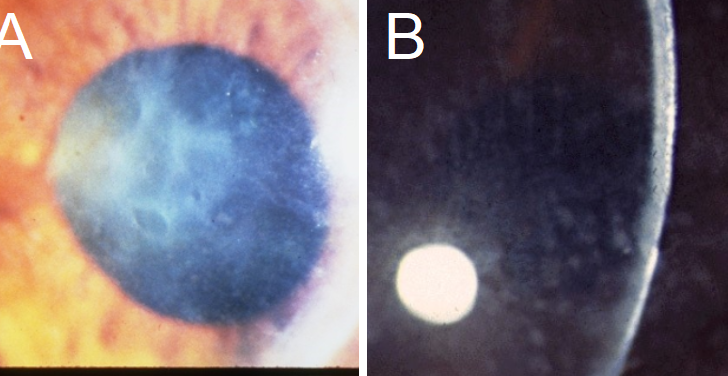
Dystrophy) presents with geographic, map-like erosions on the corneal surface on
biomicroscopy. They may present as microcysts or pebble-like. B: Meesmann’s
Corneal Dystrophy with small, bubble-like inclusions on the corneal surface with
biomicroscopy (arrows).
What is Corneal Dystrophy?
Corneal dystrophy, often referred to as CD, is a term for a group of rare, inherited eye conditions that involve abnormal deposits in the cornea but are not caused by inflammation. The term was first used in 1890 and since then, a lot of effort has been put into understanding these disorders. According to a classification brought forward in 2015, CD is grouped according to the part of the cornea it affects: the epithelial/subepithelial, epithelial-stromal, stromal, and the endothelial. Even though this has been helpful in understanding CD, there are unique cases that do not fit into these four categories.
In this article, we provide an easy-to-understand overview of the evaluation and treatment of the most commonly seen and well-understood types of CD. While some people with CD may not show any symptoms, those who do, typically experience vision loss in both eyes, usually because their cornea (the clear front surface of the eye) is not perfectly round. Other symptoms, if present, can include light sensitivity, dry eyes, swelling of the cornea, recurrent corneal erosions which can be particularly painful, especially for those whose CD affects the epithelial layer of their cornea. Age of onset varies according to the type of CD and treatment can range from non-invasive methods to corneal transplantation.
Despite its rarity, CD plays a significant role in eye diseases. The role of genetics in these diseases is crucial, especially for affected individuals who are considering starting a family. As our understanding of genetics improves, so will our ability to evaluate and treat CD.
This article falls under a series aimed at giving an overview of the evaluation and treatment of the most common types of CD. In upcoming StatPearls articles, we will provide more detailed information on these forms of CD. The main categories of CD based on the International Classification of Corneal Dystrophies are:
- Epithelial and subepithelial dystrophies
- Epithelial-Stromal Dystrophies
- Stromal dystrophies
- Endothelial corneal dystrophies
Under each category, there are specific types of corneal dystrophies such as the epithelial basement membrane corneal dystrophy under Epithelial and subepithelial dystrophies, Lattice corneal dystrophy under Epithelial-Stromal Dystrophies, Macular corneal dystrophy under Stromal dystrophies, and Fuchs endothelial corneal dystrophy under Endothelial corneal dystrophies.
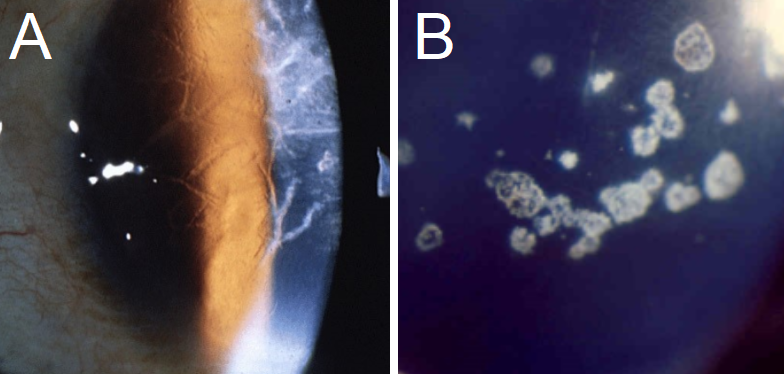
presentation of Granular Corneal Dystrophy, with crumb-like opacities separated
by clear corneal surface space.
What Causes Corneal Dystrophy?
Doctors must be able to tell the difference between corneal degeneration and corneal dystrophies. In simple terms, corneal degeneration is a group of conditions that damage the structure of the cornea due to different reasons like wounds, infections, ageing, or other environmental issues. On the other hand, corneal dystrophy is a disorder that’s separate from corneal degeneration because it’s caused by genes, which means it’s either inherited or develops spontaneously through new gene changes.
In the past, corneal dystrophy was identified by its slow and identical development in both eyes, with no clear connection to environmental factors. Also, corneal dystrophies have a higher tendency to affect vision compared to corneal degeneration.
Based on our understanding of their genetic underpinnings, corneal dystrophies have been grouped into four categories. Category 1 is for a corneal dystrophy where the altered gene(s) have been found, category 2 is for when the location of the altered gene in the body has been identified, category 3 is for corneal dystrophy without an identified altered gene or location, and category 4 is for a new or suspicious types of corneal dystrophy. Although we are still learning about some types of corneal dystrophy, many are already well understood and can be found in category 1.
It’s important to know that many corneal dystrophies are passed down from parents to children in what is called an ‘autosomal dominant’ manner. However, some corneal dystrophies are the result of gene changes that happen in families that are closely related by blood. Certain corneal dystrophies, like Lisch epithelial corneal dystrophy and X-linked endothelial corneal dystrophy, are associated with other inherited diseases too.
Although many different genes could be altered and lead to corneal dystrophy, some have already been confirmed, including genes responsible for producing several types of protein that are crucial for maintaining the structure and function of the cornea. When these genes carry certain alterations, they can lead to different types of corneal dystrophy, some of which include lattice corneal dystrophy, granular corneal dystrophy, Reis-Bücklers corneal dystrophy, and Thiel-Behnke corneal dystrophy.
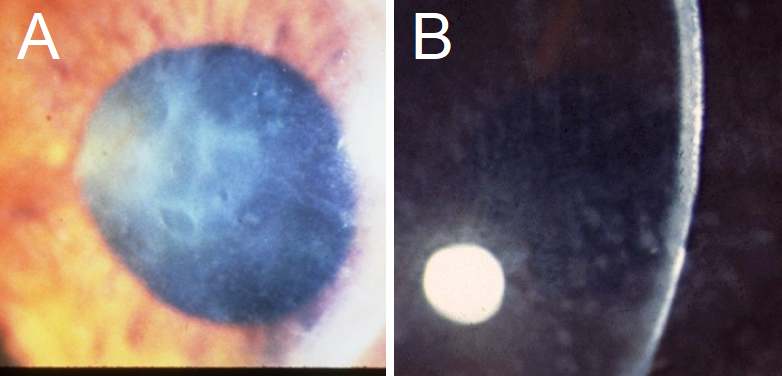
findings similar to EBMCD, with geographic, map-like erosions on the corneal
surface. Note the background corneal haze, which is often not seen in EBMCD. B:
Macular Corneal Dystrophy presents with a diffuse ground glass-like opacity, as
seen in this cornea from the side.
Risk Factors and Frequency for Corneal Dystrophy
Fuchs endothelial corneal dystrophy is the most common type of corneal dystrophy. As of 2012, it accounted for 39% of corneal transplants worldwide.
However, corneal dystrophies are still considered rare diseases. In the United States, less than 0.01% of Americans are affected by it. One study revealed that out of a million people in the U.S, around 530 have endothelial-type corneal dystrophy. Only 5 to 10 out of a million have granular, macular, or lattice-type corneal dystrophy. A very small number of families have been reported to have central cloudy dystrophy of Francois (CSCD).
Interestingly, there is a variety of demographics affected by corneal dystrophy. It affects both genders equally, although Fuchs corneal dystrophy is more common in women. People of Caucasian descent are more likely to have Fuchs endothelial corneal dystrophy. Some types of corneal dystrophy are more common in certain geographical regions. For example, granular corneal dystrophy type II is mainly seen in Europeans, and lattice corneal dystrophy type II is found in individuals of Finnish descent. Some forms of the disease can present from birth, like Fleck corneal dystrophy, congenital hereditary endothelial dystrophy (CHED), and CSCD, while others develop later in life, typically in the second or third decade. Late-onset Fuchs endothelial corneal dystrophy and lattice corneal dystrophy type II fall into this category.
Signs and Symptoms of Corneal Dystrophy
Patients with Corneal Dystrophy (CD) may or may not have symptoms. Some may experience blurry vision while others mention the sensation of a foreign body or light sensitivity. These symptoms can be ascribed to the separation of the corneal layer from the membrane. Often, this separation is likened to corneal erosion, which tends to cause more discomfort in the morning. Corneal dystrophy can generally affect sight in both eyes, although in a few cases, it may only affect one.
Medical examination often involves the use of a tool called a slit-lamp, which helps identify the different types of corneal dystrophies. Different types of CDs may present with similar symptoms which often are grouped based on the part of the cornea they are affecting. Some of these common symptoms include:
- Blurriness
- Corneal erosions
- Eye irritation
- Photophobia (light sensitivity)
- Increased tear production
- Mild visual loss
These symptoms are not limited to but often affiliated with the corneal dystrophies that affect the epithelial and subepithelial parts of cornea, the lattice and granular CD that affects the stromal (middle layer of the cornea), as well as the Fuchs endothelial CD that affects the endothelial (inner layer of the cornea) layer.
It’s important to note that while these are few common symptoms among corneal dystrophies, each type of CD may also present with specific and unique symptoms. With most patients, these symptoms could affect visual acuity and clarity of sight. If the dystrophy affects other parts of the cornea, the severity of the symptoms may progress and vary from mild to severe.
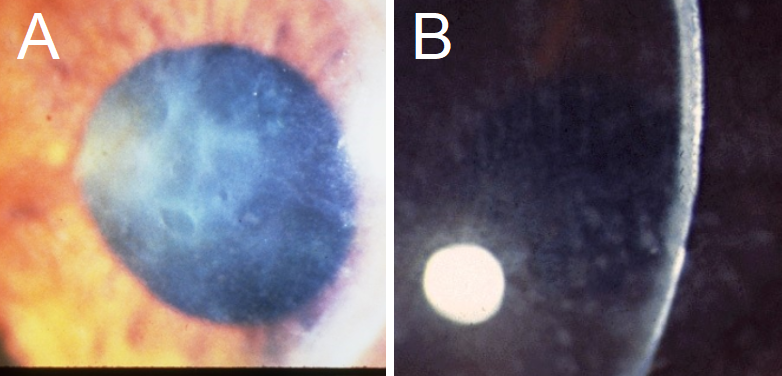
findings similar to EBMCD, with geographic, map-like erosions on the corneal
surface. Note the background corneal haze, which is often not seen in EBMCD. B:
Macular Corneal Dystrophy presents with a diffuse ground glass-like opacity, as
seen in this cornea from the side.
Testing for Corneal Dystrophy
Diagnosing eye conditions begins with a thorough eye examination. One technique used is biomicroscopy, which allows doctors to study the front surface of the eye, especially the cornea. This technique was the first way to observe physical changes on the cornea. Using light microscopes to examine tiny samples can help determine the types of corneal dystrophy (CD), a group of rare genetic eye disorders.
Different types of CDs have different characteristics. For instance, certain types of CD such as Epithelial Basement Membrane Corneal Dystrophy (EBMCD) and Meesmann CD can display a thickened part of the cornea that interacts with the outside world, called Bowman’s Layer. Granular Corneal Dystrophy (GCD) type 1 exhibits snowflake-like deposits, while Lattice Corneal Dystrophy (LCD) includes deposits similar to a protein called amyloid. GCD type 2 may show both types of deposits. Other types of CD, like Fuchs’ Endothelial Corneal Dystrophy (FECD), show a thickened part of the cornea called Descemet’s membrane and outgrowths that look like the membrane.
To diagnose some forms of CD, it’s necessary to use special dyes to stain the tiny tissue samples. These stains can identify the substances deposited in the cornea, which are often signs of the disease. Some dystrophies that result from a mutation in a protein called TGFBI, like LCD and GCD, will test positive for a red dye called Congo red, showing that they produce an amyloid-like disease. These CDs also test positive with other stains that highlight deposits in the tissue. The stain for polysaccharides and glycogen can be positive in Meesmann CD, while other stains will test positive in different types of CDs due to the accumulation of certain substances in the cornea.
Transmission electron microscopy (TEM) is another method used to help diagnose CDs. This type of microscope allows detailed viewing of cell structures that can determine one variant of CD from another. MEETING
For example, in Meesmann CD, the microscope may show collections of material and mutated proteins in the cell substance. Other types of CDs will show different findings under the microscope, like curly fibrils and intracytoplasmic vacuoles with fine material.
Treatment Options for Corneal Dystrophy
For people with no symptoms or mild cases of Corneal Dystrophy (CD), it is recommended to have regular check-ups with their doctor. These check-ups ensure that there are no common eye changes and that the CD isn’t getting worse. Regular check-ups are particularly important for slower progressing versions of CD. During these check-ups, treatment may include using glasses or contact lenses to correct vision.
For those who have noticeable symptoms, the treatment highly depends on the specific type of Corneal Dystrophy, as symptoms tend to be similar among the same kinds of dystrophies.
For example, people with an epithelial dystrophy commonly experience corneal erosions, especially in the morning. Treatments for this include artificial tears and nighttime lubricants to reduce friction and keep the cornea moist. Also, non-steroidal anti-inflammatory drugs (NSAIDs) may be used to reduce pain, as well as protective contact lenses. In severe cases, options like superficial keratectomy, anterior stromal puncture, and phototherapeutic keratectomy are available to help relieve symptoms.
Stromal dystrophies, those which involve the stroma (a layer of the cornea), often lead to vision loss. In these cases, more invasive measures like automated lamellar keratoplasty (ALK) and deep automated lamellar keratoplasty (DALK) may be performed to remove the affected cells and tissue.
Endothelial Dystrophies, those affecting the innermost layer of the cornea, can now be treated with techniques like Descemet’s stripping endothelial keratoplasty (DSEK) and Descemet’s membrane endothelial keratoplasty (DMEK). These procedures offer faster recovery, better post-surgery vision, and decreased chance of graft rejection because they don’t disturb the front part of the eye surface.
Other new therapies on the horizon include gene or enzyme therapy, stem cell therapy, and lipid-based therapies. Also, Rho-kinase inhibitors could be used to decrease intraocular pressure and help with cell adhesion and replication in the cornea. Since CD is mostly genetic, genetic counseling is advised for those considering having children.
What else can Corneal Dystrophy be?
Corneal dystrophies, or CDs, are eye conditions that can sometimes be confused with one another due to their similar symptoms. In fact, even using a microscope to look at the eye may not provide a clear distinction between different types of CDs. Genetic testing, however, can often help identify the specific type of CD a patient has.
Many symptoms of CDs can also be caused by other eye conditions. For example, recurrent erosions of the cornea, or scratches on the eye surface, can occur due to reasons other than genetic disorders. These can include eye trauma or the natural aging process. Corneal degeneration, a weakening and thinning of the cornea, may happen as we grow older or due to injury, and not necessarily because of CD. Similarly, certain symptoms might not be indicative of CDs at all. These could be due to bacterial or herpes infections, damage to specific nerves leading to less sensitivity in the cornea, or calcium deposits in the cornea due to chronic inflammation, conditions causing high levels of calcium, and other diseases.
Other signs that might be mistaken for CDs can include the presence of blue-white nodules beneath a layer of the cornea, or changes in the cornea similar to those seen in a specific type of CD in older people. If these changes are seen in children or teenagers, it might indicate the presence of a CD.
Patients experiencing instances of a scratched eye surface could also be dealing with herpes infections, foreign bodies in the eye surface, dry eyes due to immune system disorders, and other conditions. Eye pain and disturbances in vision, which are often seen in the serious eye condition glaucoma, can also be seen in some CDs, or even occur alongside CDs. Therefore, it is often necessary to test for these conditions when diagnosing a CD.
Furthermore, some types of CDs can have similar symptoms to each other, so genetic testing can sometimes be important in telling them apart. For example, genetic testing can help distinguish between two such CDs when they both cause repeated cornea erosions.
Finally, certain CDs can present with symptoms related to other diseases. These can include signs of high levels of fat in the blood, reminiscent of inherited diseases impacting fat metabolism, and conditions affecting specific tissue layers in the body that could produce eye symptoms similar to those seen in CDs.
What to expect with Corneal Dystrophy
The eventual outcome for those with corneal dystrophy (CD) largely depends on the specific form of the condition they have. Nevertheless, most kinds of CD cause a gradual reduction in how well a person can see. Posterior Amorphous CD is pretty harmless, only causing slight issues with eyesight. Certain types of CD, for instance Posterior Polymorphous CD, Meesmann CD, and Fleck CD show up early in life, but usually get worse quite slowly, sometimes needing very little treatment.
However, some forms, like FECD, can get worse faster, to the point that surgery may be necessary by the time a person is in their sixties. Furthermore, MCD, GDLD, and Congenital Stromal CD can have serious symptoms from an early stage, risking major loss of vision if the patient doesn’t undergo a transfusion of cornea (keratoplasty).
There is also a risk that the CD could return after a corneal graft operation, leading to the need for further treatment. This is more likely to happen in stromal dystrophies. For instance, reports indicate that the recurrence of LCD nine years after corneal grafting is 60%, while GCD could return in an average of 2-3 years after the operation. Recurrence has been reported for other types as well though it is not common. However, it must be pointed out that not all re-treatments are due to the return of the disease. In the case of patients with FECD, the need for further corneal grafts is typically a result of issues like the donor cornea detaching, failure, or loss of endothelial cells, rather than the CD making a comeback.
Possible Complications When Diagnosed with Corneal Dystrophy
People with untreated Corneal Dystrophy (CD) can face complications, including issues related to surgery. If left untreated, severe Corneal Dystrophy may lead to deteriorating vision, which could result in significant vision loss. Corneal erosions, another issue linked to Corneal Dystrophy, can be painful and bring about secondary keratitis because of excessive eye rubbing.
The usual treatment for Corneal Dystrophy involves removing the damaged corneal tissue and replacing it with donor tissue. This procedure, however, brings with it risks such as infection, the possibility of the body rejecting the new tissue, and the risk of the treatment not succeeding. It’s been found that up to 35% of patients might experience tissue rejection within the first year following the procedure.
Preventing Corneal Dystrophy
Patients should be made aware of the limited scope of surgical procedures. Many eye disease conditions, such as dystrophies, may come back within a few years even after a cornea transplant operation. For slow-progressing conditions like CD, it is often recommended to use non-invasive treatments like glasses or contact lenses instead.
Patient education about safety measures following surgery is crucial to help them achieve the best healing outcomes. Techniques like using bandage contact lenses can be beneficial to avoid the loosening of surgical stitches or the shifting of the transplanted cornea.
Furthermore, the use of artificial tears in the morning could be a useful method for reducing the pain caused by corneal erosion.