What is Hollenhorst Plaque?
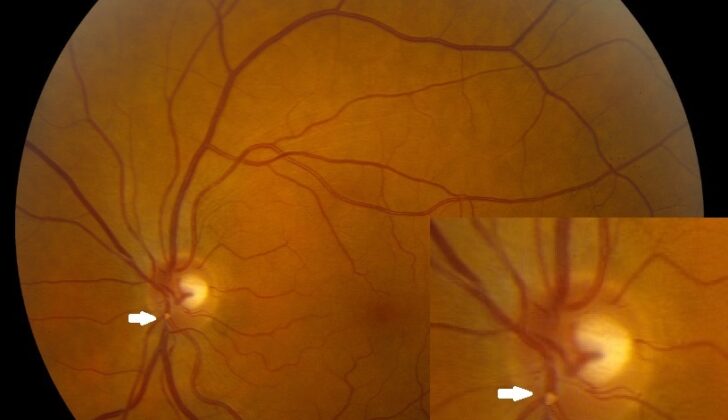
Stroke is the third most common cause of death in the U.S. Most strokes, about 80%, happen because a blood vessel is blocked due to things like fatty deposits or blood clots. Hollenhorst plaque was identified in 1961 by Dr. Robert Hollenhorst as small clots caused by fatty, cholesterol plaques. These can be seen in the small blood vessels of the retina, the part of the eye that senses light and sends images to the brain. They are yellow, shiny, and usually found at the point where a blood vessel splits into two. Hollenhorst plaque is often the primary cause of ocular ischemic syndrome, which is when the eyes don’t get enough blood, usually because of a blockage in an eye artery.
In 1927, T. Harrison Butler spoke about a bright retinal blood clot in a blood vessel in the lower part of the eye. This clot was further described by Hollenhorst, Witmer, and Schmid in 1958. Hollenhorst suggested that cholesterol ester, a type of fat found in the blood, was the main component of the clot. He also proposed that the appearance of these clots could predict future strokes in the same side as the clot in patients with symptomatic carotid disease, a condition where the main blood vessels to the brain get narrow or blocked. He also noted that the clot could move when pressure was applied to the eye. He detailed these bright, orange-looking clots in a paper in 1961, noting they were found in 11% of patients with carotid disease and 4% with vertebrobasilar diseases, a type of stroke caused by poor blood flow to the back of the brain. These clots usually don’t block blood vessels completely, instead often moving to smaller blood vessels and eventually breaking up.
Hollenhorst and Jack Whisnant were able to reproduce these retinal clots in animals by injecting cholesterol crystals and fatty material into their carotid arteries. This was later confirmed in 1963 from a patient who had similar looking retinal clots and who died after surgery to remove fatty deposits from their carotid artery.
What Causes Hollenhorst Plaque?
Hollenhorst plaques (HPs) typically develop from carotid arteries or the aorta, and this is usually due to atherosclerosis (a disease where plaque builds up inside your arteries). Eye care professionals initially thought these plaques came from the narrowed (stenosed) carotid artery on the same side of the body (ipsilateral). This belief was based on the direct anatomical path from the internal carotid artery (ICA) to the artery that supplies the retina (central retinal artery, or CRA).
Here’s why: the ophthalmic artery, which is the first branch of the ICA, leads into the CRA. This means that the ICA is directly connected to the CRA, providing a potential pathway for the plaques to reach the retina.
Risk Factors and Frequency for Hollenhorst Plaque
According to the Blue Mountains Eye study, 1.4% of people over 49 years old have retinal emboli, a condition of the eyes. This condition becomes more common as people get older. It’s been found that retinal emboli are more common in men than in women. About 80% of retinal emboli are made up of HPs, and around 10% of carotid emboli reach the blood vessels in the eyes.
In the Beaver Dam Eye Study, which included almost 5000 patients, 1.3% had HPs and a 5-year occurrence rate was found to be 0.9%. Moreover, in another study involving 130 consecutive patients diagnosed with HP and either central or branch RAO, the average age of the patients was found to be 68, with 61% showing symptoms.
- The rate of retinal emboli without symptoms is 1.4%.
- Cholesterol emboli affect men more than women (2.2% vs 0.8%).
- About 80% of all retinal emboli are cholesterol-type.
- There have been observed connections with high blood pressure (odds ratio [OR], -2.2), vascular disease (OR, -2.4), history of vascular surgery (OR, -3.5), and current or past smoking (OR, -2.2 and OR, -2.6 respectively).
Signs and Symptoms of Hollenhorst Plaque
Hollenhorst plaques (HP) are signals of previous embolic incidents but they are not reliable in predicting future ones. These plaques can sometimes cause a retinal artery occlusion (RAO), but not always. The presence of these plaques without symptoms can indicate more about the overall health of the person, rather than just their eye health. HPs are typically found unexpectedly during a routine eye examination. These plaques might move and wouldn’t be seen in later eye tests.
HP is a factor in diagnosing RAO. For a plaque to cause an RAO, it must completely block the blood vessel. RAO can happen in the main retinal artery (central retinal artery occlusion or CRAO) or one of its branches (branch retinal artery occlusion or BRAO). However, HP is only a possible cause of a CRAO/BRAO and doesn’t always mean there’s an occlusion.
As per different diagnosis, there are other kinds of emboli that can block the blood vessels. There are also other causes of RAO not related to emboli, like low blood pressure at night and temporary vasospasm. HPs, just like other types of retinal emboli, can dislodge and move to a smaller vessel before getting stuck again, or they can dissolve altogether. If there’s an HP, it confirms a diagnosis but its absence does not completely rule out the possibility of embolic blockage.
If an RAO happens, a sudden and painless vision loss is the most common symptom. The back of the eye (fundus) will show signs of low oxygen supply including, whitening around the blocked vessel. The macula area (part of the retina) will remain “cherry-red” due to an additional blood supply. If the plaque only partly blocks the blood vessel, blood can still flow and not cause any damage. A person can experience more than one temporary RAO in the same eye.
Testing for Hollenhorst Plaque
A variety of tests can be used to evaluate hollow pearls (HPs), a medical condition:
Listening to the carotid (a major neck artery) for abnormal sounds (or bruits) is one way. This is done using a stethoscope and the process is known as auscultation.
Checking the patient’s blood pressure is another important step, this can help identify if the patient has abnormally high or low blood pressure which can cause problems.
Carrying out an electrocardiogram (ECG) can help to identify any irregularities in the heart’s rhythm, such as atrial fibrillation (an abnormal heart rhythm characterized by rapid and irregular beating).
A carotid duplex study is another form of testing to evaluate the degree of narrowing in the carotid arteries. A significant narrowing usually means a reduction in diameter of 80% to 99%, a peak blood flow speed over 125cm/sec, and an end-speed over 140cm/sec. In one study, fewer than one in three patients had narrowing of more than 30%, and only 8% had narrowing over 60%.
Echocardiography (ECHO), which is an ultrasound test of the heart, can help to identify the sources of potential blood clots in the heart that can cause hollow pearls.
Either a CT scan or an MRI of the carotid arteries (often referred to as 4-vessel carotid angiography) can be used to evaluate for narrowing, tearing or abnormal development of the carotid arteries. CT angiography has an 85% success rate for spotting these problems and specific accuracy rate of 93%.
Blood tests can be done to rule out blood clotting disorders.
Fluorescein angiography is a specific eye test using a special dye and camera to look at blood flow in the retina and choroid, the two blood vessel layers in the back of the eye. It can help to identify loss of blood flow, damage to blood vessels due to chronic low blood supply, swelling in the macula (central retina), and leakage from the optic disc (nerve connecting the eye to the brain) and blood vessels in the eye.
Visual-evoked potentials (VEP), electroretinography (ERG), and ophthalmological tonometry are rarely applied. ERG measures the electrical responses of various cell types in the retina, including the photoreceptors (rods and cones), inner retinal cells, and the ganglion cells.
Optical coherence tomography (OCT) can measure retina thickness and can identify damage due to hollow pearls. Reduced visibility of the blood vessels in the central retina and reduced blood vessels in all retinal layers after treatment for HPs were seen during the OCT exam.
Finally, imaging techniques like B-scan ultrasonography or CT scan are performed to rule out the presence of mass lesions or tumors that could be causing pressure effects.
Treatment Options for Hollenhorst Plaque
If a blood clot forms in your eye, immediate massage may help to remove the blockage. However, the retina, which is the part of your eye that senses light, can be permanently damaged after just four hours of blockage.
A surgical procedure to remove the clot was first tried in 1990 and was successful in allowing blood flow to return and improving sight in the majority of patients in one study.
Further treatment depends upon how blocked your arteries are. For patients whose arteries are less than 50% blocked, doctors usually recommend antiplatelet therapy. This is a type of medication that prevents your blood from clotting, including Aspirin and Clopidogrel. Following this plan can lower your stroke rate by almost 50% over the next five years. A trial showed that using cholesterol-lowering medication also reduces the risk of both stroke and heart disease.
Patients with arteries more than 70% blocked may need surgery. The options include removing the blockage or using a balloon to open up the blood vessel. Both options are safe and effective, but removing the blockage can increase your chance of heart attack, while opening up the blood vessel can increase your chance of a stroke. Both options have a similar risk for a stroke leading to death or disability.
The North American Symptomatic Carotid Endarterectomy Trial showed it is very useful to do surgery on patients with a blockage of 70% to 99%. Surgery dramatically lowered the risk of stroke within two years compared to medication alone (from 26% to 9%). These findings were also seen among patients in a European trial. A study involving a large number of patients with moderate to severe blockages but low risk of complications from surgery showed that removing the blockage is better than medical therapy alone.
For patients with moderate blockages of 50% to 69%, the benefits of surgery were much less prominent.
A trial involving people with 60% blockages showed a 53% and 46% risk reduction when the blockage was removed. Doctors often recommend removing the blockage when the risks associated with surgery, such as stroke or heart attack, are very low.
If a clot completely blocks a vessel in your eye, causing a retinal artery occlusion (a blockage in the blood vessels of your eye), you may not need treatment if an HP which is a type of blood clot does not cause a complete blockage. All patients with eye blood clots should be referred to their primary care provider for a study of the blood flow in both carotid arteries (the major blood vessels in the neck that supply blood to the brain). Approaches to managing this issue include educating patients on the underlying causes, making lifestyle changes (treating diabetes, high blood pressure, and high cholesterol, improving sedentary lifestyles and obesity, and quitting smoking), and taking aspirin to treat arteriosclerosis, a disease where plaque builds up inside your arteries.
What else can Hollenhorst Plaque be?
There are several different types of emboli, or blockages, that can occur in the retina:
- Calcific emboli: These appear whitish, usually affect the central retinal artery, don’t dissolve, and often come from calcification in the cardiac valves or aorta.
- Fibrinoplatelet emboli: These appear as a dull white within the retinal arteriole and are often a result of a carotid thrombus (clot in the carotid artery).
- Talc emboli: These are often seen in patients who use intravenous drugs and/or cocaine, are usually relatively small and appear around the fovea, the central part of the retina.
- Metastatic tumor cells: These emboli are actually cancer cells that have traveled to the retina from elsewhere in the body.
- Septic emboli: These typically follow bacterial endocarditis, an infection of the inner layer of the heart.
- Fat emboli: These often occur when long bones are fractured and are usually accompanied by scattered retinal microinfarcts (small areas of cell death) and hemorrhages (bleeding).
- Amniotic fluid emboli: These are a rare complication of childbirth where fragments of amniotic fluid, which surrounds an unborn baby in the womb, enter the mother’s bloodstream and block blood vessels.
- Air emboli: These occur when air bubbles enter the bloodstream and block blood vessels. This is often a complication of certain surgeries, scuba diving accidents, or lung injury.
What to expect with Hollenhorst Plaque
A disease called atheromatous, which affects the ICA (a major artery in the neck that supplies blood to the brain), can be linked with HPs (small clumps of cholesterol in the blood vessels in the eyes). This is usually a sign of potential stroke risk. Narrowing of this artery, known as carotid stenosis, increases stroke risk by 1.18 times for every 10% increase in narrowing. If the artery is less than 80% blocked, the risk of stroke is less than 1% per year. However, when the artery is more than 90% blocked, the risk of stroke goes up to 4.8% per year.
Interestingly, about 75% of HPs show no symptoms and are not a strong predictor of future blockages in the blood vessels. However, 25% of such cases have more than 40% carotid stenosis – a significant narrowing of the carotid artery. Patients who have symptoms are more likely to have narrowing of more than 69% in the carotid artery compared to those without symptoms (25% vs 9.2%).
It was also observed that patients with cholesterol plaques in the retina had a higher incidence of stroke compared to those without (8.5% vs 0.8%). Cholesterol blockages carry a 15% risk of death at 1 year, which increases to 29% at 3 years, and jumps to 54% at 7 years. These patients have increased chances of dying due to stroke.
Even if the cholesterol embolism in the retina shows no symptoms, it still poses a risk for cerebral infarction – a type of stroke caused by blocked blood flow to the brain. In an analysis of 1343 patients with asymptomatic cholesterol emboli, 17.8% had a history of either stroke or TIAs – transient ischemic attacks that can be a warning sign of a future stroke. Twelve percent of these patients had a stroke, TIA, or died during their follow-up, suggesting that these patients should be referred to a medical professional to manage similar cardiovascular risk factors.
There are no current guidelines recommending carotid endarterectomy (CEA – a surgical procedure to remove blockages from the carotid arteries and restore blood flow to the brain) for patients with just HP or retinal emboli. In a study comparing different eye-related conditions, only patients with CRAO (a blockage in the main artery in the retina resulting in vision loss) and BRAO (a blockage in a smaller branch of the retinal artery) had significantly higher rates of death and cerebral vascular events.
Possible Complications When Diagnosed with Hollenhorst Plaque
Possible complications of HPs include:
- Blockage of the main artery in the eye (Central retinal artery occlusion)
- Blocking of the smaller branch arteries in the eye (Branch retinal artery occlusion)
- Lack of blood supply to the brain, also known as ischemic strokes
Preventing Hollenhorst Plaque
Preventing vascular health problems, such as cholesterol plaques blocking blood vessels (known as HPs), is a process that heavily relies on education and deterrence. This involves understanding risk factors and learning ways to lower risks.
Healthcare providers aim to identify and manage risk factors associated with cholesterol plaque formation. These could include high blood pressure (hypertension) and the buildup of fats, cholesterol, and other substances on artery walls (atherosclerosis). They also recommend lifestyle changes – such as a heart-healthy diet, regular exercise, and quitting smoking – to help prevent cholesterol plaques and related vascular problems.
Equally important is patient education. Understanding the significance of these cholesterol plaques, the potential risks they pose and the preventive methods available allows individuals to be proactive about their own health. This could involve recognizing early warning signs, attending regular eye check-ups (since plaques can also affect the eyes), and sticking to prescribed medications. Being aware and actively involved in managing their condition enables patients to detect problems at an earlier stage, allowing for quicker intervention and lessening the possible impact of cholesterol plaques on their overall health.
In summary, a combination of preventive strategies and patient education creates a supportive environment for patients to make informed decisions and work with their doctors in maintaining overall vascular health.