What is Blepharochalasis Syndrome?
Blepharochalasis syndrome (BS) is a rare condition that mainly affects young people and involves repeated episodes of swelling around the eyes. The condition was first reported by Austrian eye doctor, Joseph Beer, in 1807. However, the term “blepharochalasis” was first used by Ernst Fuchs in 1896, which is derived from a Greek term meaning “eyelid slackening”.
What Causes Blepharochalasis Syndrome?
Several ideas and factors have been suggested concerning the causes of Blepharochalasis (BS), but what exactly causes this condition is still not clear. Although most cases only affect the eyelid, there are instances where BS has been linked with other abnormalities in the body. Because of this, some experts believe that BS could be part of a larger, more complex health disorder.
The various theories about what causes BS include hormone changes, allergies, localized forms of a skin condition called cutis laxa, and a swelling condition known as idiopathic angioedema. However, recent studies examining the disease at the microscopic level have proposed that deposits of a type of antibody called Immunoglobulin A (IgA) might have a role in causing the disease.
Risk Factors and Frequency for Blepharochalasis Syndrome
Blepharospasm Syndrome, or BS, is a rare condition, and as such, there isn’t a ton of information available. Most of what we know comes from individual case studies or small groups of cases. The disease typically starts in childhood or the teen years. People with BS usually experience episodes every 3 to 4 months for several years, but these episodes tend to happen less often as they age. Eventually, the disease quietens down and enters a resting phase. One large study of the disease found that it affected 45 women and 22 men, and the average age when the disease started was around 11.4 years.
- Blepharospasm Syndrome (BS) is not well-studied due to its rarity.
- Our understanding of BS mainly comes from case studies and small groups of cases.
- BS often starts in childhood or teen years.
- People with BS usually have episodes every 3 to 4 months for several years.
- With time, the frequency of these episodes decreases.
- The disease eventually quietens and enters a resting phase.
- A large study reported 45 female and 22 male patients with BS, with an average starting age of around 11.4 years.

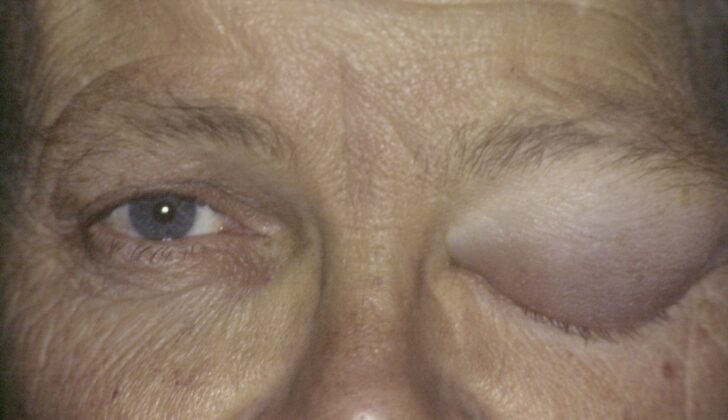
of 18 years. B. One of multiple episodes of bilateral periorbital swelling which
lasted “a few days each time”. C. Appearance at age 54 years after having had
attacks of blepharochalasis lasting a few days each time over several years.
Patient now has periorbital tissue atrophy with levator disinsertion ptosis,
loss of upper eyelid and brow fat and thinning of the eyelid skin
Signs and Symptoms of Blepharochalasis Syndrome
Blepharochalasis is a condition that generally develops during childhood or puberty. This condition is marked by repeated episodes of swelling, often affecting both upper eyelids. These episodes can happen 3 to 4 times a year and be triggered by factors like fatigue, exposure to wind, physical or emotional stress, upper respiratory infections, exercise, bee stings, or menstruation.
The swelling phase, also known as the acute stage, usually lasts anywhere from a few hours to a couple of days. During this stage, the swelling is painless and doesn’t leave a dent when pressed (known as non-pitting edema). The skin may also turn red. Some patients may experience a red eye and excessive tear production.
- Painless non-pitting edema (swelling)
- Redness of the skin
- Red eye
- Increased tear production
Over time, repeated swelling episodes can cause changes in the appearance of the eyelids and the surrounding area. The upper eyelid might droop, the skin could appear wrinkled and discolored, and the blood vessels under the skin might become more visible. In the advanced stages, there could be deformation of the eyelid’s structures, causing a rounded lateral angle and a narrowing of the eye opening (known as acquired blepharophimosis). As the eyelid’s supporting structures weaken, the upper eyelid droop intensifies and fat from within the eye socket may protrude. There are also some reports of eye bulging in one-sided cases, suggesting a possible effect on the eye socket.
This condition can be broadly divided into two phases: an ‘active’ or ‘early’ phase when the swelling episodes occur, and a ‘quiescent’ or ‘late’ stage when there have been at least 2 years without attacks.
It’s important to note that Blepharochalasis can also be part of a systemic disease. In such cases, other parts of the body may also need examining. The most common associations are with Ascher syndrome (characterized by upper eyelid swelling, double lip, and non-toxic thyroid enlargement), or Acquired Cutis Laxa, which involves redundant skin, skeletal anomalies, and multi-organ impairment.
Testing for Blepharochalasis Syndrome
To diagnose Bouvier’s syndrome (BS), doctors typically rely on observing the natural course of the disease and completion of physical examinations during the episodes of the illness and when it’s not active. The primary step involves making sure that other similar medical conditions are not causing the symptoms.
An array of other conditions may present similar symptoms as BS, therefore, establishing a comprehensive list of possible conditions (differential diagnosis) is crucial to rule these out. In some instances, the doctor may order blood tests and imaging studies. However, these are conducted mostly to exclude the possibility of other illnesses, as the results from these tests, in case of BS, often come back normal. Hence, these tests don’t directly confirm the presence of BS but they help to rule out other possibilities.
A skin biopsy, which is a procedure that involves taking a small sample of skin for testing, is usually not required for the diagnosis of BS. However, if carried out, it may provide support for the diagnosis. This is because the biopsy can identify the typical signs of BS, such as the loss of elasticity in layers of the skin (dermis).
Treatment Options for Blepharochalasis Syndrome
Treatment for BS, or Blepharochalasis syndrome, is aimed at reducing the inflammation during flare-ups and fixing any complications or long-term effects during non-flare-up periods, also known as the “quiescent stage.”
There aren’t strictly defined steps to treat the inflammation during flare-ups. Some doctors report good results using steroids, either as a pill or as a cream applied to the skin. However, these observations are based on a small number of patient cases and only show some improvements. Since long-term use of steroids can have negative side effects, especially if taken by mouth or through injections, this treatment is not generally used for all BS patients but may be considered for some specific cases. Other agents that suppress the immune system, like a topical medication called tacrolimus, have also been tested.
One study showed improvements in the flare-up stage for two patients with BS after taking an oral medication called doxycycline. This drug helps slow down an enzyme called matrix metalloproteinase. Another medication that has shown promising results in a few patient cases is the diuretic known as acetazolamide. The idea behind using this medication is that it reduces fluid build-up and swelling, which is thought to be a potential cause of BS.
Despite these various attempts to treat the inflammation during flare-ups, the main treatment strategy for BS predominantly involves surgical procedures to correct the complications or long-term effects. Surgery is typically done during the quiescent phase, which is usually about 6 – 12 months after the last flare-up. This is to lower the risk of the surgery not working. Common long-term effects in BS include an overhanging fold of the upper eyelid skin, fat build-up or disappearance, droopy eyelids, tear gland displacement, and misalignment of the eyelid corners.
All these conditions require a variety of surgical techniques that are chosen as per the individual case. Performing cosmetic surgery on the eyelids, surgery to correct droopy eyelids, and surgery on the eyelid corners are more challenging in BS patients due to unique changes in the surrounding eye tissue. Techniques to reposition tissue and to graft or transfer fat are used alongside other reconstructive techniques to repair tendons, thin sheets of fibrous tissue that attach muscle to bone, and the tear gland.
What else can Blepharochalasis Syndrome be?
Other conditions can imitate BS (Blepharospasm). During the initial phase, it can be hard to accurately diagnose, particularly when the inflammation starts, as various causes for sudden or recurring eyelid swelling must be contemplated:
- Allergic reactions
- Local eyelid infections or inflammation like stye or chalazion
- Inflammation around the eye (orbital inflammation)
- Skin conditions
- Angioedema – a kind of rapid swelling underneath the skin
- Melkerson-Rosenthal Syndrome – a rare neurological disorder
In the non-active (quiescent) phase, other conditions to consider are:
- Dermatochalasis – an excess of skin usually in the upper eyelid
- Floppy eyelid syndrome – a condition that leads to everted (flipped) eyelids during sleep
- Upper lid ptosis – drooping of the upper eyelid
- Acquired cutis laxa – a disorder characterized by sagging and wrinkling skin
- Eyelid or orbital masses – abnormal growths around the eye
A thorough patient history and physical examination can help differentiate BS from these conditions, especially if the episodes of swelling happen recurrently.
What to expect with Blepharochalasis Syndrome
BS, or Birt-Hogg-Dubé syndrome, is well-understood in terms of its progression over time, though it can show up in different ways from person to person. Some people may experience more swelling attacks or longer initial (or “early stage”) symptoms than others. Based on these factors, the number and severity of complications can vary widely in different patients.
At this time, we’re not certain how surgery affects the chance of BS symptoms returning in the future. This is an area that continues to be studied.
Possible Complications When Diagnosed with Blepharochalasis Syndrome
BS is a disease that doesn’t threaten your vision. However, it could cause complications around the eyes. Swelling of the eyelids could come and go multiple times. As a result, here are the different effects you might notice:
- Droopy, saggy skin around the eyes due to loss of fat in some areas and gain in others
- Skin might become thin, wrinkled, discolored and lose its normal texture
- Upper eyelid droopiness even though the muscle responsible for lifting the eyelid is working fine. This suggests that the connective tissue (aponeurotica) might have separated from the muscle tissue
- The outer (and sometimes inner) corner of the eyes could separate causing a rounded deformity and shortening of the length of the eye opening (leading to a condition called, acquired blepharophimosis)
- A new fold similar to an epicanthal fold could form
- The tear gland could bulge out
- The lower eyelid might become loose and its position might change
- These changes could lead to irritation on the surface of the eye
Preventing Blepharochalasis Syndrome
BS is a rare ailment, and right now, doctors don’t know what causes it, nor do they have a clear-cut cure. Despite this, it doesn’t typically lead to serious vision problems. Understanding this condition helps promptly identify it and reduces worries and uncertainties for the patient. Once we recognize the condition, we’ll explain its nature, potential triggers, and some straightforward remedies that you can apply during the swelling episodes, such as using cold compresses.
We also think it’s crucial to let you know that other illnesses can look like BS. So, if you experience swelling attacks, it’s important to seek medical attention to confirm whether it’s truly BS causing the symptoms.