What is Acute Sinusitis?
Acute sinusitis is a type of inflammation that affects the sinuses. As the sinus passages are interconnected with our nasal passages, it’s often more accurately referred to as rhinosinusitis. This is a fairly common condition, causing around 30 million people to visit primary care and resulting in an annual healthcare cost of around $11 billion. Rhinosinusitis is one of the main reasons why antibiotics are prescribed in the US and around the world. Recent guidelines highlight the necessity of using antibiotics wisely due to the threat of antibiotic resistance. Therefore, having clear treatment plans for such a widespread diagnosis is crucial.
Rhinosinusitis can be grouped into a few different categories, although this grouping is largely based on a general agreement rather than specific research:
1. Acute: symptoms are present for less than 4 weeks
2. Subacute: symptoms last between 4 and 12 weeks
3. Chronic: Symptoms persist for more than 12 weeks
4. Recurrent: there are four episodes of symptoms which each last less than 4 weeks, with the symptoms completely disappearing in between episodes.
What Causes Acute Sinusitis?
Viruses are the most common culprits causing acute rhinosinusitis, which is inflammation in your sinuses. Rhinovirus, adenovirus, influenza virus, and parainfluenza virus are among the viruses that can cause this condition.
Bacteria can also result in acute rhinosinusitis. The most common bacteria behind this are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
While it’s uncommon, fungi can cause acute rhinosinusitis too. However, this usually only happens in people with weak immune systems, such as those with uncontrolled diabetes, HIV, cancer patients undergoing treatment, or those on drugs to suppress the immune system for conditions like organ transplant or rheumatologic diseases. The offenders are typically species like Mucor, Rhizopus, Rhizomucor, and Aspergillus.
There’s a key difference between acute invasive fungal sinusitis, which affects people with weaker immunity, and allergic fungal sinusitis. The latter occurs in those with normal immune systems, and appears as a mass or lump inside a sinus cavity, often causing long-lasting symptoms. But allergic fungal sinusitis is beyond the scope of this article and will be discussed elsewhere.
Risk Factors and Frequency for Acute Sinusitis
Acute rhinosinusitis, an inflammation of the nose and sinuses, is very common and a major reason for adults getting antibiotics. In fact, 1 in 5 antibiotic prescriptions are given for this condition, making it the fifth most common reason for such prescriptions. Around 6-7% of kids with symptoms affecting their respiratory system have acute rhinosinusitis. Each year, it’s estimated that 16% of adults are diagnosed with acute bacterial rhinosinusitis (ABRS). However, since this is based on clinical diagnosis, there might be some overestimation.
It’s also estimated that only a small portion of viral rhinosinusitis cases become bacterial infections. In adults, 0.5-2.0% of viral rhinosinusitis may develop into a bacterial infection, while in children it can happen in 5-10% of cases.
Signs and Symptoms of Acute Sinusitis
Acute rhinosinusitis is a medical condition that’s primarily diagnosed based on symptoms. The three most common and clear-cut signs to look out for include thick nasal discharge along with either difficulty breathing through the nose or discomfort in the face, ranging from pressure to fullness. When patients complain about headaches, it’s crucial to determine if they are experiencing facial pressure instead since headaches alone aren’t usually associated with sinusitis. In rare cases, a type of sinusitis might result in an occipital or top-of-the-head headache, but this tends to be a chronic condition.
If a patient experiences the above symptoms for more than ten days or if the symptoms get worse after initially improving, they could be diagnosed with acute bacterial rhinosinusitis (ABRS). Other signs to be aware of include coughing, tiredness, decreased or loss of smell, toothache in the upper jaw, and a sense of fullness or pressure in the ears. Upon examination, the doctor might observe mucous or pus sourced from the osteomeatal complex, an area in the nasal cavity. This can also be seen during endoscopic rhinoscopy, a procedure where a tube with a light at the end is used to examine the nasal passage.
In children, the presentation of ABRS could slightly differ. Apart from the longer duration of cardinal symptoms or double worsening, children could also have a fever. Their nasal discharge might start watery and then turn thick and yellow-green. It’s also worth noting that the majority of bacterial sinusitis cases in children occur following a viral upper respiratory infection.
Severe symptoms like high fevers (over 39 C or 102 F) paired with purulent nasal discharge or facial discomfort lasting for three to four consecutive days right at the beginning of the illness are usually indicative of a bacterial cause. Viral illnesses, on the other hand, often resolve after three to five days. This distinction is important for determining the correct treatment approach.
Antibiotic resistance should be taken into account during the treatment decision. The factors that may lead to resistance include:
- Recent use of antibiotics, specifically within the last month
- Being hospitalized in the past five days
- Working in the healthcare sector
- Known patterns of antibiotic resistance in their community
Certain individuals could be at higher risk of complications. Risk factors for severe sinusitis include:
- Having other diseases, such as heart, kidney, or liver conditions
- Being in an immunocompromised state
- Being under 2 years or over 65 years old
Fungal acute rhinosinusitis typically presents with fevers, nasal congestion or bleeding, and facial pain, particularly in patients with weakened immune systems. Sometimes, however, it can exhibit no symptoms. If you are immunocompromised and have severe or resistant symptoms, you should consider the possibility of fungal rhinosinusitis under the guidance of a healthcare professional.
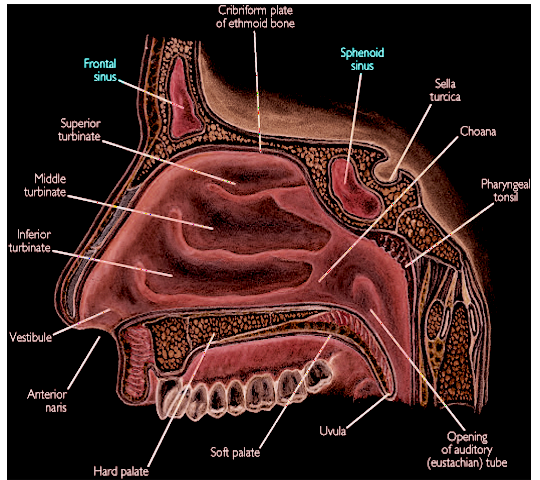
facial sinuses.
Testing for Acute Sinusitis
Acute rhinosinusitis, an inflammation of the nasal and sinus passages, is something doctors diagnose based on symptoms. They need to tell the difference between viral rhinosinusitis (VRS) and bacterial rhinosinusitis (ABRS) since they require different treatments. Understanding the local patterns of bacterial resistance to antibiotics is key to treatment.
The criteria for diagnosing rhinosinusitis involves adult patients showing two major symptoms or one major and two minor symptoms. In children, diagnosis relies more on the presence of nasal discharge than obstruction. Major symptoms can include noticeable nasal discharge, nasal congestion, facial discomfort, loss of sense of smell, and fever. Minor symptoms may include headaches, earache, bad breath, toothache, cough, fatigue, and low-grade fever.
ABRS is different from VRS by the length of symptoms (over ten days), higher fever lasting for 3-4 consecutive days at the start of illness, and a sudden worsening of symptoms within the initial ten days.
Usually, no lab tests are needed unless patients have persistent or recurring rhinosinusitis, which might signify an underlying condition like cystic fibrosis, ciliary dysfunction, or an immune disorder. However, high levels of two inflammation markers, ESR and CRP, may indicate a bacterial infection.
While endoscopic aspirate culture, a test that looks for bacteria in mucus taken directly from the sinuses, is the ideal standard, it is typically not necessary and rarely used. Samples from the nose or back of the throat often don’t correlate with sinus cultures hence their use is limited. Nonetheless, for difficult cases or patients with allergies to many antibiotics, a referral for an endoscopy might be useful.
Imaging tests for acute sinusitis are only needed if complications or other diseases are suspected. Standard X-rays typically aren’t very helpful because they don’t show inflammation well. They might reveal pockets of fluid or mucus, but these aren’t useful for telling the difference between viral or bacterial causes. A CT scan of the sinuses may be necessary to check for bone, soft tissue, dental, or anatomical abnormalities, or signs of chronic sinusitis if acute infections keep coming back. While a CT can show inflammation, it’s still not useful for differentiating between viral versus bacterial causes. Finally, MRIs offer more detailed images, which can be useful when complications involve the soft tissues or when trying to evaluate a tumor.
Treatment Options for Acute Sinusitis
The treatment for acute bacterial rhinosinusitis (ABRS) can involve either antibiotics or a careful waiting period, providing that reliable follow-up care is guaranteed. Different medical guidelines have slightly different recommendations for this process.
According to the 2015 guideline updates by the American Academy of Otolaryngology Adult Sinusitis, the first-line therapy for adults is amoxicillin, with or without clavulanate, taken over 5 to 10 days. If symptoms persist after 7 days or get worse, that’s deemed treatment failure.
Meanwhile, the Infectious Disease Society of America suggests amoxicillin with clavulanate for 10 to 14 days for children, and 5 to 7 days for adults. They classify treatment failure as a lack of symptom improvement after 3 to 5 days, or symptom worsening within 48 to 72 hours of starting the treatment.
The American Academy of Pediatrics recommends amoxicillin, with or without clavulanate, as the first-line therapy for children up to 18 years. They’re uncertain about the duration of treatment but suggest continuing for an additional seven days after symptoms subside. If symptoms do not improve or worsen after 72 hours, that’s identified as treatment failure.
When dealing with children, high-dose or regular amoxicillin doses depend on antibiotic resistance and severity of symptoms. If a child is penicillin-allergic, other drugs including third-generation cephalosporin with clindamycin, or doxycycline can be used. However, these must be administered with extra caution, especially to children.
In some cases, antibiotics might not necessarily reduce symptoms quickly or lower complication rates in adults. Many instances of ABRS can resolve on their own within two weeks.
Relief treatments such as nasal steroids or saline nose washes can be used, despite the lack of clear evidence supporting their effectiveness. Nasal steroids can help reduce swelling inside the nose, and saline rinse can help clear nasal blockages. However, antihistamines are not usually recommended, unless the patient has clear allergies, because they can thicken nasal secretions.
Fast evaluation and immediate referral for a biopsy is crucial for those suspected of having the invasive form of acute fungal rhinosinusitis. If confirmed, patients will need both medication and surgery for treatment.
What else can Acute Sinusitis be?
It’s critical to distinguish between sinusitis caused by a virus versus bacteria. Allergies can also cause inflammation in the nose and sinuses, and it is another common condition that needs to be clarified. Fungal infections can lead to inflamed sinuses, with a severe form known as invasive fungal sinusitis being more common in people with weak immune systems and carrying a high risk of death. Other less common explanations for sinus-related symptoms could include:
- Foreign objects stuck in the nose
- Enlarged or infected glands at the back of the throat
- Structural issues with the nose, like a bent septum or tumors
- Conditions affecting the movement of fine hair like structures in the nose that help trap and move out mucus and dirt, such as primary ciliary dyskinesia and cystic fibrosis
- Pain from other areas, such as a tooth infection, being felt in the sinuses
- An infection in the upper airway
What to expect with Acute Sinusitis
Acute bacterial rhinosinusitis, typically caused by a virus, usually resolves on its own or can be effectively treated with antibiotics in most cases. However, invasive fungal rhinosinusitis is a rare, yet severe kind of infection that can happen in those with weakened immune systems. This form is associated with severe illness and high death rates.
Possible Complications When Diagnosed with Acute Sinusitis
While complications from sinus infections are rare, occurring in roughly 1 out of every 1000 cases, they can spread to different areas such as the eyes (orbit), bone, or even inside the skull (intracranial cavities). Around 80% of complications related to the orbit and skull happen in the orbit – this is largely due to a very thin bone (ethmoid bone) that separates infections from the ethmoid to the orbit. These complications can potentially cause serious health issues or even death.
Orbital complications are usually classified using the Chandler classification, and they range from the least to the most severe:
- Preseptal cellulitis
- Orbital cellulitis
- Subperiosteal abscess
- Orbital abscess
- Cavernous sinus thrombosis
Complications might also affect the skull. This could lead to the development of a blood clot under the outer protective layers of the brain (subdural or epidural hematoma) or an infection of the brain’s protective membranes (meningitis). One particular severe complication is a subdural empyema, which is known to have a high mortality rate. Pott’s puffy tumor is another complication that results from a particular type of abscess (subperiosteal abscess) of the frontal bone and is usually linked with bone infection (osteomyelitis). These complications typically come from infections in the forehead sinus that spread through a system of veins (valveless diploic vein system).
Acute fungal sinusitis is another potential complication. It comes in two forms: noninvasive and invasive. The invasive type has the potential to spread to nearby structures. Finding and treating this complication early is important in order to avoid severe outcomes.
Preventing Acute Sinusitis
The majority of sudden bacterial nose and sinus infections actually have viral origins, and they usually get better on their own. Certain evidence suggests that this type of infection, known medically as acute bacterial rhinosinusitis (ABRS), can also clear up by itself. The method to determine if someone has ABRS is through a clinical diagnosis.












