What is Middle Ear Cholesteatoma?
Cholesteatoma is a term that misleadingly suggests the presence of cholesterol or fat. Neither of these substances are actually found in these growths. Instead, cholesteatomas are non-cancerous growths that can potentially cause damage. They usually develop in the air-filled portions of the bone near the ear, such as the middle ear and mastoid and are rarely found in the ear canal.
There are two main types of cholesteatoma: congenital and acquired. Congenital cholesteatoma appears as a cyst and arises from abnormal embryonic tissue, while acquired cholesteatoma is a benign, expanding growth that comes from the skin cells in the ear and can cause inflammation, infection, and damage. The exact cause of congenital cholesteatomas is still uncertain, but our focus here is on acquired cholesteatomas, which are further divided into primary-acquired and secondary-acquired.
Primary-acquired cholesteatomas develop due to pressure changes in the middle ear that cause the eardrum to retract. This is often due to chronic middle ear inflammation. This retraction can damage the small bones in the ear and degrade the bone covering the ear. Secondary-acquired cholesteatomas occur from a direct injury to the eardrum, usually from infection or trauma. Both types of acquired cholesteatomas can be challenging to diagnose, treat, and manage due to poor blood supply.
Common symptoms include progressive hearing loss and persistent bad-smelling ear drainage that doesn’t improve with medical treatment. Acquired cholesteatomas can damage the hearing structures, disrupt ear tube function, erode the bone covering the ear, affect balance, and in rare cases, lead to complications involving the nervous system in the brain and spinal cord. Conventional treatments like antibiotics and steroids often don’t work. Because of the buildup of skin cell debris and drainage, topical treatments, like antibiotics, steroids, and antifungal agents, usually provide only temporary or superficial relief.
What Causes Middle Ear Cholesteatoma?
Cholesteatomas are typically one-sided and occur either in the middle ear or mastoid, which are located in your ear area, or at the cerebellopontine angle, an area near your brain. Cholesteatomas may develop due to the movement of squamous epithelium (a type of skin cell), growths that are a result of developmental errors, or the transformation of normal skin cells.
The formation of cholesteatomas is likely due to a combination of factors. Things like inflammation, local pressure, certain proteins in the skin, and granulation tissue (new connective tissue and microscopic blood vessels that form on the surfaces of a wound during the healing process) can contribute to the formation of cholesteatomas and the breakdown of bone.
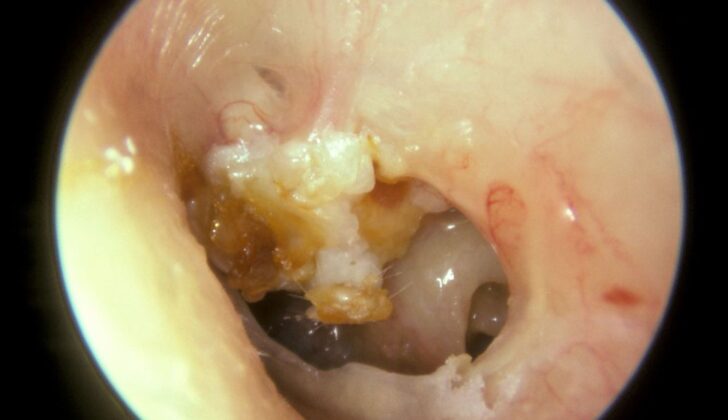
Acquired cholesteatomas, which are cholesteatomas that aren’t present at birth, are commonly divided into retraction or non-retraction pocket types. The retraction-pocket theory suggests that cholesteatomas form because of issues with the eustachian tube (a tube that connects the middle ear to the upper throat) and poor airing of the space behind the eardrum. This causes a retraction pocket to form due to negative pressure in the middle ear. This negative pressure pulls part of the eardrum inwards, often towards the top of an ear bone. As the skin layers build-up, they can form a white, pearly sac.
There are different types of cholesteatomas:
- Attic cholesteatoma
- Tensa retraction cholesteatoma
- Sinus cholesteatoma
Cholesteatomas that form in the non-retraction pockets, also known as secondary-acquired cholesteatomas, often arise from ear infections, but can also be caused by injury, such as surgery or foreign objects. There are a few theories on how these cholesteatomas form:
Epithelial migration theory: The theory suggests that a defect in the eardrum allows skin cells to move into the middle ear, leading to the formation of cholesteatomas.
Squamous metaplasia theory: This theory suggests that irritation leads to the formation of cholesteatomas due to the overgrowth of cells.
Basal cell hyperplasia theory: The theory suggests that the Prussak space (a small area in the ear) is invaded by keratin-filled microcysts, buds, or pseudopods (extensions of a cell) originating from the base layer of the skin. In this theory, retraction pockets or ruptures in the eardrum are not involved.
Regardless of the cause, once cholesteatomas have formed in the middle ear, they continue to grow and spread, causing damage to the surrounding parts of the middle ear. Cholesteatoma is a progressive condition which can eventually affect the bone, soft tissue, and nerves. If left untreated, cholesteatoma can lead to hearing loss, balance issues, loss of facial nerve function, and changes in taste. In rare cases, it may also cause complications like blood clot in the brain, meningitis (inflammation of the brain and spinal cord membranes), or an abscess in the brain.
Risk Factors and Frequency for Middle Ear Cholesteatoma
Cholesteatoma is usually not thought to be a hereditary condition, but recent research suggests it might be. This finding comes from a study in Sweden that lasted for 30 years. The results showed that if a close family member has had surgery to remove cholesteatoma, the patient’s risk of developing the condition is nearly four times higher.
- The rate of cholesteatoma is 6 to 9 cases per 100,000 people in developed countries.
- It is more common in children.
- People with a cleft palate have a higher risk of developing cholesteatoma.
- There has been a notable decline in the yearly rate of surgery for cholesteatoma, with a small increase in males over females, with a ratio of 1.4:1.
The higher rate of cholesteatoma may be influenced by differences in social and economic conditions. Factors might include more frequent usage of tubes to balance ear pressure, adenoid surgeries, access to certain types of ear examination and more focused antibiotic treatments for ear infections.
Signs and Symptoms of Middle Ear Cholesteatoma
A cholesteatoma is a skin growth that occurs in the middle ear, often caused by repeated infection. The most common symptom is painless ear discharge that is either ongoing or comes and goes. Most cases of cholesteatoma affect only one ear. Hearing loss may also occur, but it’s sometimes hard to detect due to disturbances in the ear’s sound pathway caused by the growing cholesteatoma.
Dizziness or facial weakness can be more concerning symptoms, suggesting that the cholesteatoma might be affecting the delicate structures within the ear. These symptoms occur in 1-3.4% of cases and are due to the cholesteatoma causing swelling and irritation of the facial nerve. In rare cases, cholesteatomas can lead to serious complications like blood clots in the brain, abscesses, or meningitis.
When assessing a patient with these symptoms, a healthcare provider would ask about the following:
- How long have the ear symptoms been present?
- Are there recurring instances of ear discharge, and does it have a foul smell?
- Is there a sensation of pressure in the ear?
- Are there feelings of unsteadiness or dizziness?
- Is there any hearing loss or ringing in the ears?
- Is there pain in the ear?
- Do the symptoms affect one or both ears?
- Has the patient had previous ear infections and what treatments were used?
- Has the patient had previous ear surgery or trauma?
- Has the patient had prior imaging studies of the ear?
During the physical examination, the healthcare provider may use special instruments to look inside the ear. Cholesteatomas typically appear as white or yellow masses within the ear. These masses may be hidden by discharges in the ear canal, which can be removed for a more detailed inspection. The provider may also assess the movement of the patient’s facial muscles and check for signs of damage to the structures of the ear.
Testing for Middle Ear Cholesteatoma
Cholesteatoma, a condition characterized by an abnormal skin growth in the middle ear, is usually diagnosed through a detailed patient history, physical examination, hearing tests, and sometimes imaging. There’s no need for laboratory tests or tissue samples in most cases. It’s vital to assess the risk for each patient to gauge the chances of further hearing loss, facial nerve paralysis, or complications involving balance or the brain. Although surgery is typically the primary treatment for cholesteatoma, in some instances, it might be better to monitor the condition carefully over time.
Hearing tests should be carried out before and after surgery. Such tests might involve measuring air and bone conduction, speech reception thresholds, speech discrimination, tympanometry, acoustic reflexes, and auditory brain response (in selected cases such as young children or individuals with disabilities).
Imaging can provide useful information for evaluating and managing cholesteatoma. However, some ear, nose, and throat (ENT) specialists might choose to skip advance imaging like a computed tomography (CT) scan unless the diagnosis is unclear, the extent of the disease is uncertain, the underlying anatomy is tricky to determine, or there is a concern for birth defects like atresia or craniofacial anomalies. Imaging may also be considered if specifically requested by the patient or their caregivers.
However, even with a thorough clinical assessment and imaging findings, ENT doctors must be ready for unexpected findings during surgery. Such findings could include a larger cholesteatoma mass, more severe destruction of the ossicular chain (small bones in the middle ear), a crack in the labyrinth, erosion of the roof of the middle ear, a defect in the bone covering the middle part of the ear, or issues with the facial nerve.
If imaging is carried out, a CT scan without contrast of the temporal bone (bone surrounding the ear) is typically used as it can detect bone defects. However, even high-resolution CT scans may not be able to differentiate between granulation tissue (new tissue forming during wound healing), keratinizing squamous debris (a build-up of skin cells), or fluid.
Magnetic resonance imaging (MRI) can sometimes provide additional information. Cholesteatoma will appear brighter on certain types of MRI scans. It’s particularly important to do an MRI scan if there are concerns about the disease spreading to the lining of the brain, causing an abscess, leading to the brain tissue herniating into the cavity behind the ear, causing inflammation of the inner ear or facial nerve, causing a clot in the vein draining the brain, or causing meningitis (an infection of the brain).
Some studies suggest combining a CT of the temporal bone with diffusion-weighted MRI can enhance the diagnosis. With advancements in technology, high-quality diffusion-weighted MRI may become increasingly useful for monitoring the disease after operations, and could eventually replace some follow-up surgical procedures to check for recurrence of cholesteatoma.
Treatment Options for Middle Ear Cholesteatoma
The treatment for cholesteatoma, a skin growth that occurs in the middle ear, usually involves surgery unless other serious health concerns make it too risky. While antibiotics and other treatments may slow down the growth and control the infection, they are typically not sufficient to halt the damaging process.
The goal of the surgery is to create a safe, dry ear, which involves stopping the destructive process and chronic infection. Preserving or restoring hearing is another goal, but it’s important for patients to understand that their hearing may worsen after the procedure. The surgery also aims at improving the quality of life, such as allowing water exposure, and ensuring a satisfactory cosmetic appearance.
The main surgical methods include tympanoplasty, which repairs the eardrum, and mastoidectomy, which removes the disease from the skull bone behind your ear. Sometimes, these are performed together in a procedure known as tympanomastoidectomy. The surgery might also involve ossicular chain reconstruction if there has been damage or dislocation to the small bones of the ear.
The surgery is commonly performed through a cut behind the ear, but the exact method depends on the individual case. Two main methods exist, which either preserve or remove the ear canal wall. Preserving the ear canal wall typically results in better cosmetic outcomes and can lead to better hearing, but may have a higher chance of leaving or causing recurring cholesteatoma. Removing the ear canal wall requires more frequent ear cleaning and may result in less optimal hearing outcomes, but could potentially lower the chances of a recurring cholesteatoma.
In certain situations, like when facial nerve weakness is present before surgery, a specific approach may be preferred. Regardless of the procedure used, the eardrum is often reconstructed, and special care is taken to remove the cholesteatoma from around the delicate ear bones.
The surgery is technically challenging and may not always yield satisfactory outcomes. Some patients might require a second surgery or continuous monitoring to ensure the cholesteatoma has been completely removed.
During the recovery period, a dressing is typically applied for the first day or two after surgery, and the patient might require hearing assessments. The ideal surgical approach is determined by considering the patient’s overall health, the condition of the other ear, and the characteristics of the cholesteatoma. Potential risks associated with the surgery include facial nerve weakness, worsening hearing loss, cholesteatoma reoccurrence, balance issues, and temporary taste alterations, all of which should be fully discussed with patients beforehand.
What else can Middle Ear Cholesteatoma be?
When a doctor thinks a patient might have a condition called middle ear cholesteatoma, they need to consider other health problems that might cause similar symptoms. These symptoms could include problems hearing, ear discharge, or recurring ear infections.
The conditions a doctor might consider include:
- Acute otitis media (a type of ear infection)
- Chronic suppurative otitis media (long-term, fluid-filled ear infection)
- Malignant otitis externa (a serious infection of the outer ear)
- Otitis media with effusion (ear infection with fluid buildup)
- Middle ear osteoma (a benign bone tumor in the ear)
- Typanosclerosis (hardening of tissues in the middle ear)
- Tympanic membrane perforation (a tear or hole in the ear drum)
- Cholesterol granuloma (a mass or lump in the middle ear)
- Granulomatous diseases, such as Granulomatosis with polyangiitis (also known as Wegener granulomatosis) or Histiocytosis X
- Mycobacterial infection (infections caused by certain bacteria)
- Rarely, primary auricular or temporal bone malignancy (cancer in the ear or nearby bone)
By considering all these possibilities, the doctor can run the right tests to come to an accurate diagnosis.
What to expect with Middle Ear Cholesteatoma
Generally, all cholesteatomas need to be surgically removed. Cholesteatomas are abnormal, noncancerous skin growths that can develop in the middle ear. After the surgery, most patients recover well and have a good chance of getting better. Complications after the surgery are uncommon and usually temporary.
If you are going to have surgery for cholesteatoma, it’s important that you receive clear instructions about what to do before and after the operation. It’s also vital to have a realistic understanding of what to expect. After surgery, you should have regular checkups, including having your ear examined with an otoscope (a device for looking inside the ear) and having your hearing tested.
Depending on your specific situation, you may need to have the mastoid (the part of your skull behind your ear) cleaned as often as every 3 months, or as infrequently as once a year. If there’s a chance that the cholesteatoma has come back or not fully healed, or if there’s an infection or a concern about your hearing, your doctor might have to operate again. This decision will be based on your individual situation.
Possible Complications When Diagnosed with Middle Ear Cholesteatoma
Cholesteatoma surgery doesn’t often lead to complications, but when it does, they can include:
- Narrowing of a passage in the body (Stenosis): This can be triggered by excessive tissue growth or infection. Surgical treatment might be necessary but it isn’t always needed.
- Facial nerve weakness or paralysis: This is rarely permanent and, if it happens, can be managed through a method that does not strain the nerve. If facial paralysis occurs after the operation without any visible injury to the nerve, the doctor may opt to adjust the packing to alleviate pressure on the nerve.
- In some cases, the patient may need to return to the operating room for further examination and possible relief of pressure on the nerve. In many cases, if the nerve wasn’t severely damaged, doctors may choose a ‘wait and see’ approach, as the weakness often improves on its own.
- Profound and lasting sensorineural hearing loss: This generally occurs due to a type of inner ear injury, known as labyrinthine fistula.
- Hearing loss caused by sound not being able to reach the inner ear (Conductive hearing loss): This can happen as a result of a hole in the eardrum or challenges related to the reconstruction of the bone chain in the middle ear.
- Balance disturbance.
- Inflammation of ear cartilage (Perichondritis or Chondritis).
- Persisting or repeated ear discharges, usually due to bone infection.
- Foreign bodies such as small metal fragments from the surgical drill used during the procedure.
- Changes in taste on the front part of the tongue on the same side of the surgery (Dysgeusia): This is usually temporary.
- Rare and severe complications from cholesteatoma surgery can include blockage of blood flow in a sinus located in the brain, infection of the protective membranes of the brain and spinal cord (meningitis), and a buildup of pus between the outer covering of the brain and the skull (epidural abscess).
Recovery from Middle Ear Cholesteatoma
Many patients have surgery under general anesthesia and are usually sent home within one day. The time it takes to fully recover can vary between patients because it depends on individual tolerance levels and the magnitude of the surgery carried out. Patients are advised to take off their bandage within 48 hours, or they can do so during a doctor’s appointment. Everyone who has had the procedure should make sure their ear is kept dry, use ear drops in most instances, and take pain relievers if needed.
Follow-up appointments after the surgery are also important to check on recovery and to assess healing and hearing. Some procedures may require thorough ear cleaning under a microscope in the doctor’s office. There’s a chance that a type of tissue known as granulation tissue may grow in the open area of the mastoid bone in the ear, which could potentially reduce its size and affect the final hearing result. To manage this, the removal of dead or infected tissue, application of topical steroids, and usage of gentian violet or silver nitrate might be needed.
Minor infections after surgery are common and can be caused by specific bacteria like Pseudomonas, Streptococcus, or Staphylococcus spp. Topical medication with aminoglycoside and fluoroquinolone agents, such as ciprofloxacin, along with steroids like dexamethasone ear drops are effective treatment options. If it seems like there’s a fungal infection, a cream called nystatin-triamcinolone or clotrimazole cream may be required.
Preventing Middle Ear Cholesteatoma
Preventing and managing a condition called middle ear cholesteatoma is largely about being proactive and well-informed. Middle ear cholesteatoma is a skin growth that occurs in the middle ear, and if not treated, it can affect hearing and balance. A big part of this is teaching patients why it’s essential to get treatment for chronic ear infections quickly. Letting ear infections go untreated might lead to the growth of a cholesteatoma, although doctors are still figuring out exactly why this happens.
Patients should know how to spot the early signs of this condition, like ongoing ear drainage, hearing loss, and ear pain. If you have these symptoms, you should quickly seek medical help. Regular check-ups are also very important, especially for patients who have had chronic otitis media—a long-term ear infection— in the past. These check-ups can help doctors spot and manage a cholesteatoma early on.
Doctors can give patients clear instructions on how to care for their ears, like how to stay clean, keep the ear dry, and avoid getting them wet. Following any treatments the doctor prescribes can also help lessen the chance of problems happening and improve the likelihood of successful treatment.
Patients should also understand how to look after themselves following any surgeries and what to expect in the long term. The goal is to ensure the ear remains safe and dry. Maintaining hearing is obviously important, but in some cases, it might not be the main focus. Good education can help patients and their families to be engaged and active in their own care. This approach can lead to better results and reduce the chances of developing a middle ear cholesteatoma.