What is Globe Rupture?
Globe rupture, along with globe laceration, globe perforation, or open globe injuries, are different types of eye injuries that need immediate attention and treatment. All these injuries are collectively referred to as ‘globe rupture.’ Two main ways the eye can be damaged like this are through the eye being pierced, cut, or ruptured due to a blunt force.
A piercing eye injury means that something has entered the eye, but hasn’t gone all the way through. Sometimes, this can leave something lodged in the eye. If an object goes in and out the eye, it’s referred to as a ‘perforating injury’.
In the United States, there are about 3 instances of globe rupture for every 100,000 people each year. Doctors can diagnose a globe rupture by asking about the history of the injury and conducting an eye examination, typically using a device called a ‘slit lamp’ and a technique called ‘fundoscopic evaluation’. Images or scans may not always be accurate in diagnosing a globe rupture, but they can be used as supporting evidence. If there is a high chance that the eye has been ruptured, it is recommended to see an eye specialist (ophthalmologist) immediately.
What Causes Globe Rupture?
In children, eye injuries like a rupture of the eyeball often happen due to sharp objects such as scissors, usually occurring at home. In adults, these types of eye injuries are often the result of accidents at work, attacks, or car accidents. For older adults, falling from a standing position is a common cause of eye rupture.
An extensive study from China revealed that if the patient has an eye injury due to an object entering or going through the eye, it is usually due to an explosion in children under ten. For those over ten, such injuries are more likely to be caused by a foreign object.
Eye rupture can also result from gunshot injuries, sports-related injuries, stab wounds, and injuries from explosions.
Risk Factors and Frequency for Globe Rupture
Globe rupture, a type of eye injury, tends to happen more frequently in males than in females. This injury is almost twice as likely in men below the age of 40 compared to those older than 40. The main causes of globe rupture in men under 40 are usually assault and workplace accidents. However, for people above 75 years of age, the most common cause is typically falls from ground level.
The eye injury can occur at any place on the eye, but it’s most commonly located close to the limbus, at the upper nasal quarter of the eye if the trauma is indirect. Substance abuse has also been linked to a higher incidence of eye trauma.
- Globe rupture is more frequent in males than females.
- Men under 40 experience this injury almost twice as often as men over 40.
- Assault and workplace injuries are the main causes in men below 40.
- In people older than 75, the most common cause of this injury is falls from ground level.
- The injury can happen anywhere on the eye, but it’s usually located at the upper nasal quadrant, near the limbus when the trauma is indirect.
- There’s a higher occurrence of eye trauma in people who misuse substances.
Signs and Symptoms of Globe Rupture
When a patient comes in with a ruptured eye globe, doctors usually ask about what caused the injury to the eye or around the eye. Patients often experience sudden eye pain and vision loss following an injury that may have punctured the eye. This could happen due to a variety of reasons such as bits of glass or metal, shotgun or BB pellets, or wood shavings, particularly from wood grinding. A rupture can also happen due to a blunt force trauma caused by incidents such as falling, fainting, seizures, car accidents involving airbags, or attacks with blunt objects.
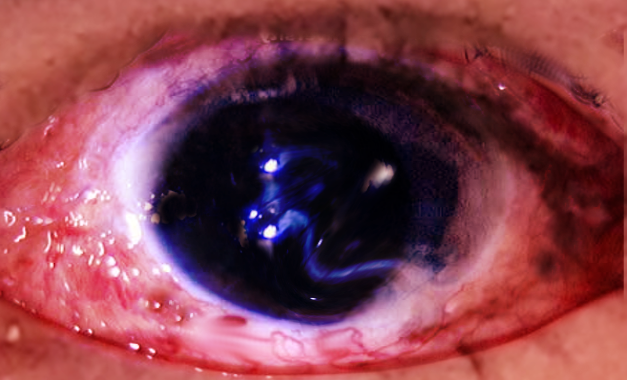
During the physical examination of patients with a suspected ruptured globe, doctors conduct a thorough eye examination. The first thing they typically check is the patient’s basic vision capacity. After that, they use a tool called a slit lamp to inspect the front part of the eyeball and the front chamber of the eye. It’s important to gently check the conjunctiva (the clear tissue covering the front of the eye) for any defects, visible foreign objects, or cuts. They pay special attention to the area of the ‘sclera’ (the white of the eye) located behind the insertion of the rectus muscles (muscles that control eye movement), as this is a common site for eye globe rupture due to its thinness. The doctor will also look at the pupil’s response to light and its shape, noting any irregularities. It’s essential that the eye not be pressed during assessment, therefore tests like tonometry (measuring the pressure inside the eye) and turning the eyelids inside out are usually avoided at the start.
Testing for Globe Rupture
After an eye injury, doctors usually check for a more serious condition known as a globe rupture, which affects the round part of your eye (the eyeball). However, this evaluation is done only after doctors have ensured you’re breathing normally and your heart is working properly. Usually, these injuries greatly affect a person’s ability to see clearly.
To assess your ability to see, doctors might use a Snellen chart or near card, which are tools with letters or symbols of different sizes. If your vision is severely impaired, doctors might check if you’re able to count fingers, see a moving hand, or detect flashes of light.
Doctors also use an instrument called a slit lamp to inspect your eye. It helps them to spot things like foreign objects that may have penetrated the eye, tears in the cornea (the clear outer layer at the front of your eye) or the sclera (the white part of your eye), a bulging part of the uvea (middle layer of the eye), or abnormal iris (the colored part of your eye) shapes like pointed or “teardrop” pupils.
They might also use a special type of dye to stain the cornea and sclera. If the patient has a wound in their eye, the dye may stream out of it, indicating a condition called Seidel sign. However, even if this sign is absent, the eye could still be ruptured. Doctors avoid performing this test if it’s clear that the eyeball has ruptured.
A maxillofacial computed tomography (CT) scan, a specific type of X-ray, can assist doctors in managing globe rupture, although it’s not a substitute for a direct assessment of your eyes. A CT scan is the preferred technique for spotting foreign objects inside the eye.
Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to produce detailed images of the inside of your body. Doctors avoid MRI scans for eye injuries if they suspect metallic foreign objects in the eye, as this may worsen the injury. However, if the CT scan doesn’t reveal any metallic objects but a foreign object is still suspected, they may consider an MRI scan or a plain X-ray.
Ultrasound, which uses sound waves to create images, can also find foreign objects in the eye. However, because it requires direct contact with the eye, doctors usually avoid it. Putting pressure on an injured eyeball could extrude, or force out, its internal contents, making the injury worse.
Treatment Options for Globe Rupture
If you suspect that your eye has been seriously injured or ruptured, it’s vital that you seek immediate medical attention from an eye specialist, known as an ophthalmologist. Before heading to the hospital, it’s best to avoid eating and drinking and protect your eye with a shield or cup. Do not try to remove any foreign bodies from your eye by yourself; this should be done in a surgical setting by a professional.
While you wait for treatment, try to avoid any activities that might increase the pressure in your eye, such as heavy lifting or straining. You may be advised to rest in a reclining position to help ease the pressure. Medications to control nausea and pain may be given. Also, if you’re not up-to-date on your tetanus shots, you may receive a booster, as open eye injuries can lead to tetanus infection.
Avoiding an increase in eye pressure is also important when considering anesthesia for your eye surgery. Some common anesthesia drugs might raise this pressure, so your doctors will choose the safest option for you. It’s also recommended to receive antibiotic eye drops before surgery to potentially lower the risk of a severe eye infection, known as endophthalmitis.
(The surgical process usually begins as soon as possible to avoid worsening the vision and to lower the risk of infections. Initially, the ophthalmologist will repair the wounds in the cornea or sclera (two structures in your eye) using tiny sutures, or stitches. They’ll also remove any trapped tissue and reform the front part of your eye. Once the wound is patched up, you’ll receive more antibiotics directly into your eye to help avoid infections.
If the injury has affected the back part of your eye, you might require further surgical intervention. However, this doesn’t always involve stitches, as this could potentially damage your eye further. Instead, the body often naturally seals these wounds within a week through fibrous growth. But this growth can sometimes lead to complications such as retinal detachments and vision loss. In such cases, you might need additional surgery such as a vitrectomy, which involves removing the vitreous gel in the middle of the eye. If a foreign body is trapped inside the eye, removing it may also be necessary, especially if it could harm the eye over time.
After the surgery, you’ll need to use antibiotic eye drops and possibly oral antibiotics to prevent infections. The specific antibiotics prescribed will depend on the cause of your injury and the most likely bacteria involved. An infectious disease specialist can provide updated recommendations on the best choices for you.
What else can Globe Rupture be?
If someone comes to the hospital with face injuries after a blunt force or sharp object has hit them, or if they’re experiencing pain or can’t see well after an injury, doctors need to consider the possibility of a ruptured eyeball (“globe rupture”). This is a severe condition that needs immediate attention. To determine if the patient has a globe rupture, other conditions that show similar symptoms should also be taken into account:
- Bleeding below the clear surface of the eye (subconjunctival hemorrhage)
- Break in the bones of the eye socket (orbital wall or floor fracture)
- Scraped cornea (corneal abrasion)
- Bleeding inside the eye socket (orbital hemorrhage)
- Ulceration on the transparent front part of the eye (corneal ulceration)
- Glaucoma (eye disease causing optic nerve damage)
- Inflammation of the iris following trauma (traumatic iritis)
What to expect with Globe Rupture
The final vision outcome of a patient after a severe eye injury, known as a globe rupture, largely depends on their initial visual acuity or how well they could see at the time of the injury. Other factors that can negatively affect the final vision include the severity of the injury reaching towards the back of the eye, an irregular response in the pupils to light stimulus, the jelly-like substance inside the eye (vitreous) escaping through the wound, the length of the wound, blood leakage inside the eye (vitreous hemorrhage), blood in the anterior chamber of the eye (hyphema), eye inflammation (endophthalmitis), and the detachment of the light-sensitive tissue at the back of the eye (retinal detachment).
To help predict the vision outcome after a severe eye injury, doctors can use a tool called the Ocular Trauma Score. This score was developed in 2002 to estimate the likely functional outcome for patients who have suffered a serious eye injury.
Possible Complications When Diagnosed with Globe Rupture
If someone’s eye ruptures, it can cause a range of problems, including lifelong blindness, severe eye inflammation and chronic pain. Some complications may not appear until later, such as membranes forming in the eye, the retina pulling away from its normal position, or the eye shrinking and losing function. A particularly harmful complication is sympathetic ophthalmia, where both eyes become inflamed due to the body’s immune system reacting to the injured eye. To reduce the risk of this happening, some experts suggest removing the injured eye within two weeks if there’s a high chance of poor vision.
Another issue can happen if something gets lodged in the eye. If this object is made of copper, it can lead to what’s known as chalcosis which may cause conditions such as cloudy lenses, chronic eye inflammation, blurred vision due to clouding of the vitreous humor, and copper deposits in the central part of the retina. If the object is made of iron, it may result in siderosis bulbi, causing retinal damage, eye color changes, loss of ability to adjust the eye to different light levels, night blindness and vision loss.
Common complications:
- Permanent blindness
- Severe eye inflammation (endophthalmitis)
- Chronic pain
- Retina Detachment
- Eye Shrinking (phthisis bulbi)
- Bilateral eye inflammation (sympathetic ophthalmia)
- Chalcosis (Copper toxicity)
- Siderosis bulbi (Iron toxicity)
Preventing Globe Rupture
Patients need to be well-informed about the importance of protecting their eyes and steering clear of harmful habits that can hurt their eyes. Patients should also be aware that they are at a higher risk of an eye injury known as a ‘globe rupture’, especially after a type of eye surgery called a ‘penetrating keratoplasty’. For this reason, it’s crucial that patients avoid any strenuous activities after having such a surgery.