What is Hyperopia?
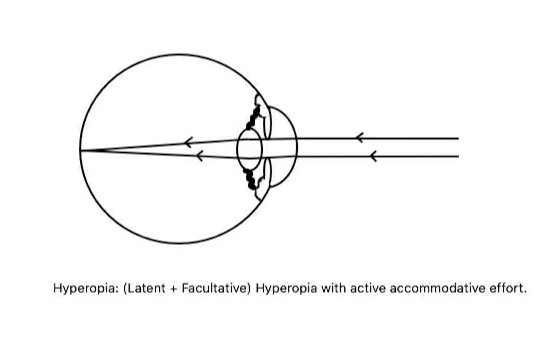
Hyperopia, often known as “farsightedness,” is the most common vision issue in children. This condition happens when the eye focuses light rays from distant objects behind the retina, the part of the eye that receives light, instead of directly onto it, when the eye is in a relaxed state. Because of this, the eyes have to work harder to refocus the light, especially in younger people.
When babies are born, they are often farsighted. As they age, their eyes naturally adjust to focus correctly, which brings their vision to normal, or they might even become shortsighted. It’s also worth noting that genetics play an important role in farsightedness, meaning that if it’s common in your family, there’s a likelihood it’ll be passed on to future generations. If farsightedness is diagnosed but not treated, it can lead to further problems such as lazy eye (amblyopia) and misalignment of the eyes (tropia).
What Causes Hyperopia?
Hyperopia, also known as farsightedness, is generally classified into several types based on different factors:
1. Axial hyperopia (most common – simple hyperopia): This happens when the eyeball is shorter than usual due to genetic factors. Swelling of the retina can also contribute to this condition. A reduction of 1 mm in eyeball’s length can increase farsightedness by 3 units (called diopters).
2. Curvature hyperopia: This is caused by the cornea (the clear front surface of the eye) or the inner lens becoming flatter. An increase of 1 mm in the curvature radius can lead to 6 diopters of hyperopia.
3. Index hyperopia: This type of hyperopia is linked to changes in how the natural lens of eye bends light. Such changes often happen as a person gets older or if they have diabetes.
4. Positional hyperopia, or absence of the lens (aphakia) or eye disease: This happens when the lens is not in the right place, when it’s missing (congenitally or from surgery), or when the lens is replaced with an artificial lens forming a lens-free zone. Blunt or penetrating trauma and surgical removal of the lens are not uncommon causes of hyperopia.
There are also certain eye conditions, such as nanophthalmos (small eye), microphthalmos (underdeveloped eye), and aniridia (absence of the iris), which might cause hyperopia.
Currently, no unanimous root cause of hyperopia has been identified. However, it’s thought to be a mix of genetic features, environmental factors, and age-related issues. Some identified causes of hyperopia include genetic factors (16p11.2 microdeletion and Myelin regulatory factor gene mutation), family history of squint, maternal smoking during pregnancy, cortical cataract (related to index hyperopia), aphakia (congenitally or acquired), and high blood sugar levels.
Interestingly, diabetes and sudden control of high blood sugar levels in diabetics can lead to farsightedness. It has also been seen in astronauts due to retina and optic nerve swelling after long space missions. Other conditions and syndromes related to hyperopia include peripapillary pachychoroid syndrome, Heimler syndrome, Kenny syndrome, loss of focusing ability due to complete nerve paralysis or paralysis caused by eye drops or lorazepam, post silicone oil injection in eyes with natural or artificial lenses, Loeys-Dietz syndrome, Larsen syndrome, Leber congenital amaurosis, X-linked retinoschisis, and senile retinoschisis.
Risk Factors and Frequency for Hyperopia
Axial hyperopia is a common condition that typically starts at birth. Moderately intense hyperopia, which is equal to or greater than +2 diopters, affects 13.2% of 6-year-olds and 5.0% of 12-year-olds. This condition is more prevalent in white individuals. With an intensity of hyperopia equal to or more than +4 diopters, about 3.2% of people have it on the worse eye, and in 64.4% of cases, it affects both eyes.
- In the United States, non-Hispanic and Hispanic White races have a higher risk of hyperopia in ages 6-72 months.
- In the age groups of 15 years or less and those 30 years and above, hyperopia is more prevalent in females.
- A review of refractive errors showed the general prevalence of hyperopia being 4%, which is less than myopia. It is more common in school-going boys than girls.
- In the United States, among people 20 years and older, hyperopia is the least common refractive error but becomes the most common refractive error paired with astigmatism in people aged 60 years and above.
- For Polish immigrants in Chicago, hyperopia is a more common refractive error overall, and especially so in those over the age of 45 years.
In Cameroon, children aged 6 to 15 years typically have hyperopia as the most common refractive error. There’s no association between hyperopia and posterior subcapsular cataracts, but it is related to nuclear and cortical cataracts. A UK study found that the intelligence quotients of people with hyperopia are lower than those with myopia. People living in rural areas are more likely to have hyperopia compared to those in urban areas. Strabismus, a condition characterized by the lack of coordinated eye movements, develops in 20% of babies with hyperopia. Families with a history of accommodative esotropia and hyperopia are also more likely to have members with hyperopia.
Signs and Symptoms of Hyperopia
Hyperopia, or far-sightedness, can present in a variety of ways depending on factors like the age of the patient and the extent of the hyperopia. Sometimes there may be no symptoms at all, while other times a range of symptoms may be present. In some cases, the patient’s own eye muscle tone and effort can overcome a certain degree of hyperopia without causing any problems. However, in other instances, patients may experience several different symptoms.
The severity of symptoms can differ from person to person based on factors such as their age and the effort they can put into accommodation or adjusting their vision.
Here’s a list of potential symptoms:
- Eye deviation (observed by parents): In young children with hyperopia, parents may notice deviation or misalignment in one or both eyes. The most common type is an inward deviation (esotropia).
- Asthenopia: This is a condition in which patients experience eye fatigue, resulting in headaches and sometimes associated with light sensitivity and watering eyes. It usually worsens after close and prolonged visual activity.
- Blurred vision: Patients may experience blurred vision, especially for close objects. The level of blur increases as objects get closer. Blurred vision might also be associated with eye fatigue.
- Sudden blurring of vision (intermittent): Some teenagers with uncorrected hyperopia may experience brief episodes of blurry vision, often referred to as pseudomyopia. This usually occurs due to a temporary, involuntary contraction of the eye muscles during prolonged close-up tasks (like reading).
- Recurrent Internal/External Hordeolum or Conjunctivitis: Some hyperopia patients may experience recurring inflammation of the eyelid or conjunctiva. This could be attributed to the frequent rubbing of the eyes with unclean hands.
- A sensation of Crossed Eye: Some patients may feel like their eyes are crossing each other due to the continuous effort to focus clearly, especially in close-up tasks.
- Premature Presbyopia: Some hyperopic patients may experience an early onset of presbyopia (inability to focus on close objects) which is typically noticed as we age. This can occur earlier (before the 40s) in far-sighted individuals compared to those with normal vision.
Testing for Hyperopia
If your doctor suspects you might have hyperopia (farsightedness), they will likely conduct a comprehensive eye exam to confirm this.
Part of this exam will be a test of your visual acuity – how well you can see. This can be affected by your age, the flexibility of your eye’s crystalline lens, and the health of the back part of your eye. Children, who are very good at focusing, may not always show signs of hyperopia. However, high levels of hyperopia can affect far vision, which can’t be corrected through focusing alone. If hyperopia goes untreated in children, it can drastically reduce vision over time. This condition can also make near vision poor, especially for older individuals where the ability to focus is partially or fully lost. The ability to see up close can get gradually worse with age.
Your doctor may also do a diffuse light examination. This involves looking at the cornea (the clear, outermost layer of the eye) and the eyeball, which can appear smaller in people with high hyperopia and in cases where it affects only one eye. In some instances, it can make it seem like the eye has sunk into its socket. The doctor will also evaluate the anterior chamber (the front part of the eye) and the angle of this chamber, which could appear smaller if someone has hyperopia. An eye exam may be needed to rule out a narrow-angle which is a type of glaucoma. Sometimes, older individuals and people living with diabetes may also have cataracts.
During fundoscopy (an examination of the back of the eye), the doctor might see a small optic disc (the area where the optic nerve enters the eye) with a very small depression. The edges of the disc may become blurred due to the overcrowding of blood vessels. This can sometimes lead to “pseudopapillitis” or “pseudo-papilledema.” In addition, they might notice crowding of the nerve fiber layer in the eye and an increased reflex of the retina, which is a condition known as “shot-silk appearance.”
Another part of the eye exam can involve checking for strabismus (eye alignment problems), which may be present in children who have had uncorrected hyperopia for a long time. Strabismus can be latent (hidden unless certain conditions bring it out) or manifest (where the eye deviates noticeably). However, eye movement is usually normal. A cover-uncover test can reveal latent strabismus, primarily in children and young people. In cases of manifest strabismus, a Hirschberg corneal reflex test and a prism bar can be used to determine the degree of deviation from normal eye alignment.
Retinoscopy, or using a tool called a retinoscope to reflect light off the back of the eye, is still important when examining young or bed-ridden patients even though most exams these days are automated. If a young child exhibits signs of a vision error, doctors often use cycloplegic retinoscopy from a meter away as standard practice. Cycloplegia is a state in which the muscles controlling the shape of the lens are temporarily paralyzed, stopping accommodation and revealing the actual status of the eyesight. Then, using a streak retinoscope and different powered-spherical lenses, they try to find the point of neutralization, or when the eye’s reflex illumination seems steady when the light beam is swung from side to side and up and down.
The existing refractive error, or how much the eye’s ability to bend light is off, is determined by subtracting the value of the distance from the patient in meters and the cycloplegic agent’s tonus allowance from the retinoscopy results. If both the horizontal and vertical refractive errors are equal after the deductions, then that indicates the spherical refractive power of the eye. If they are unequal, then the difference in power denotes the astigmatic power (blurriness or distortion at all distances due to irregular curvature of the lens) in the other axis.
Treatment Options for Hyperopia
The objective of treating hyperopia, or farsightedness, is to improve vision through proper corrective lenses, prevent lazy eye formation (amblyopia), avoid the development of crossed eyes (strabismus), and prevent recurring eyelid infections and eye inflammation (conjunctivitis).
To address vision problems, specific lenses, known as biconvex lenses, are recommended. These lenses help converge light rays on the back part of your eye where vision is processed (the neurosensory retina). Optometrists are guided by a set of principles when prescribing these corrective lenses. For example, they prescribe full corrective lenses to young children, gradually reducing this as the children get older.
The guidance from the American Academy of Ophthalmology (AAO) for children’s glasses prescription based on the amount of their farsightedness considers their age and whether the amount of farsightedness is similar in both eyes or not, and if any crossed eyes are present. Glasses or contact lenses can be used for correcting vision. Contact lenses are typically recommended when the amount of farsightedness is significantly different between the two eyes.
Surgery is also an option for treating hyperopia. Prior to surgery, several tests must be carried out to ensure patient safety and operation success. These tests involve examination of eye health, eye pressure, retinal health and assessing the patient’s vision. There are several types of surgeries available to treat hyperopia, from incisional procedures to laser-based treatments, each with their own set of strengths and potential complications.
After surgery, patients will likely need to wear an eye patch or dark glasses and apply certain medications. Some cases may also require special types of lasers or techniques. The doctor would talk through the entire process, possible outcomes, and any potential side effects with the patient beforehand.
When it comes to treating hyperopia-related angle-closure disease, a potential risk for those with farsightedness, laser peripheral iridotomy (a procedure to make a small hole in the outer edge of your iris) has proved an effective solution. Eye surgeries that remove part or the entire lens, such as cataract surgery or clear lens extraction, have also shown promising results.
Regardless of the treatment option pursued, regular follow-up checks are essential to monitor the child’s vision and adjust treatment as needed.
What else can Hyperopia be?
If an individual is suffering from hyperopia (far-sightedness), a doctor may suggest the possibility of the following health conditions:
- Nanophthalmos – A situation where the eye is smaller in size, but its structure appears normal.
- Microphthalmos – In this condition, the eye is not only smaller in size, but its structure is also abnormal. This might be related to other health conditions.
- Posterior microphthalmos – This is a type of Microphthalmos where only the back part of the eye is involved. The front part of the eye remains of normal size.
- Micro-cornea, enophthalmos – These conditions relate to a smaller cornea and a sunken eye.
- Partial ptosis – Here, there appears to be a smaller eyeball due to drooping of the eye.
- Papilledema – Swelling of the optic nerve in the eye.
- Retinal edema or serous or exudative elevation of the retina – Conditions that include swelling or fluid build-up in the retina.
- Orbital tumors – This occurs when tumors in the eye socket push forward the back part of the eyeball.
- Hypoglycemia – Low blood sugar. This particular condition might not seem related to the eyes, but it can cause vision problems similar to hyperopia.
- Presbyopia – This is a condition common in older adults where the flexibility of the eye’s lens decreases, causing difficulty in seeing up close.
What to expect with Hyperopia
Good prognosis factors:
If hyperopia (more commonly known as farsightedness) is diagnosed and treated early, particularly in preschool aged children, the prospects for recovery are quite high. An essential part of the process is to initially dilate the pupils using eye drops for what is called a cycloplegic refraction test, followed by a standard eye exam.
Additionally, suspected amblyopia (also known as lazy eye), if correctly managed, can have a positive outcome. However, if treatment for this condition is delayed, it can lead to permanent vision decline.
Patients who receive preoperative preparation and timely medical interventions also usually have a good outlook.
Bad prognosis factors:
However, certain factors could potentially make the prognosis worse. These include:
– Other eye abnormalities
– Performing surgery in cases where the eye prescription is not stable
– Co-existing systemic syndromes (a combination of medical conditions in various parts of the body)
– Having a family history of squint (crossed or turned eye) and lazy eye.
Possible Complications When Diagnosed with Hyperopia
People who are hyperopic, or long-sighted, have several potential eye health risks if their condition isn’t timely corrected. Amblyopia, sometimes called lazy eye, is where one or both eyes do not develop clear sight. If left untreated, it might lead to stimulus deprivation or anisometropic amblyopia, which means one eye sees more clearly than the other. To treat this, orthoptic exercises and appropriate vision correction are necessary.
If the eye is not corrected in time, it can lead to squinting, also known as convergent strabismus, which is fairly common in developing children. Over time, the squinted eye gets less and less visual stimulation.
There’s also the risk of developing closed-angle disease, where the drainage canals in your eyes get blocked, leading to increased eye pressure. Again, not correcting hyperopia in time could trigger this condition.
Furthermore, hyperopia is a risk factor for Anterior Ischemic Optic Neuropathy (AION), it is a condition that happens when blood flow to the optic nerve is reduced or blocked.
Potential Complications:
- Amblyopia if not timely corrected
- Convergent strabismus in developing children
- Increased risk of closed-angle disease
- Higher likelihood of developing AION
In some people, branch retinal vein occlusion, where the smaller branches of the major retinal vein become blocked, might be more likely to happen. Also, age-related macular degeneration, a condition that blurs your sharp, central vision, and central serous chorioretinopathy, where fluid builds up under the retina and distorts vision, could be associated with hyperopia.
Further Potential Complications:
- Branch retinal vein occlusion more likely
- Possible association with age-related macular degeneration
- Risk of developing central serous chorioretinopathy
There are other common features associated with hyperopia, like serous retinal detachment, pre-retinal folds with macular cysts, macular folds, and thickening of the fovea (the center of the retina) and retinal pigment epithelium.
Additional Conditions:
- Serous retinal detachment, pre-retinal folds with macular cysts
- Macular folds
- Thickening of the fovea and retinal pigment epithelium
Recovery from Hyperopia
Treatment for hyperopia, or long-sightedness, often involves glasses or contact lenses, which are both effective and budget-friendly options. Wearing glasses consistently, as well as carrying out specific eye exercises known as amblyopia therapy, is a key way to manage a related condition called refractive amblyopia as the eyes develop. This approach can also help prevent misalignment of the eyes, a condition known as strabismus.
Keratorefractive surgeries, which reshape the eye’s cornea to improve vision, are another important option for treating hyperopia. These surgical procedures usually use lasers or intense heat from radio waves. After such surgery, you might have to:
* Wear dark glasses (after LASIK surgery) or use eye patches (after CK surgery).
* Apply eye drops containing broad-spectrum antibiotics for 5 to 7 days or more if necessary, plus use artificial tears.
* Be careful not to rub your eyes immediately after the operation.
* It’s possible that you may need to use a medicated eye drop called cyclosporine A to help with dry eyes after surgery.
* Regular follow-up appointments will be necessary to check your eye prescription, how your flap (surgically created thin layer of the cornea) is healing, and to catch any complications early.
Preventing Hyperopia
Teaching patients and their parents about health is essential to prevent health issues from worsening. This includes explaining to expecting mothers that smoking while pregnant can increase the chances of their child having hyperopia, or long-sightedness, which makes it difficult to see things up close.
It’s also important to provide education and counselling to parents. This doesn’t just help in detecting and treating hyperopia early, but also prevents the development of strabismus, where the eyes don’t line up in the same direction, and amblyopia, commonly known as lazy eye.
Additionally, parents need to take an active role in treating amblyopia. This involves making sure the child wears their glasses as necessary, doing eye patching therapy, and giving eye exercises, which can help improve the eye’s vision.
Lastly, it’s critical to schedule regular check-ups that includes an eye examination and refraction testing, which checks for changes in the eye’s need for glasses. These regular tests help identify any changes in the child’s eyesight and respond to those changes promptly.