What is Corneal Ulcer?
A corneal ulcer is a defect in the lining (epithelium) of the cornea (front part of the eye) that extends into the tissue beneath it (stroma). This condition can pose a serious risk to vision and is considered a potential eye emergency. It usually involves tissue decay and destruction. Even with quick treatment, people can suffer from serious health issues including cornea scarring or rupture, development of eye pressure problems (glaucoma), lens clouding (cataracts) or other eye conditions, and even vision loss. If a bacterial infection of the cornea (keratitis) is left untreated, it could lead to an infection inside the eye (endophthalmitis) and even loss of the eye. It’s estimated that between 30,000 to 75,000 new cases of corneal ulcers occur in the USA every year, with infections being the cause of around 12.2% of corneal transplants. That’s why it’s so important this condition is quickly identified and treated, and that an eye examination is arranged in a timely manner.
The cornea consists of six layers: The epithelium, Bowman’s membrane, the stroma, Dua’s layer, Descemet’s membrane, and the endothelium. Corneal ulcers can be categorized by cause, location, and which layers of the cornea they affect. They can be caused by infections from bacteria, viruses, fungi, and other microorganisms, as well as non-infectious causes like nerve damage, vitamin A deficiency, or a type of ulcer known as Mooren’s ulcer. The ulcer could be located at the center, close to the center, or at the edge of the cornea and it can be surface-level or deeper.
There are many factors that could increase the likelihood of corneal ulcers such as eye injuries, dry eyes, vitamin A deficiency, long-term eye inflammation, eyelid issues, eyelash problems, protruding eyes, inability to close the eyes completely, wearing contact lenses, and the misuse of steroid eye medication. People with poor nutrition, diabetes, alcoholism, drug addiction, cancer, HIV/AIDS, and a weakened immune system also have a higher risk. For people with autoimmune disorders and those with weakened immune systems, the risk of non-infectious corneal ulcers is increased. Long-term use of contact lenses, improper cleaning of contact lenses with tap water, use of contaminated lens solution, and improper lens wear are key risk factors for infectious ulcers. When an infection is involved, a corneal ulcer can become a serious, eye-threatening condition.
What Causes Corneal Ulcer?
Bacterial: Corneal ulcers, which are often infected, are usually caused by bacteria. A corneal ulcer starts off as keratitis (cornea inflammation) when bacteria enter the cornea through a damaged area. This damage is often due to wearing contact lenses, scratching the eye, or eye injuries. Other risk factors for corneal ulcers are diabetes, previous eye surgery, chronic eye disease, use of corticosteroids, contaminated eye drops, and farming. The usual culprits are bacteria like Staphylococcus aureus, coagulase-negative staphylococcus, and Pseudomonas aeruginosa. However, in cases of keratitis caused by more than one type of microorganism, fusarium is often involved, usually due to injuries. Other bacteria that can cause this include Staphylococcus pyogenes and Staphylococcus pneumoniae.
Viral: The Herpes simplex virus (HSV) is a common cause of viral keratitis and the top cause of one-sided infectious corneal blindness in the developed world. Eye inflammation can also be caused by Varicella-zoster virus (VZV) and cytomegalovirus, but these are less common. HSV-1 is usually the type involved.
Fungal: Only 5% to 10% of all corneal infections are caused by fungi. These are more common in hot, humid parts of the country and usually occur after an eye injury and exposure to plant or vegetable material. Fungi that are often involved include Aspergillus, Fusarium, Scedosporium apiospermum, phaeohyphomycetes, Candida albicans, and other Candida species.
Protozoan: Acanthamoeba, a type of protozoan found in freshwater and soil, can cause keratitis and corneal ulcers, mainly in contact lens wearers.
Pythium: Pythium keratitis is a recently discovered type of keratitis caused by the protozoan Pythium insidiosum. This species is potentially dangerous and can cause severe vision-threatening effects.
Autoimmune disease: Not all corneal ulcers are infectious; some have non-infectious causes. Peripheral ulcerative keratitis (PUK), a type of non-infectious keratitis, is often linked with many systemic diseases. After anterior uveitis, PUK is the second most common eye complication of autoimmune disorders. Collagen vascular diseases are responsible for 50% of all PUK cases, and rheumatoid arthritis is usually the cause. PUK is also associated with Wegener granulomatosis, relapsing polychondritis, polyarteritis nodosa, Churg-Strauss syndrome, and microscopic polyangiitis.
Risk Factors and Frequency for Corneal Ulcer
Keratitis, a condition that can lead to corneal ulcers, results in about one million clinic and emergency room visits each year in the U.S. People of all backgrounds can have corneal ulcers, but those who wear contact lenses, particularly extended-wear lenses, are more susceptible. In a study from California, young women ages 25 to 34 had the highest rate of bacterial corneal ulcers, with an incidence of 60.3 per 100,000 person-years.
In developed countries, ocular herpes infections, majorly caused by the strain HSV-1, have a reported rate of 5 to 20 cases per 10,000 people each year. Only a small portion of these cases, between 1.3% to 12%, are bilateral (affecting both eyes) and tend to occur in younger patients, typically being more severe.
Fungal keratitis, although rare, is more common in young men who work outdoors. It’s more common in developing countries and its occurrence varies according to the climate. In the UK, a study identified the rate of fungal (mycotic) keratitis as 0.32 cases per million person-years. However, in tropical and subtropical environments, fungal keratitis can account for up to half of all infectious keratitis cases. On the other hand, peripheral ulcerative keratitis, which can occur independently or as part of an underlying autoimmune disorder, has an estimated rate of 3 cases per million each year.
Signs and Symptoms of Corneal Ulcer
When investigating the cause of corneal ulcers, doctors ask about certain risk factors. These include wearing contact lenses and habits regarding their storage and hygiene, past eye surgeries, recent eye injuries, exposure to herpes, specific work environments, and taking medications that can suppress the immune system. They also ask about the patient’s pain, such as how severe the pain is and how quickly it began, as well as other symptoms like sensitivity to light and blurry vision. It’s essential to know the patient’s general health history as well since conditions like diabetes, rheumatoid arthritis, and certain blood vessel diseases can make someone more likely to develop corneal ulcers.
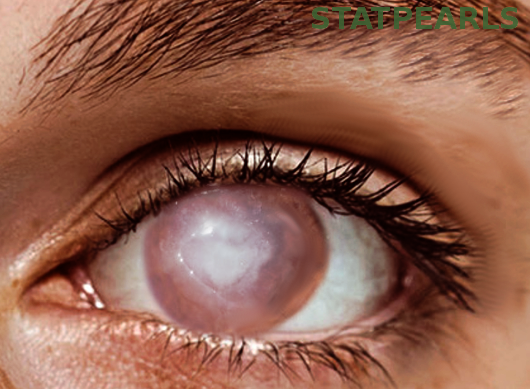
Different tests are performed as part of the physical examination, such as checking vision sharpness and eye pressure (unless a ruptured eye or perforated ulcer is a concern), and pupil reaction. The doctor also examines the eyelids and conjunctiva – the clear tissue covering the white part of the eye. They look for signs of infection or inflammation, such as redness, swelling, and discharge, along with ciliary flush, which is redness around the cornea. A more detailed examination with a slit lamp, a type of microscope used for eye exams, helps determine the size, location, and shape of the ulcer or ulcers. If there’s a chance the eye has ruptured, they’ll do Seidel’s test.
Corneal ulcers can be caused by different types of organisms, and each causes slightly different symptoms:
- Bacterial Ulcer Symptoms: Pain, redness, feeling like something’s in the eye, sensitivity to light, tearing, watery discharge, and swelling.
- Fungal Ulcer Symptoms: Blurry vision, redness, swollen eyelids, sensitivity to light, pain, and irritation.
- Viral Ulcer Symptoms: Pain, redness, sensitivity to light, blurry vision, and a gritty feeling.
Testing for Corneal Ulcer
If a patient has a bacterial corneal ulcer, they might experience light sensitivity (photophobia), redness around the white part of the eye (conjunctival injection), swiftly occurring pain, and their vision might get worse to a certain extent. When viewed with a slit lamp (a special microscope for eyes), these ulcers look like well-defined infected areas with swelling and fluid build-up in the middle layer of the cornea (stromal inflammation and edema). To guide the treatment, an eye doctor often needs to take a sample (culture).
A patient with corneal ulcer caused by Herpes Simplex Virus (HSV keratitis) usually shows similar symptoms to those with bacterial corneal ulcers such as the feeling of a foreign body in the eye, light sensitivity, redness around the eye, and blurred vision. On the slit-lamp exam, the doctor will typically find tree-like structures (dendritic lesions) that are visible under a unique dye (fluorescein).
Fungal infections are typically slower to develop and usually don’t cause as much redness as bacterial infections. On a slit lamp exam, the fungal lesions appear as gray-white, dry, feather-like areas with irregular edges. Ulcers caused by yeast appear on the surface as white, elevated patches with clear borders.
A patient with an eye infection caused by Acanthamoeba (a type of amoeba) usually has significant pain, which often exceeds what you’d expect from a physical examination. Intense light sensitivity is also common. The exam may reveal several types of lesions, such as small, widespread epithelial lesions, dendritic-like lesions, or ring-shaped infiltrates. The surefire way to diagnose this is by directly scraping the cornea, examining the tissue under a microscope (histology), or identifying Acanthamoeba DNA through a test (PCR).
Patients with peripheral ulcerative keratitis or PUK (which can be due to an underlying autoimmune disease) might already have a diagnosis, or the corneal ulcer might be the first sign of the disease. The damage seen in PUK is usually shaped like a crescent and located at the border of the cornea (limbal region). The patient may show other symptoms of their underlying disease, such as swollen and painful joints or rashes. Examinations for these patients may involve a complete eye examination, lab work, and imaging to help identify or monitor the underlying autoimmune condition.
The descriptions and investigations (tests) for different types of corneal ulcers vary and include bacteria, fungi, viruses, amoebae, and other microscopic creatures. Please consult an eye professional for diagnosis and treatment options.
Treatment Options for Corneal Ulcer
When treating bacterial corneal ulcers and keratitis, the first step usually involves using antibiotic eye drops, often a type called fluoroquinolones, such as ciprofloxacin or ofloxacin. However, due to increasing antibiotic resistance among common eye bacteria, it’s recommended to get a culture and sensitivity test for all corneal ulcers. This is especially important for large, centrally located ulcers with significant involvement of the stroma, the dense, transparent part of the cornea.
If a corneal ulcer is caused by the gonococcus bacteria, hospitalization for treatment with intravenous antibiotic ceftriaxone and topical antibiotics is necessary. For severe infections caused by other common bacteria, systemic antibiotics could be needed. Those who can’t or won’t comply with treatment might also need to be hospitalized. The use of additional corticosteroids is controversial but might benefit certain patients with a positive culture for non-Nocardia bacterial keratitis, particularly if they also have a central ulcer or low vision.
Treatment for herpetic keratitis usually involves topical antiviral drugs and additional topical steroids. In the U.S., the most common topical antiviral is trifluridine, whereas in Europe, topical acyclovir is the first choice. Other alternatives include ganciclovir, which is also effective against varicella zoster virus (VZV) and cytomegalovirus (CMV) keratitis. Oral acyclovir or valacyclovir are also options, with oral valganciclovir being the preferred treatment for CMV stromal keratitis. But patients need close monitoring with this medication because of potential serious side effects, such as aplastic anemia, a serious condition affecting blood cell production.
Fungal ulcers usually have worse outcomes than bacterial ones because there are fewer treatment options. The common treatment for these is natamycin, a topical polyene. Another option is Amphotericin B, but its use is limited due to toxicity. Voriconazole, a third-generation triazole was found to be less effective than natamycin in treatment trials.
For Acanthamoeba keratitis and corneal ulcers, treatment usually consists of removing the diseased corneal cells (epithelial debridement) and prescribing several months of anti-amoebic therapy. This often includes the drugs chlorhexidine and poligexametilen biguanide. In severe cases, medication like diamidines, fluconazole, itraconazole, neomycin, and iodine-containing medicines may be added.
For those with peripheral ulcerative keratitis associated with autoimmune and collagen vascular diseases, they should be treated with systemic immunosuppressants, cytotoxic agents, and managed collectively by a rheumatologist and an ophthalmologist. These patients need to have careful monitoring and blood tests regularly while on immunosuppressants medication.
All patients with corneal ulcers should see an ophthalmologist immediately, within 12 to 24 hours. In cases of suspected bacterial ulcers, an immediate ophthalmologic consultation is essential to guide appropriate antibiotic treatment. They would typically perform a culture test on the ulcer to determine which antibiotics would be effective.
What else can Corneal Ulcer be?
If someone goes to the doctor with red, painful eyes, there are numerous conditions the doctor might consider:
- Pink eye (Conjunctivitis)
- Scratches on the cornea (Corneal abrasions)
- Nonulcerative keratitis (Inflammation of the cornea)
- Foreign body in the eye
- Exposure keratitis (Inflammation due to dry eye)
- Iritis (Inflammation of the iris)
- Acute angle-closure glaucoma (a type of eye pressure problem)
- Chemical burns to the eye
- Thermal burns to the eye
- Atopic keratoconjunctivitis (Allergy-related eye inflammation)
- Rosacea keratitis (Eye problem related to rosacea, a skin condition)
- Shield ulcer (A type of corneal problem)
- Keratitis medicamentosa (Inflammation caused by eye drops)
- Episcleritis (Inflammation of a thin layer of the eye)
- Scleritis (Inflammation of the white part of the eye)
- Anterior uveitis (Inflammation inside the eye)
The doctor needs to correctly diagnose the right condition to provide the best treatment.
What to expect with Corneal Ulcer
The outlook for healing depends on factors like the cause, size, and location of the ulcer, as well as the response to treatment. Other important factors include how severe the ulcer is, the overall health of the eye, the strength of the immune system, and how timely and consistent the treatment is. The patient’s socioeconomic status, any complications, and individual differences also play a role. In general, surface-level ulcers tend to heal better compared to deeper ones.
Possible Complications When Diagnosed with Corneal Ulcer
If corneal ulcers are not treated properly, they can lead to various complications. These include:
- Corneal scarring
- Vascularization or formation of blood vessels in the cornea
- Perforation in the cornea
- Glaucoma, a condition that damages your eye’s optic nerve
- Irregular astigmatism, which affects the shape of the eye
- Cataracts or hazy areas in the lens of the eye
- Endophthalmitis, a severe inflammation inside the eye
- Vision loss
Recovery from Corneal Ulcer
Recovering well after a keratoplasty, a surgery that swaps a damaged cornea with a healthy one from a donor, is key to not only repair the eye’s structure but also improve the patient’s vision and ease any pain or discomfort. After having this surgery, the patient will stay in a recovery room where doctors will regularly check the eye for complications or possible infections. Part of their eye may be temporarily covered for protection.
To fend off infections, control inflammation, and boost healing, the patient will typically be given topical drops or ointments. It’s important to use these medications consistently and as prescribed. Regular check-ups with an eye doctor are also crucial, so the doctor can monitor the healing process, look for signs of the body rejecting the donor cornea, and make changes to the medication if needed. Putting on an eye shield or glasses with protective lenses can help prevent accidental harm to the eye while it’s still in the early stages of healing.
Patients should avoid touching or scratching their eyes to keep the donor cornea from becoming dislodged and to lessen the chance of infection. High-intensity activities, swimming, and any pursuits that might expose the eye to harmful substances should be avoided until the eye has healed. Keeping the eye clean and avoiding any irritants are also key to a smooth recovery.
It’s important that patients follow their eye doctor’s instructions closely when it comes to medication, taking care of their eyes, and restricting certain activities. Rehabilitation for the vision may also be required to help the vision improve once the eye has healed. This may include vision therapy sessions or wearing glasses to correct vision. Patients should also be aware of signs that might indicate their bodies are rejecting the cornea, including increased pain, redness, light sensitivity, and decreased vision. If patients experience any of these symptoms, they need medical help immediately.
Patients and their families need to understand the importance of sticking to the plan for care after the operation and of recognizing any signs that complications might be brewing. For some patients, dealing with the recovery process can be a tough time. Giving them emotional support and words of encouragement can make their experience more positive. Remember that everyone recovers differently and that following an eye doctor’s instructions closely is key. Regularly discussing progress with the healthcare team can help ensure the best recovery after keratoplasty surgery.
Preventing Corneal Ulcer
The biggest risk for developing corneal ulcers is the use of contact lenses. This is why it’s crucial to educate patients properly on how they should be using their contacts. Specifically, patients need to know the correct ways to insert, clean and store their lenses, along with understanding the importance of not wearing them for extended periods of time or overnight.
Additionally, they should be informed about the potential dangers of swimming or showering while wearing contacts, buying contacts from unauthorized sellers, and the greater chance of infection from wearing lenses for long durations. This education is a critical component in preventing such ulcers.