What is Duane Retraction Syndrome?
Duane retraction syndrome (DRS), previously known as Stilling-Turk-Duane syndrome, is a condition caused by the lack or incomplete development of a certain nerve, called the abducent nucleus and nerve. This issue leads to irregular control of the muscle that helps move our eye sideways, known as the lateral rectus, which becomes controlled by another nerve called the oculomotor nerve. Similar problems happening in one or more of the nerves that originate from the brain, known as cranial nerves, are generally categorized under congenital cranial dysinnervation disorders (CCDD). These issues may either be primary due to the non-existence of normal nerve control or secondary if other cranial nerves take over the control function.
Evaluating and managing Duane retraction syndrome can be quite difficult, requiring a careful and considered approach.
What Causes Duane Retraction Syndrome?
Ever since it was first brought up in a medical book all the way back in 1887, we’re still not completely sure what causes DRS (Duane Retraction Syndrome). However, what we do understand is that it’s usually because the sixth cranial nerve, which is responsible for our ability to move our eyes, doesn’t fully develop or is missing altogether. As a result, our third cranial nerve, which usually controls most of our eye movements, also has to power the outside muscle of the eye.
When we’re still embryos, our eye muscles come together as one mass, controlled by the third cranial nerve. Then, as the embryo grows a little larger, these muscles separate out. That’s when the fourth and sixth nerves would usually come in. However, under certain unknown circumstances, the sixth nerve doesn’t develop, which means the third cranial nerve ends up controlling the muscle that helps to move the eye outward.
Other issues with the eyes and other body parts suggest that these certain unknown circumstances could occur as the body is developing between the 4th and 8th weeks of pregnancy. People with DRS are generally 10 to 20 times more at risk of also having other birth defects. These commonly include abnormalities in the skeleton, ears, eyes, and nerves.
Some of these abnormalities may include cleft palate, limb deformities, abnormal ear shape, deafness, and issues with cranial nerves. Eye-related issues may include different-colored irises, droopy upper eyelid, cloudy lens, and unusual eye movements, among others.
DRS generally occurs at random, but around 10% of the time, it runs in families. Research has linked different genes with different forms of DRS. For example, DRS has been associated with the DURS1 gene, CHN1 gene, and the SALL4 gene. These genes could impact the development and guidance of the sixth cranial nerve, which as we now know, plays a key part in DRS.
The HOXA1 gene, which helps create or keep alive the neurons in our cranial nerves, has also been linked to DRS. Syndromes associated with this gene and DRS include Bosley-Salih-Alorainy Syndrome and Athabascan Brainstem Dysgenesis syndrome.
Risk Factors and Frequency for Duane Retraction Syndrome
DRS is a condition that affects 1 to 4% of people who have misaligned eyes. Most of the time, it only affects one eye, but in about 10% of cases, it can affect both eyes. Women are more likely to have DRS, and it’s more common in the left eye than the right. It’s been suggested that because women have higher levels of estrogen during the development of the baby in the womb, plus a higher chance of inflammation, they may have a higher risk of blood clots. Clots, especially when they travel from the right to left side of the body, can affect the left carotid artery (a major blood vessel) and cause abnormal cell death and incorrect nerve connection, which typically affects the left eye.
Although DRS is naturally present from birth, most people don’t show symptoms until later. The average age when people start showing symptoms for types I, II, and III of DRS is around 13.5 years, 23.0 years, and 21.9 years respectively.
Signs and Symptoms of Duane Retraction Syndrome
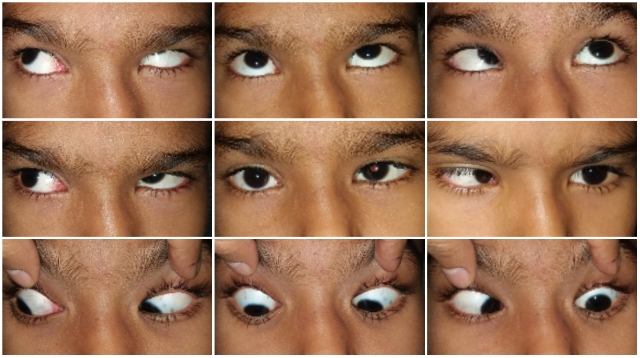
Parents might seek help for a child with Duane Retraction Syndrome (DRS) if they notice unusual head positions, drooping eyelids when the affected eye moves inward, restricted eye movement, and abnormal eye movements. DRS is characterized by several specific features:
- Limitation in moving eye outward: This key symptom happens due to decreased control of the eye muscle that helps in looking sideways. This issue is more than what is typically found when the eyes look straight – helping in distinguishing this from another condition called sixth nerve palsy.
- Unusual head position: Often seen in one-sided cases, the child might turn their head to maintain a clear, unified vision and compensate for the limitation in eye movement. The head might turn towards the side of the affected eye in inward turning DRS cases or away from it in outward turning cases.
- Eye retraction: This sign of DRS is typically accompanied by a narrowing of the eye gap when the eye moves inward.
- Eye shoots upward or downward: These moves can be sudden or gradual. Gradual elevation or lowering of the eye as it moves inward may be associated with a vertical misalignment of eyes when looking straight.
- Alphabet patterns: Patients might show specific patterns when they look towards the affected field of vision. The most common pattern is the V pattern, but A and no pattern can also occur.
- Eye turn (Strabismus): Finally, patients can display various types of eye turn, which will be discussed in further sections.
These symptoms can help medical professionals diagnose and manage this syndrome better.
Testing for Duane Retraction Syndrome
Evaluating someone with Duane Retraction Syndrome (DRS) follows the same process as those who have crossed or misaligned eyes. The assessment includes checking vision and refraction (how well the eye can focus), looking at the eyes, evaluating eye movements, testing how well the two eyes work together, and carrying out other necessary tests.
A large group of DRS patients (between 30% and 70%) are far-sighted or have astigmatism (a problem with the eye’s shape) of more than 1.5D. Some of these patients may also need more effort to focus their eyes; hence, cycloplegic refraction (a special type of focus test where the eyes’ focusing mechanism is relaxed) is vital for planning treatment.
Most people with DRS on one side can avoid lazy eye by adjusting their head posture. However, up to a quarter of patients with DRS in both eyes can develop lazy eye.
Inspecting the eyes and evaluating eye movements helps categorize the type of DRS. There are three types, classified based on analysis of the electrical activity of eye muscles:
– Type 1: This is the most common type, which is when the eye can’t move outwards well, but can move inwards normally or slightly less than normal.
– Type 2: This is the least common type, where the eye struggles to move inward but can move outwards normally or a bit less than usual.
– Type 3: In this type, there’s limited or no ability to move the eyes in and out.
A modified classification divides each type based on how much the eyes deviate from the midline. This classification is more helpful for surgical planning and management. Usually, single-sided Type I DRS patients’ eyes tend to turn inward, while Type II DRS patients’ eyes turn outward, and Type III DRS patients have an equal chance of their eyes turning inward, outward, or staying in the midline.
Bilateral DRS, where both eyes are affected, is less common. It’s divided into three types depending on whether there’s fusion (the ability of the eyes to work together to form a single image), a distinctive inward or outward deviation of the eye, or a particular eye movement pattern.
As DRS can come with many other eye and health concerns, a comprehensive evaluation involving multiple specialists is necessary.
Treatment Options for Duane Retraction Syndrome
Non-surgical treatment methods for Duane retraction syndrome, or DRS, include glasses, contact lenses, prism glasses, and standard therapy for amblyopia. The use of botulinum toxin has also been studied with results showing short-term benefits.
When the condition is severe enough to cause notable eye misalignment, an unusual head position, eye retraction, or unusual up and down eye movements, surgery can be considered. However, patients should be informed that no treatment or procedure can fully correct the abnormal eye movements seen in DRS.
The surgical options depend on the alignment of the eye. For esotropic DRS, where the eye turns inward, there are many approaches including moving one or both of the medial rectus muscles which control eye movement. This can potentially correct eye alignment but must be carefully done to prevent further complications. This procedure is usually considered when there is tightness in the medial rectus muscle and minimal co-contraction happening in the eye. Another approach is to move both the medial rectus muscle and the lateral rectus muscle to reduce abnormal nerve signals.
There’s also the option to move the vertical muscles to create an outward pull on the eye, though this can potentially lead to other issues including changes in vertical eye position. Vertical muscle transposition may also require a second procedure or could potentially put the patient at higher risk for anterior ischemia syndrome, which deprives the anterior segment of the eye of blood. Superior rectus transposition, where only the top muscle is moved, poses less potential risk.
For exotropic DRS where the eye turns outward, the lateral rectus muscle can be moved to correct the eye alignment. There’s also an innovative procedure where the insertion of the lateral rectus muscle is relocated, minimizing the anomalous signals and muscle stiffness, although its efficacy is not yet well-established in the literature.
Eye retraction and abnormal eye movements upward or downward can also be managed surgically. This can be done by splitting the lateral rectus muscle into two parts, relocating the lateral rectus to the side of the eye socket, or cutting the vertical rectus muscle. These operations aim to treat the cause, whether mechanical or nerve-related.
What else can Duane Retraction Syndrome be?
Doctors considering a DRS (Duane Retraction Syndrome) diagnosis need to rule out other conditions that could cause similar symptoms. These could include eye movement disorders like sixth nerve palsy, infantile esotropia, Mobius syndrome, and congenital ocular motor apraxia. Usually, each of these conditions comes with additional clinical features, making it possible to distinguish them from DRS. For instance, infantile esotropia typically involves abnormal fast eye movements and cross-eye viewing, Mobius syndrome may come along with feeding and speech troubles, and congenital ocular motor apraxia involves difficulty producing horizontal eye movements.
Esotropic DRS and congenital sixth nerve palsy can be differentiated through certain signs. For example, eye retraction (pulling back) when looking to the side is seen in DRS but not in sixth nerve palsy; the misalignment of the eyes tends to be lesser in DRS patients with the same level of side gaze limitation as in sixth nerve palsy patients; and the degree of side gaze restriction varies in DRS patients when looking up and down, unlike in those with sixth nerve palsy.
The third group of conditions to be considered are those that lead to symptoms similar to DRS (eye retraction when looking to the side and limitation of side gaze) but are entirely different in their causes. These types of conditions are referred to as “Acquired retraction syndrome.” Some mechanical causes include a break in the bone of the eye socket, inflammation in the eye socket, thyroid eye disease, and spread of cancer to the bones around the eye. Other causes could be related to nerve damage due to a head injury, or the spread of cancer to the brain, or brainstem tumors like glioma. In these cases, details of the patient’s health history, double vision, trauma, or previous surgery help to differentiate them from DRS.
What to expect with Duane Retraction Syndrome
If treated correctly, isolated DRS often leads to a great long-term outlook for one’s vision. A variety of non-surgical and surgical treatments can effectively manage symptoms like abnormal head posture, eye retraction, rapid movements, and misalignment of the visual axes. Recent advancements in surgery, like the shifting of vertical muscles, also contribute to improving eye movements in patients with DRS.
Possible Complications When Diagnosed with Duane Retraction Syndrome
Potential complications can occur during an eye procedure for correcting an inward turning of the eyes (esotropia). Here are the main possibilities:
- Undercorrection and residual esotropia – This can happen if a) not enough of the horizontal muscle is adjusted, b) the medial rectus muscle (MR) tightens over time, or c) the muscle transposition doesn’t generate enough force.
- Consecutive exotropia – This could occur if a) too much tension is created by the vertical muscle transposition, b) the muscle controlling eye movement towards the nose (ipsilateral MR) is weak, or c) muscle tightening worsens due to transposition.
- Induced vertical deviation – This may occur due to an imbalance between the transposed muscles, or if the moved muscle slips or recedes. If too much muscle is used for transposition, vertical action of the muscle may also weaken, leading to induced vertical deviation.
Preventing Duane Retraction Syndrome
It’s important for doctors to clearly explain to patients and their families why a comprehensive body check-up and genetic analysis are necessary. This is because Duane retraction syndrome (DRS) can sometimes be linked with other bodily disorders. If the patient doesn’t need surgery, it’s crucial to stress the significance of following treatment plans, like wearing glasses or using prisms, and continuing with lazy eye treatment. In cases where surgery is required, it’s essential to tell patients that no surgery can fully restore eye movement. This is because the root cause, which is an unusual communication within the nervous system, cannot be cured.