edema and non-center involving macular edema.
Diabetic retinopathy is a serious condition and should be evaluated regularly for individuals with diabetes.
Testing for Diabetic Retinopathy
When getting tested for diabetic retinopathy, which affects the eyes, there are key markers to look out for. One is your fasting blood glucose level; if it’s less than 110 mg/dl, you’re in the clear. If it’s between 110 and 125 mg/dl, this suggests prediabetes, and if it’s above 126 mg/dl in two separate tests, this is an indicator of diabetes. In addition, your HbA1c level (a type of hemoglobin linked to sugar) is important, too; a normal range is between 4% to 5.6% and should ideally stay below 7%.
Given that diabetes can impact major organs, checking for potential complications related to this condition is also essential. This check can include running tests related to kidney, cardiac, and liver function, as well as evaluating blood pressure, thyroid markers, and doing a neurological examination. This testing process requires teamwork among medical professionals.
In terms of examining the eye specifically, the patient should have a thorough set of tests done including checking vision acuity, measuring eye pressure, inspecting the parts of the eye through various methods, and doing a detailed check of the back of the eye where the retina is.
Further tests like taking photos of the inside of the eye, doing a fluorescein angiography (which can help identify if there are any issues with blood flow or new blood vessel growth), performing an optical coherence tomography (which provides high-resolution images of the eye), or using ultrasound techniques can help to document any diabetic-related changes and evaluate the retina and other parts of the eye further.
More advanced methods such as ultrawide field fundus imaging and fluorescein angiogram can capture changes in a single shot. There are also other tools and methods like OCTA and artificial intelligence-based devices, which can provide detailed information on the vascular structure of the retina and detect even minor changes.
Overall, these tests and tools can provide valuable data that can aid in the early diagnosis and treatment of diabetic retinopathy.
Treatment Options for Diabetic Retinopathy
The best way to manage diabetes and keep it under control is by:
* Keeping your diabetes under strict control,
* Making sure your HbA1C levels remain under 7%,
* Making healthy changes like exercising regularly and eating a diet suitable for diabetics.
It’s important for patients to see their diabetes doctors regularly and take their diabetic medications on time. If the patient has any other health issues like high blood pressure, high cholesterol, low protein, anemia, kidney disease, nerve disease, heart conditions, or others, they should be managed with the appropriate medications and a good team of healthcare professionals.
How to Manage Non-Proliferative Diabetic Retinopathy (NPDR)
The most effective way to manage NPDR is to carefully control your blood sugar and take your antidiabetic medication as advised by your doctor. It’s also vital to control your diabetes, and keep a close eye on any changes in your eyes. If you have other health problems, they should also be addressed. A doctor or an endocrinologist should do a full exam to check for any other side effects from having diabetes.
Here is a suggested schedule for follow-up appointments:
* Very mild NPDR – check-up every year
* Mild to moderate NPDR – check-up every 6-12 months.
* Severe to Very Severe NPDR – check-up every 2-4 months.
How to Manage Diabetic Macular Edema (DME)
If your DME is affecting the center of your macula, drugs that inhibit a molecule called VEGF are the first choice of treatment. Some of these drugs are bevacizumab, ranibizumab, and aflibercept, which can be beneficial for patients depending on their baseline vision. If your DME doesn’t affect the center of your macula, laser treatment is generally the go-to choice.
Sometimes, a combination of anti-VEGF treatment and laser treatment might be necessary. Regardless of treatments, improving blood sugar control remains critical. For cases not responding to multiple anti-VEGF injections, implants that release steroids over a long period may be considered as they could help control inflammation and need less frequent administration. However, these steroids come with various risks, including an increased likelihood of developing glaucoma.
Advanced or Refractory Diabetic macular edema requires careful management and may need a higher dose or frequency of anti-VEGF medications, the use of steroid implants, and other treatments.
How to Manage Proliferative Diabetic Retinopathy (PDR)
Photocoagulation, which uses light to treat the affected areas, has long been the standard treatment for PDR. However, this approach is destructive, so alternatives like intravitreal anti-VEGF injections have been studied. One study concluded that, although the anti-VEGF drug ranibizumab was as effective as photocoagulation, it required repeated injections and was, therefore, costlier. So, a mix of anti-VEGF injections and photocoagulation, depending on the severity of the disease, may help manage PDR.
Lastly, in the case of advanced diabetic eye disease, prognosis is guarded. Depending on the severity of the condition, several treatments can be applied, including laser treatment, injections, or even surgery for cases with tractional retinal detachment. Treatment options for a painful blind eye could include laser treatment or cooling therapy, but the prognosis usually remains poor. In all cases, maintaining your overall health and keeping your diabetes under control can certainly help limit the progression of retinopathy.
What else can Diabetic Retinopathy be?
When trying to diagnose diabetic macular edema, which is an eye condition related to diabetes, doctors can sometimes confuse it with other conditions due to similar symptoms. These other conditions can include:
- Hypertensive retinopathy (vision problems due to high blood pressure)
- Blockage in the main vein of the eye (central retinal vein occlusion)
- Blockage in one of the smaller veins of the eye (branch retinal vein occlusion)
- Irvine Gass syndrome (swelling of the macula following cataract surgery)
- Post uveitic macular edema (swelling of the macula due to uveitis)
- Breakage of tiny blood vessels in the eye (ruptured microaneurysm)
- Swelling in the macula caused by a membrane (macular edema secondary to epiretinal membrane)
- New blood vessel growth under the retina (choroidal neovascular membrane)
Similarly, diabetic retinopathy, which can cause vision loss in people with diabetes, can be mistaken for these other eye conditions:
- Blockage in the main vein of the eye (central retinal vein occlusion)
- Hypertensive retinopathy (vision problems due to high blood pressure)
- Sickle cell retinopathy (eye problems due to sickle cell disease)
- Eye problems caused by severe brain bleeding (Terson syndrome)
- Ocular ischemic syndrome (eye problems due to reduced blood flow)
- Blockage in one of the smaller veins of the eye (branch retinal vein occlusion)
- Blockage in half of the main vein of the eye (hemiretinal vein occlusion)
- Vision problems due to strong pressure on the eye (Valsalva retinopathy)
- Bleeding in the retina after an injury (post-traumatic retinal bleed)
- Big blood vessels in the eye (retinal macroaneurysm)
- Eyes problems typical for thalassemia patients (retinopathy in thalassemia)
What to expect with Diabetic Retinopathy
The likelihood of successfully treating diabetic retinopathy, or diabetes-related eye disease, depends on several factors. These include how long a person has had diabetes, how well their blood sugar is controlled, any additional health problems, and their commitment to treatment.
It’s crucial that doctors help patients understand their eye condition and the need for regular check-ups. In the worst-case scenario, neglecting proper follow-up could lead to permanent and irreversible vision loss.
The early stages of diabetic retinopathy can often be reversed with well-controlled blood sugar levels. Some patients with a condition called diabetic macular edema may need ongoing support in the form of repeated injections of specific drugs into the eye.
Patients undergoing a type of laser eye surgery may also need these drugs if there is persistent swelling and abnormal blood vessels in the eye. Unfortunately, once the macular, or central part of the retina, has been detached for a prolonged period, it often leads to a poor outlook as the structure of the macular is significantly altered.
Select features seen on eye scans, such as changes to the inner and outer layers of the retina, thickness of other eye structures and presence of fluid under the retina, can help doctors predict the outcome of diabetic retinopathy.
Possible Complications When Diagnosed with Diabetic Retinopathy
Issues with vision can occur if diabetic retinopathy, a condition affecting the eye, isn’t well-managed. These threats to sight may include a swelling at the back of the eye (known as diabetic macular edema), the retina getting pulled from the back of the eye (tractional retinal detachment), and bleeding into the clear, gel-like substance in the eye (vitreous hemorrhage). These generally occur in advanced stages of diabetic retinopathy.
While there are treatments for diabetic retinopathy, such as anti-VEGF therapy, laser photocoagulation (laser treatment), and vitrectomy (surgery), they can also have complications.
Complications from anti-VEGF medication can include:
- An increase on eye pressure (IOP spike)
- Forming cataracts
- Tearing of the retina or of the posterior capsular
- Bleeding into the vitreous gel of the eye (vitreous hemorrhage)
- Retinal detachment
- Increasing tension over the macula of patients with a pulled retina
- Serious eye infection (endophthalmitis)
Complications from laser treatments can include:
- Bleeding into the vitreous gel of the eye (vitreous hemorrhage)
- Detachment of the retina and the back of the eye, especially after many laser shots in a single session
- Contrast sensitivity, peripheral vision, and night vision may all reduce after a full retina laser treatment
- Permanent blind spots in the visual field
- Worsening or development of swelling at the back of the eye after laser treatment
- Possibly worsening pallor of optic disc
Complications related to surgery (vitrectomy) can include:
- Forming cataracts
- An increase on eye pressure due to gas or oil tamponade
- Secondary tears leading to a detached retina
- In cases of long-term swelling, the macular roof may become thin, potentially leading to a hole at the macula
Recovery from Diabetic Retinopathy
Laser photocoagulation is a treatment you get without needing an overnight hospital stay, meaning it’s an outpatient procedure. It’s important for patients to control their blood sugar levels and pay attention to any other health conditions they may have. This procedure could potentially lead to an irritating condition called macular edema, which might moderately reduce vision. In such cases, patients should promptly inform their retinal surgeon, so they can assess the situation and plan for the next steps in treatment.
Intravitreal injections can temporarily increase the pressure in your eye for a few hours. However, it usually goes back to normal within 3 to 6 hours. These patients might be advised to take a tablet of acetazolamide 250 mg as a preventive measure. Following the injection, patients should come in for a check-up the next day. Afterwards, based on how stable the eye condition is, regular follow-up appointments should be scheduled. At each follow-up visit, eye tests will be done to decide whether to continue with the injections or whether to move onto a different treatment method, such as laser or vitrectomy surgery.
Post-surgery steps
After the surgery, the eye will be covered with a patch. Once the patch is removed, the eye will be cleaned and medicines will be applied. These may include antibiotic and steroid eye drops, and cycloplegic eye drops. When gases such as sf6/c3f8 or silicone oil are used in the surgery, there may be a temporary rise in eye pressure, which can be managed with appropriate medications. It’s critical to continue coming in for regular check-ups, so that doctors can monitor your recovery. If silicone oil was used, a second surgery will be needed to remove it – doctors should clearly communicate this to their patients.
Preventing Diabetic Retinopathy
The American Academy of Ophthalmology recommends that individuals with type 1 diabetes should get their eyes checked for diabetic retinopathy every year, starting five years after they were first diagnosed with diabetes. Those with type 2 diabetes should have an eye examination when they are first diagnosed and then once a year after that.
It’s crucial for patients to understand what they can expect with diabetic retinopathy. Catching it early, managing it properly, and regular check-ups depending on how severe the disease is can make a big difference. If a person doesn’t control their diabetes well, their diabetic retinopathy can get a lot worse very quickly. To slow down the progression of diabetic retinopathy, lifestyle changes are important, alongside the right medications, both systemic (affecting the whole body) and topical (applied directly to a part of the body).