What is Episcleritis?
Episcleritis is a condition that causes sudden inflammation in the episclera, which is the thin tissue layer that lies between the outermost layer of the eye, called the conjunctiva, and the white part of the eye, known as the sclera. The episclera is made of loose connective tissue and gets its blood supply from the anterior ciliary arteries, which are offshoots of the main eye artery.
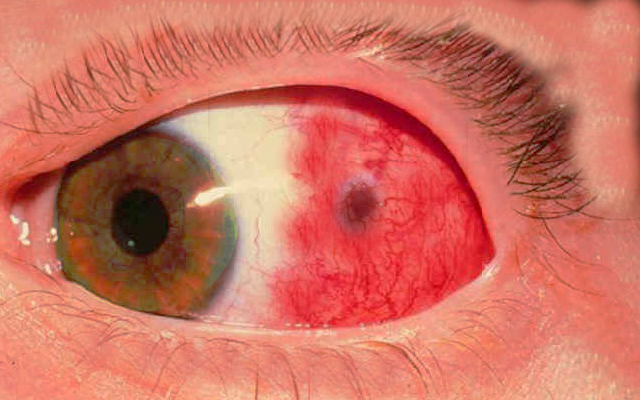
Episcleritis can affect either one or both eyes and can take three different forms: it can be spread out (diffuse), restricted to a section (sectoral), or form a lump (nodular). Most of the time, the cause is unknown but it can sometimes be linked to diseases that affect the body’s connective tissue, immune system diseases, and even certain infectious diseases.
Patients with episcleritis usually notice redness in their eyes and may feel some mild discomfort or pain. But their ability to see should remain normal. Discharge from the eyes or sensitivity to light (photophobia) are not usually symptoms of this condition.
What Causes Episcleritis?
Most cases of episcleritis, an eye condition causing inflammation, occur without a known cause. However, around 26% to 36% of people with this condition have it linked to a health disorder that’s responsible for causing the inflammation. These disorders include conditions like rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriatic arthritis, systemic lupus erythematosus (form of chronic autoimmune condition), reactive arthritis, relapsing polychondritis (recurrent inflammation of the cartilage), ankylosing spondylitis (type of arthritis affecting the spine), polyarteritis nodosa (inflamed arteries), Behcet’s disease, Cogan’s syndrome, and granulomatosis with polyangiitis (old name Wegener granulomatosis).
Some infections such as Lyme disease, cat scratch fever, syphilis, and those caused by the herpes virus are also associated with episcleritis. However, these kinds of infections are not as common a cause as the autoimmune and collagen vascular diseases (diseases affecting your body’s connective tissues) mentioned above.
Risk Factors and Frequency for Episcleritis
Episcleritis, a condition usually affecting young to middle-aged women, is rarely seen in children. There is a lack of clear records about how common this condition is among the general public. Regardless, it’s known that a form of this condition called ‘diffuse episcleritis’ affects around 70% of patients, making it considerably more common than the ‘nodular’ form, which only affects about 30% of patients.
Interestingly, people with systemic collagen-vascular disease and autoimmune diseases are more likely to get episcleritis. A study found that about 30% of patients experience repeated episodes of episcleritis, either in the same eye or in the other one. However, the actual number of episodes might be even higher because some people may treat themselves without consulting a doctor.
Signs and Symptoms of Episcleritis
Episcleritis is a condition that causes redness in one or both eyes. It often affects just one eye around 80% of the time, but sometimes it can also affect both eyes at once. In some cases (15% to 30%), there might be a small lump of inflamed tissue present, making the condition be named as nodular episcleritis. When there’s no lump, the condition is usually called diffuse episcleritis. People with episcleritis may experience tenderness or mild pain in the affected area but usually don’t have any discharge, light sensitivity, or reduced vision quality.
To distinguish between episcleritis and a similar condition called scleritis, doctors may need to evaluate the depth of the congested blood vessels in the eye. Scleritis tends to cause severe pain, light sensitivity, tearing, and sometimes can affect vision. An eye drop containing 2.5% phenylephrine can be used to see if the inflammation is only affecting the episcleral tissue, the outermost layer of the sclera or eye white. If it is, the blood vessels will appear to fade, and the eye will look relatively white and symptom-free after about 10-15 minutes. If the deeper scleral vessels are inflamed, they won’t fade with the eye drop and the eye will continue to look very red.
People with acute episcleritis often also have other eye surface diseases such as ocular rosacea, dry eye syndrome (keratoconjunctivitis sicca), and allergic eye inflammation (atopic keratoconjunctivitis).
During the clinical examination, if the patient has a history of joint or muscle pain, skin rash, psoriasis, diarrhea, mouth or genital ulcers, drug abuse, any possibility for sexually transmitted infections, or any other symptoms that could suggest a linked or underlying disease, the doctor may recommend further laboratory testing.
Testing for Episcleritis
If your doctor suspects a systemic disease – a condition that affects your entire body – due to the signs and symptoms you’re displaying, they will likely order a variety of lab tests and imaging. These diseases might include conditions like rheumatoid arthritis, Crohn’s disease, ulcerative colitis, psoriatic arthritis, lupus, reactive arthritis, relapsing polychondritis, ankylosing spondylitis, polyarteritis nodosa, Behcet’s disease, Cogan’s syndrome, and granulomatosis with polyangiitis. These can all potentially cause episcleritis, an inflammation of the white part of the eye. Other infectious diseases like Lyme disease, tuberculosis, syphilis, and shingles (herpes zoster) can also potentially lead to episcleritis.
Some of the tests that the doctor might do include a variety of blood tests. These tests measure different things in the blood like the count of different kinds of cells, the rate at which your red blood cells settle at the bottom of a test tube (which can indicate inflammation), the presence of proteins which might suggest diseases like rheumatoid arthritis or lupus, the presence of a gene that can indicate a risk for certain conditions like ankylosing spondylitis, and the presence of certain antinuclear and antineutrophil cytoplasmic antibodies (which are substances produced by your immune system that could indicate an inflammatory condition).
If Lyme disease is suspected, your doctor will order a Lyme disease test. If they think you may have tuberculosis, you’ll be given a skin test and a chest x-ray. If syphilis is considered a possibility, you’ll be tested using a test called an RPR or VDRL and given a confirmatory test called an FTA-ABS or a treponemal-specific assay.
If your episcleritis persists and doesn’t respond to treatment, your doctor might consider a tissue biopsy, which involves taking a small sample of tissue to be examined in a lab. It’s very rare, but sometimes episcleritis may actually be a sign of a serious condition like granulomatosis with polyangiitis or Cogan’s syndrome, which could be fatal if not treated. So it’s important for your doctor to consider these possibilities in their differential diagnosis.
Treatment Options for Episcleritis
Episcleritis, an eye condition causing redness and discomfort, is typically mild and short-term, often getting better on its own within 2 to 21 days. A common recommendation for relief of symptoms is to use chilled artificial tear drops at least four times a day. However, some people might need additional treatment if their symptoms are more severe.
Medical intervention might include prescription eye drops that contain mild corticosteroids, medicines that reduce inflammation. These include fluorometholone 0.1% or loteprednol etabonate 0.5%. However, while unlikely, these mild steroids may raise eye pressure. So, it’s important for patients to have a follow-up visit 1 to 2 weeks after starting this treatment to check their eye pressure and to assess how well the episcleritis is healing. If there is no improvement, doctors may prescribe a stronger corticosteroid, prednisolone acetate 1%. This is a more powerful anti-inflammatory drug, but it also has a higher risk of increasing eye pressure. In extreme cases, oral steroids could be prescribed, but this is not common as episcleritis is usually not severe enough to warrant this treatment.
Potential side effects of steroid eye drops to be aware of include an increased risk of cataracts and a higher susceptibility for infection, so it’s crucial to use the medication judiciously.
Oral non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen could be used as an alternative to steroid eye drops or if the inflammation hasn’t improved with steroids. However, these should be used cautiously as they may cause stomach ulcers. They are usually prescribed together with antacids to help protect the stomach.
NSAID eye drops, such as diclofenac 0.1% and ketorolac 0.5%, could somewhat help with the mild pain and inflammation linked to episcleritis without affecting eye pressure. However, they are not typically very effective and have been linked to certain side effects, such as corneal melting (for diclofenac 0.1%) and a significant burning sensation upon use (for ketorolac 0.5%). Because of this, the benefits of using these types of eye drops may not outweigh the potential risks and side effects.
What else can Episcleritis be?
The condition, episcleritis, is rarely misunderstood or diagnosed late. There are several other eye conditions that might seem like episcleritis at first, but a careful history taking and eye exam usually rules them out.
For example, Contact lens-associated red eye (CLARE) can look like episcleritis. However, people with this condition usually have a history of sleeping in their contact lenses and typically have pain in one eye, sensitivity to light, and excessive tearing, but still maintain good vision. Signs like inflammation of the conjunctive and cornea, corneal cloudiness and swelling, and in severe cases, inflamed iris also distinguish CLARE from episcleritis.
Next, acute conjunctivitis also needs to be ruled out. This general term refers to viral, bacterial, allergic, and toxic eye infections. Symptoms may include a red eye with discharge, sensitivity to light, itching or burning, and swollen eyelids. The presence of specific inflammatory cells on the inside of the eyelids will also help identify the type of conjunctivitis.
Phlyctenular conjunctivitis, triggered by an immune response to foreign substances in tear film and often linked to eyelid inflammation, also presents with sectoral redness and swelling on the covering of the eye.
Inflammation of pinguecula, a common eye condition particularly when cited with dry eye, needs to be excluded too. The sure sign of this condition is inflammation coupled with pinguecula.
Iritis may initially seem similar to episcleritis. Yet specific signs of iritis such as inflamed deposits on the inner surface of the cornea and cells and “flare” in the front chamber of the eye, and concentrated redness in the area surrounding the cornea (ciliary flush), make it identifiable.
Finally, scleritis, the most crucial condition to differentiate from episcleritis, comes with a slower onset of redness, pain, tearing, light sensitivity, and sometimes decreased vision. People with scleritis often describe a deep, severe pain radiating from the affected eye. The white part of the eye tends to take on a reddish-purple shade that does not go away when eye drops are applied. More than half of the people with scleritis also have an underlying autoimmune condition or blood vessel inflammation, and they need more aggressive treatment, typically with corticoids and anti-inflammatory drugs. Severe cases might require other medicines that suppress the immune system, with potentially serious side effects such as azathioprine, methotrexate, and mycophenolate mofetil.
What to expect with Episcleritis
The outlook for people with episcleritis is usually positive. Most people suffering from this condition do not have an associated underlying condition. While many people will experience recurrent flare-ups, the side effects from the inflammation and the treatments are rare and can usually be controlled without any significant intervention.