What is Airway Glottic Insufficiency?
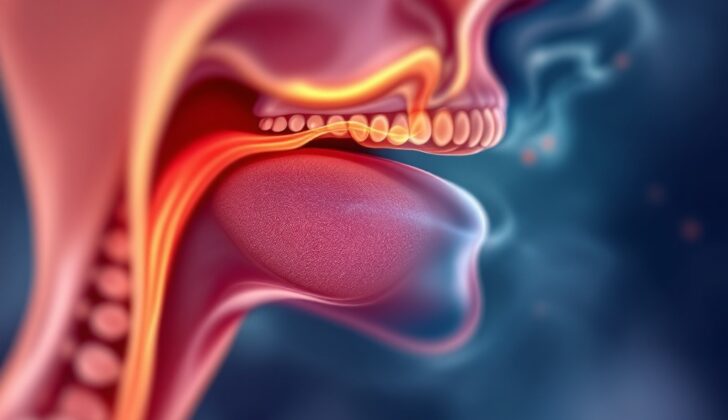
When someone has airway glottic insufficiency, it means that their vocal folds don’t fully close when they speak. This can lead to a higher chance of food or drink going down the wrong pipe and can cause laryngeal symptoms such as changes to the voice and difficulty swallowing. This condition is often caused by two main issues: vocal fold paralysis, where the vocal folds can’t move at all, and vocal fold paresis, which is when the vocal folds are weak or can only partially move. These issues are the most common reasons for airway glottic insufficiency.
People with this condition may experience a range of symptoms in the larynx, including changes to the voice, difficulty swallowing, and recurring lung infections due to food or liquid entering the lungs. There are many possible causes for this insufficiency, including growths, brain or nerve damage, trauma, functional disorders, and other contributing factors. All of these factors interfere with the vocal folds’ ability to close fully, whether they can’t move at all or can only partially move.
What Causes Airway Glottic Insufficiency?
Vocal fold paralysis and paresis are two main causes of glottic insufficiency, a condition affecting the voice box which makes it hard to speak. Vocal fold paralysis involves the complete inability to move the vocal folds, whereas paresis is a partial inability to do so. It’s important to note that these conditions aren’t diagnoses in themselves, but symptoms which require looking into to discover the root cause. The largest study of its kind showed that surgical injury is a leading cause of vocal cord paralysis on one side. Nevertheless, it’s crucial to meticulously examine patients with no history of surgery or intubation before assuming the weakness is idiopathic, meaning it has no known cause.
Doctors must rule out neurological conditions, infections and tumors affecting the brain, head, neck and upper chest areas. Conditions that impact the nerve pathway linking the brainstem to the larynx could potentially cause weak vocal folds and should be properly evaluated.
Other factors contributing to glottic insufficiency include age-related changes in the shape of the vocal folds and conditions such as sulcus vocalis, vocal fold nodules, and tumors. Injury to nerves, damage from intubation, infection, scarring or distinct vocal fold deformities can also lead to the condition. In some cases, glottic insufficiency could be present from birth, without a known cause, or as a secondary effect due to other medical procedures, like the removal of a tumor from the voice box.
Risk Factors and Frequency for Airway Glottic Insufficiency
There isn’t a lot of detailed information available about glottic insufficiency, likely due to the number of varying factors and possible underdiagnosis. Traditionally, the risk of vocal cord weakness after thyroid surgery has been thought to be around 1%. However, with more sensitive detection methods, up to 5.6% of patients may display signs of weakness after the operation. As people get older, the likelihood of having a condition called Presbylaryngeus increases, with 8% to 10% of people in some older adult facilities experiencing it. A condition known as “genuine idiopathic vocal fold paresis or paralysis”, where the vocal cords become weak or immobile for no known reason, is estimated to occur in 1 out of every 100,000 people each year, according to a large-scale study.
- Exact data on glottic insufficiency is hard to come by due to numerous contributing factors and potential for missed diagnosis.
- Historically, 1% of patients reported vocal fold weakness after thyroid surgery.
- With improved detection techniques, up to 5.6% of patients may show this weakness after thyroid surgery.
- Presbylaryngeus, an age-related condition, is found in 8% to 10% of individuals in some geriatric facilities.
- Genuine idiopathic vocal fold paresis or paralysis, a condition with an unknown cause, is estimated to affect 1 in every 100,000 people annually.
Signs and Symptoms of Airway Glottic Insufficiency
Glottic insufficiency, which can be expressed by various symptoms, is a condition that should be assessed during a patient’s initial consultation. Some patients may have a weak voice and experience discomfort when speaking. Additionally, breathlessness when speaking and a weaker cough may also be present. Patients’ medical history may disclose swallowing difficulties, recurrent chest infections, and choking episodes. Doctors should be attentive to symptoms such as throat pain, weight loss, and a neck mass, as these can suggest a serious cause like cancer.
When examining a patient with glottic insufficiency, it’s crucial to understand any additional medical factors that may be contributing to the problem. They should ask patients whether they’ve had any recent surgeries, particularly involving the neck, thyroid, or chest, as well as any incidents of neck trauma. Understanding a patient’s vocal requirements, especially important for people who use their voice a lot in their work, is also crucial. If a patient’s livelihood depends on their voice, even minor vocal changes can have a major impact. Therefore, comprehensively understanding a patient’s neurological and cardiovascular condition is essential, since conditions like stroke or neurological disorders can affect voice and nerve functions.
Doctors often use the GRBAS scale to assess patients’ voices. This tool takes into consideration aspects such as the overall quality, roughness, breathiness, weakness, and strain of the voice. Though it requires trained evaluation, it is very useful for comparing voice conditions before and after medical treatment.
An examination of the ear, nose, and throat is necessary before assessing the voice. In this examination, doctors use a flexible laryngoscope to identify any abnormal structures in the larynx. They can often find physical issues, such as neck masses or nasal polyps, which can affect voice quality. Other problems, such as chronic laryngitis or “singer’s nodules” might also be identified, impacting voice directly or indirectly. A thorough nerve examination should be conducted to understand if other nerves are affected.
Laryngeal palpation, a method to check for tenderness or excessive tension, can help rule out muscle tension dysphonia. Also, the patient may be asked to perform a certain maneuver to evaluate the condition of the cricoarytenoid joint, a joint crucial for vocal production. If vocal fold paralysis is present, this can be detected as no movement on one side, while a gentle tap may be felt on the other side.
Testing for Airway Glottic Insufficiency
Looking directly at the vocal cords is the best way to identify any abnormalities in their movement. However, the most useful method in a clinical setting often involves indirect observation with a technique called videostroboscopy.
Doctors can start the observation process using a flexible laryngoscope, which allows them to examine the vocal cords. This examination can help spot any irregularities, such as unevenness or bowing of the vocal cords, or identify any lesions that might be causing issues with the vocal cords closing properly. Paying close attention to the exact position of the vocal cords is important because it can suggest where the issue might be. For example, if the vocal cords are slightly off-center, it could indicate a problem with a nerve in the larynx, whereas the cords being in a lateral position could point towards issues with more than one nerve.
Videostroboscopy is a key tool that helps in assessing the dynamic activity of the vocal cords, allowing doctors to pick up subtle changes in the movement of the vocal cord tissue. It’s particularly useful in diagnosing issues linked to symptoms such as breathless speech.
Blood tests typically don’t offer too much insight when it comes to issues with the vocal cords. However, if a patient’s symptoms suggest that a systemic disease, like rheumatoid arthritis or an autoimmune disorder, might be the source of their vocal cord issues, blood tests become essential.
If a patient’s vocal cords are not moving, further investigation is needed to find out why. In some cases, the cause might not be apparent during the first consultation. An advanced imaging technique like a CT scan or MRI might be used to check for any issues along the paths of the relevant nerves in the neck and chest.
If there’s uncertainty about why the vocal cords aren’t moving, an electromyography of the larynx could be considered. This procedure helps to tell the difference between motion issues caused by structural problems (like mechanical fixation or joint issues) and those caused by nerve issues affecting the vocal cords.
Acoustic voice recording, while not as sensitive, can still be valuable for analyzing voice outcomes objectively and assisting in rehabilitation. By comparing results from digital analyses of voice recordings, doctors can make more informed decisions about treatment, rather than just relying on what they or the patient perceive.
Treatment Options for Airway Glottic Insufficiency
Improving the function of the voice box (or glottis) can help enhance the quality of voice, ease difficulty in swallowing (dysphagia), and reduce the likelihood of food or fluid entering the lungs (aspiration). All of these improvements can significantly enhance a patient’s quality of life. When planning treatments, it’s vital to consider characteristics such as the patient’s age, job, social circumstances, and personal preferences.
Voice therapy often plays a critical role in treating problems with the voice box, regardless of the cause. For example, patients with one paralyzed vocal cord might start with voice therapy, as many cases can get better on their own. In other situations where surgery might be unpredictable, like vocal cord scarring or specific abnormalities (sulcus vocalis), starting with conservative treatments such as reflux medication, steroids, and voice therapy can be beneficial. Voice therapy can work effectively by itself, or it can complement other surgical treatments.
Surgical procedures are used to treat problems with the voice box resulting from one-sided paralysis or weakness. The goal is to move the affected vocal cord towards the center (medialize) so that it can properly close when speaking, helping enhance the lower airway’s protection. Techniques used for this include injection augmentation, medialization thyroplasty, laryngeal reinnervation, and arytenoid adduction.
Injection augmentation involves injecting various materials into the vocal cord to restore its shape and size. This procedure can give immediate results and is a less invasive option. The materials commonly used today include absorbable hemostatic powder, collagen from cattle and humans, fat, dermal fillers like calcium hydroxylapatite, hyaluronic acid gels, and micro-ionized acellular dermis. This method can be performed under full anesthesia in an operating room or with local anesthesia while the patient is fully awake.
In a procedure called medialization thyroplasty, the vocal cord is moved towards the center using an external approach. A permanent implant is placed through a window in the thyroid cartilage. This procedure, typically performed under sedation with intraoperative voice analysis, is considered the gold standard treatment for large glottic gaps. It is the primary surgical treatment for one-sided vocal cord paralysis.
Arytenoid adduction is a surgical procedure used to restore the correct position of the vocal process, helping to improve the movement and position of the affected vocal cord. It is often used alongside other procedures when the vocal processes can’t touch but there is some remaining vocal cord movement.
Nonselective laryngeal reinnervation is a procedure that connects the ansa cervicalis nerve to the recurrent laryngeal nerve with the aim of preserving the tone of the thyroarytenoid muscle in the voice box. This procedure provides excellent results because the vocal cords remain flexible as compared to other techniques.
In cases of sulcus vocalis and vocal fold scars, techniques that release the epithelial layer are typically used along with injection augmentation, medialization, and laryngoplasty. These techniques are geared towards improving the vibrational function of the vocal fold. By addressing the underlying scar tissue or tissue deficits, these techniques can help optimize vocal fold motion and enhance vocal quality.
What else can Airway Glottic Insufficiency be?
When a doctor is trying to diagnose a condition that affects the opening in the throat known as the glottis, they might consider several possibilities. If a person has difficulty with their glottis not working correctly or causing issues with their airway, the doctor may look at these potential conditions:
- Throat (laryngeal) cancer
- Growths on the vocal cords, like nodules or polyps
- Inflammation of the vocal cords (acute corditis vocalis)
- Voice disorders due to weakened muscle controls (hypotonic voice disorders)
- Swelling of the vocal cords (Reinke’s edema)
- Growth of lumps or granuloma in the throat (laryngeal granuloma)
- Loss of voice without any physical reason (Functional aphonia)
- A condition causing spasms in the vocal cords that affect the voice (spasmodic dysphonia)
- A voice disorder where the voice is produced using wrong vocal cords (dysphonia plicae ventricularis)
- An involuntary shaking that primarily affects areas of the body like the hands (Essential tremor)
Thoroughly investigating these possibilities can help a doctor make a more accurate diagnosis.
What to expect with Airway Glottic Insufficiency
A study by Omori and others examined patients with a speech disorder called glottic insufficiency dysphonia. They looked at the effects of the size of the glottal gap (the space between the vocal cords) and the cause of the issue on voice function. The results showed that the larger glottal gaps, often associated with vocal fold palsy, lead to more severe voice function limitations than other conditions like vocal fold atrophy or sulcus vocalis. Interestingly, the size of the glottal gap seemed to be the main factor influencing voice function, rather than the underlying cause of the glottic insufficiency.
Two treatment methods, medialization thyroplasty and injection augmentation, have been found to improve voice function. Injection augmentation is a safe and effective procedure that involves injecting a material (like hyaluronic acid) which usually gets absorbed within three months. This treatment can significantly improve voice quality and protect the airway. Although recovery is usually complete for most cases of vocal fold paralysis and paresis caused by unknown or viral reasons, it can take up to a year.
However, results can be inconsistent with certain methods, like fat injections to the vocal fold. This is due to unpredictable absorption rates of the injected fat. To account for this, it is recommended to inject approximately 30% more than is required to compensate for anticipated loss. Patients should be informed that they might experience speech impairments for about three weeks post-procedure. Moreover, a recent review found no evidence that one injectable agent is comparatively better for treating unilateral vocal fold palsy.
Medialization thyroplasty, on the other hand, has been found to produce favorable outcomes. While augmentation might yield satisfactory short-term results, medialization thyroplasty might be better for long-term results, particularly for larger glottic gaps. Limited data is available regarding the long-term effectiveness of injection augmentation. One study reported that although initial voice outcomes were similar for both fat injection and medialization thyroplasty, the benefits of fat injections declined over time, leading to poorer scores on voice-related indices.
Possible Complications When Diagnosed with Airway Glottic Insufficiency
Glottic insufficiency not only influences the quality of your voice but it can also lead to issues like difficulties in swallowing and inhaling food or liquid into the lungs, which could result in constant infections in the lower part of the respiratory tract. Although the procedure commonly seen as a voice-related surgery, called medialization thyroplasty, its benefits may go beyond that. It has the potential to improve one’s ability to swallow and also prevent dangerous consequences that can arise from inhaling food or liquid into the lungs.
In a study that involved 84 patients with a condition in which one side of the vocal cords doesn’t move properly, every single one of them had voice problems, and 61% reported they had difficulties swallowing.
Preventing Airway Glottic Insufficiency
Voice therapy is very important in treating glottic insufficiency. It can be effective on its own or in combination with surgery. A voice therapist teaches patients how to use their voice most effectively and prevent habits that might not help, like unnecessary neck muscle movements when trying to speak. This kind of therapy is all about guiding patients to make the best use of their voice.