What is Interferon-Induced Retinopathy?
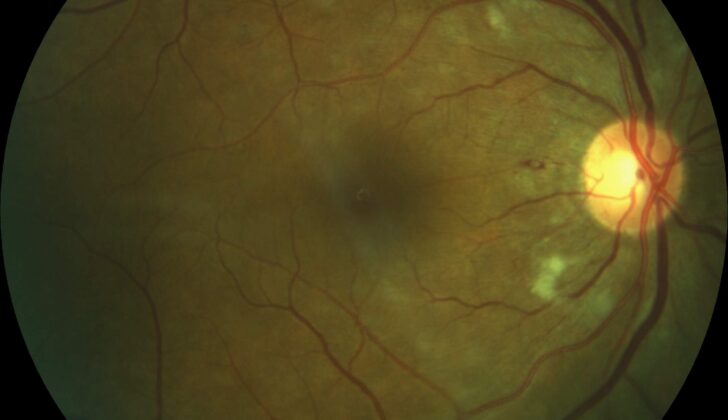
Interferons, discovered in 1957 by Issacs and Lindenmann when they were studying how viruses interact with each other, have become vital in the treatment of diseases like hepatitis C, various forms of cancer, and immune system disorders like multiple sclerosis. Even though interferon therapy can be effective, it can sometimes have negative effects on different body systems. One major side effect is ‘retinopathy’ – a disease that can damage our eyes. This can be detected by indicators like reddish-colored, flame-shaped spots of blood in the eye, ‘cotton wool’ spots (tiny, fluffy white spots on the retina, the layer at the back of the eyeball), and a condition called macular edema (swellings or thickening in the central part of the retina), found during a comprehensive eye check-up. Though interferon-related retinopathy might cause temporary and symptom-less effects, it could potentially lead to vision loss, emphasizing the need for prevention and early detection.
In 1986, the U.S. Food and Drug Administration (FDA) approved two kinds of interferons (α-2a and α-2b types) for treating a type of blood cancer, known as hairy cell leukemia. Since then, the uses of interferons have expanded to include a range of health conditions. But, along with their potential benefits, these interferons could cause harmful effects that impact various body systems such as brain, gut, glands, heart, kidneys, and the skeletal system. The first record of negative eye effects linked to interferon treatment came from Ikebe and his team in 1990. They documented a 39-year-old patient who experienced bleeding in the retina and cotton wool spots after receiving interferon via injection.
Deciding whether to continue interferon treatment or reduce the dose can be a tough call due to the range of potential side effects that could occur. These effects might be a result of blockages in the tiny blood vessels of the eye or possibly due to other issues where tissues of the body do not receive enough oxygen because of immune complex deposition (a condition where the immune system forms complexes that can cause inflammation and damage). Less common, but potentially serious side effects, such as blockages in the eye’s main blood vessels and optic neuritis (an inflammation that damages the nerve connecting the eye to the brain), could also occur.
What Causes Interferon-Induced Retinopathy?
Interferons are a group of proteins that our cells produce when they’re trying to fight off viruses. Their main job is to boost our body’s natural defense mechanisms against viruses. But they can also help fight bacterial and parasitic infections, control cell growth, and influence the development of cells.
Mainly, there are three types of interferons: interferon-α, interferon-β, and interferon-γ. They activate cells called natural killer cells and macrophages, which play a big part in fighting off infections. They also help our body’s defenses by increasing the display of what are called “major histocompatibility complex antigens.” Essentially, these are signals that help immune cells recognize infected or sick cells.
After they’re released, interferons connect with receptors on nearby cells. This triggers those cells to produce antiviral proteins and even more interferons to help stop the virus from spreading.
Risk Factors and Frequency for Interferon-Induced Retinopathy
Studies show that retinopathy (a condition that affects the retina of the eye) caused by the use of interferon, a type of medication, affects between 18% to 86% of people. The chance of getting this condition is particularly high in some areas of Japan, where it affects between 50% to 86% of people. The rate is usually higher among older adults and people with health conditions like high blood pressure and diabetes. How likely you are to get retinopathy also appears to be connected to the amount of interferon you take.
This type of retinopathy can develop anywhere from 2 to 28 weeks after starting interferon treatment, but it usually appears within the first 3 months. People who don’t respond to interferon treatment seem to be more likely to develop retinopathy. It’s important to note that retinopathy was found to occur more often in studies where eye exams were done more regularly.
- The chance of getting interferon-induced retinopathy ranges from 18% to 86%.
- It’s more common in some parts of Japan, affecting 50% to 86% of people.
- Odds are higher in older adults and those with conditions like high blood pressure and diabetes.
- The likelihood is also tied to how much interferon you’re taking.
- This condition typically develops within the first 3 months of treatment.
- Those who don’t respond to interferon treatment have a higher chance of getting retinopathy.
While interferon-induced retinopathy usually goes away on its own over time, spacing out eye exams too far apart could result in some cases being missed. This is why studies that don’t do eye exams as frequently, especially in the first 6 months of treatment, might report a lower rate of retinopathy. Similarly, if eye exams are only done after symptoms appear, the number of retinopathy cases could be underreported. It’s still unclear why some people are more likely to get retinopathy from interferon and also why some people have mild symptoms while others have severe vision loss.
Signs and Symptoms of Interferon-Induced Retinopathy
Interferon-associated retinopathy, a condition affecting the eyes, can cause various symptoms. Some people may experience reduced visual acuity, floaters, fluctuations in vision, and the perception of dark spots in their vision. However, many people with the condition remain asymptomatic, meaning they don’t have any noticeable symptoms. Specific changes in the eye, such as retinal hemorrhages (bleeding from the tiny blood vessels in the retina) and cotton wool spots (swellings on the retina), are typically observed around the optic disc, which is the area where the optic nerve connects to the retina.
Hyperemia of the optic disc (an increase in blood flow) and macular edema (swelling in a part of the retina called the macula) may also be seen, and these symptoms can affect one or both eyes. The retinal hemorrhages usually look like flame-shaped reddish streaks that may have a white center. If there are retinal microaneurysms (tiny bulges in the blood vessels of the retina), it’s necessary to rule out diabetes, which can cause these changes, too. Oftentimes, these patients may also have diabetes or hypertension in conjunction with the retinopathy.
Besides these, several other eye-related complications can arise, although they are less common. They include:
- Central retinal artery occlusion
- Central retinal vein occlusion
- Combined central retinal artery and vein occlusion
- Non-arteritis anterior ischemic optic neuropathy
- Optic neuritis
- Optic disc edema
- Vitreous hemorrhage
- Pe-retinal hemorrhage
- Ocular sarcoidosis
- Subconjunctival hemorrhage
- Choroidal neovascular membrane
- Uveitis
- Ocular myasthenia
- Panophthalmitis
All aforementioned conditions can cause severe and permanent vision loss that may persist even after stopping interferon therapy and receiving appropriate ophthalmological treatment. While interferon may not be the sole cause of these complications, it could be contributing to some existing eye conditions. However, these severe cases are relatively rare and could therefore simply be coincidental or unrelated to the interferon treatment. With regards to different types of interferons, some studies have noted that interferon-associated retinopathy is more prevalent in patients receiving pegylated versions compared to standard ones.
Testing for Interferon-Induced Retinopathy
If you’re being treated with interferon and start experiencing issues with your eyes, your doctor will likely perform a detailed eye examination. This is particularly important for older people, those taking higher doses of interferon or taking it in combination with other medications, and people with pre-existing conditions like high blood pressure and diabetes.
The exam may include checks for visual sharpness, pupil examination, and a detailed exam of the back of the eye after dilation. Certain specialized tests, like fluorescein angiography and optical coherence tomography, can be used to identify potential issues. A fluorescein angiography may show areas of bleeding, impaired blood supply, or blockages caused by what are known as cotton wool spots. Optical coherence tomography can be particularly useful for detecting swelling of the macula, the part of the eye responsible for sharp, central vision, even in subtle cases.
The Food and Drug Administration recommends all patients undergo an extensive eye exam before starting treatment with interferon-α-2b. However, not all experts agree on the need for an initial examination, as the clear benefit of such an exam is not yet established. Regardless, any pre-existing eye disease in patients, specifically retinal disease, should be ruled out.
If you do have pre-existing retinal disease, your doctor will want you to have monthly eye exams while on interferon therapy. If you don’t have any symptom or existing retinal disease, you should get an eye exam every three months, unless you note a decline in your vision.
Treatment Options for Interferon-Induced Retinopathy
If a person undergoing interferon therapy experiences issues with their eyes, it’s generally suggested they stop the treatment. This is because issues with the back part of the eye, known as the “fundus,” usually get better quickly after stopping interferon. Interestingly, some changes in the light-sensitive layer at the back of the eye, called the “retina,” may even go away on their own, even if the person continues their interferon treatment without lowering the dose.
However, some medical professionals suggest only stopping treatment if the eye issues become severe. This includes serious changes in the retina, a drop in eyesight, other eye-related symptoms, or in persons who already have conditions like diabetes, which can affect eye health.
Reducing the dose of interferon is another way to deal with eye problems related to interferon. But it’s important to note that decreasing the interferon dose could potentially make the therapy less effective and worsen the person’s main health issue that required the treatment. So whether to stop or reduce the interferon dose is a decision made after weighing the potential risks and benefits, and also considering the information provided by the drug manufacturer.
What else can Interferon-Induced Retinopathy be?
When diagnosing a condition caused by interferon treatment that affects the eye (interferon-induced retinopathy), doctors need to take into account other health issues that can cause similar problems with the eyes. This may include:
- Hypertensive retinopathy (eye damage due to high blood pressure)
- Ocular ischemia (reduced blood flow to the eyes)
- Lupus retinopathy (eye problems due to Lupus, an autoimmune disease)
- HIV retinopathy (eye condition caused by HIV)
- Purtscher retinopathy and Purtscher-like retinopathy (specific types of eye inflammation)
- Retinopathy resulting from leukemia or lymphoma (blood cancers)
In people who have long-term Hepatitis C, it can cause retinopathy, which shows up as “cotton wool spots” and bleeding in the retina. Issues that add to the risk of this happening might include age, lower platelet counts, high blood pressure, being female, and having liver cirrhosis due to the Hepatitis C. It has been observed that the retinopathy symptoms often seem to get worse after the start of interferon treatment. More research is needed to understand the relationship between these systemic diseases and the eye problems they can cause.
What to expect with Interferon-Induced Retinopathy
The outlook for individuals who develop eye problems due to the use of interferon, a type of medication, is generally good. Most of the time, stopping the medication will resolve these eye problems. Sometimes, these eye problems go away on their own during treatment, which means it might not be necessary for patients to reduce the dosage of interferon they are taking. The vision outcomes are typically excellent and many people do not have any symptoms. This is why regular eye exams are so important – they allow for the early detection of any eye problems caused by interferon.
However, in some cases, the eye problems caused by interferon do not go away. There are a few rare instances in which individuals can have a bad vision outcome. For example, in one study, out of 1289 patients, one individual experienced a vision deficit due to interferon. Also, the unusual eye complications linked to interferon treatment can have poor vision outcomes, many times resulting in vision loss.
Possible Complications When Diagnosed with Interferon-Induced Retinopathy
The main problem that can come up with retinopathy (damage to the retina caused by a medication called interferon) is losing sight. While most people’s vision problems are minor and go back to normal, some can lose a lot of their sight. There are also other complications that can occur such as blockage of the blood vessels in the retina, a type of glaucoma caused by the growth of new blood vessels, and swelling in the macula (the part of the eye that controls our most detailed vision.)
Complications:
- Vision loss
- Blockage in the blood vessels of the retina
- Neovascular glaucoma
- Swelling in the macula
Preventing Interferon-Induced Retinopathy
Interferon therapy, a treatment used for different health conditions, might have the potential risk of causing a condition called interferon-induced retinopathy. This is a situation where small blood vessels in the retina (the part of your eye that helps you see) get damaged. This could lead to a decrease in vision sharpness and, in severe instances, blindness. Often, people with interferon-induced retinopathy may not feel any symptoms, and the damage might even reverse on its own, whether the therapy is stopped or not. However, the risk of losing vision still exists.
An eye doctor could look into your eye with an instrument called an ophthalmoscope and identify signs of retinopathy like cotton wool spots (pale, fluffy areas on the retina), retinal hemorrhages (bleeding in the retina), and macular edema (swelling in the central part of the retina).
It’s necessary for people to have a thorough eye check-up before starting interferon therapy and then continue with regular eye check-ups. This first eye check-up helps in taking note of the initial state of your retina, avoiding the beginning of interferon in individuals who already have a retina-related condition, like those with diabetes or high blood pressure. Keeping blood sugar levels and blood pressure under control is very important, as these can cause retinopathy.
In severe cases, interferon therapy might cause optic neuropathy (damage to your optic nerve that can lead to vision loss) and blockage of important retina’s veins and arteries, leading to vision loss. These situations need immediate medical attention. People on interferon therapy should quickly report any changes in their vision or other eye symptoms to their healthcare professional. Even though some individuals may be able to continue therapy without progression, most of them experience complete resolution after therapy is stopped.