What is Iritis?
The International Uveitis Study Group (IUSG) and the Standardization of Uveitis Nomenclature (SUN) working group both divide uveitis, an inflammation of the eye, into four categories: anterior uveitis, intermediate uveitis, posterior uveitis, and panuveitis. This classification is based on the part of the eye where the inflammation is present, not on whether the person has other eye problems, like cystoid macular edema, which is a swelling in the central area of the retina.
Anterior uveitis, which is when the inflammation is in the front part of the eye, is the most common type of uveitis. It can be further divided into iritis (inflammation of the iris, the colored part of the eye), anterior cyclitis (inflammation of the front part of the ciliary body, the part of the eye that controls the shape of the lens), and iridocyclitis (when both the iris and the front part of the ciliary body are inflamed).
Often, anterior uveitis appears suddenly and is caused by certain genes or unknown causes. Sometimes, it is hard to figure out the exact cause. It could be related to responses to bacteria or viruses in people with certain genetic dispositions. Potential causes can include viral or bacterial infections, injuries, inflammation related to the lens, keratitis (a condition affecting the cornea), or scleritis (a severe inflammation affecting the white part of the eye). Anterior uveitis can occur by itself or with one of the other forms of uveitis.
Chronic anterior uveitis (long-lasting inflammation in the frontal part of the eye) is much less common and usually affects both eyes. It often comes from an underlying health problem. Outcomes are generally good in most cases of acute anterior uveitis (sudden, short-term inflammation in the front part the eye), especially if it’s caused by certain genes or unknown causes, as long as they’re treated appropriately. However, outcomes can vary for individuals with chronic anterior uveitis or those with a related eye or health condition.
What Causes Iritis?
Most times, the lens of the eye becomes inflamed due to unknown reasons, a condition known as iritis. However, in about 20% of cases, it’s due to a direct injury to the lens.
Iritis that’s not due to trauma is often linked to HLA-B27 systemic diseases, which are a group of health conditions related to a specific gene. These conditions include Juvenile Rheumatoid Arthritis (a type of arthritis in children), Ulcerative Colitis (a bowel disease that causes inflammation and ulcers in the colon), Reiter syndrome (a form of arthritis that causes inflammation in various places in the body), Sarcoidosis (a disease that causes inflammation in various parts of the body), Behcet’s disease (a rare disorder that causes blood vessel inflammation), Tubulointerstitial Nephritis and Uveitis (kidney inflammation and eye inflammation), Systemic Lupus Erythematosus (an autoimmune disease that affects the skin, joints, kidneys and other organs), Multiple Sclerosis (a disease of the brain and spinal cord), and Ankylosing Spondylitis (a type of arthritis affecting the spine).
However, iritis can also be caused by infections, including Tuberculosis, Chlamydia, Lyme’s disease, Herpes Simplex, Toxoplasmosis, Varicella-Zoster virus (better known as chickenpox and shingles), and Syphilis.
Certain medications and conditions like lymphoma (a type of cancer), leukemia (a blood cancer), malignant melanoma (a type of skin cancer), and Juvenile Xanthogranuloma (a rare skin condition mostly seen in children) can also cause iritis.
After iritis of unknown cause, the second most common type of anterior uveitis (inflammation of the front of the eye) is associated with the HLA-B27 gene. It’s responsible for 40-70% of anterior uveitis cases, depending on the region, and is more commonly seen in males.
Some of the HLA-B27 associated conditions with eye involvement include Ankylosing Spondylitis, Reiter’s disease, Juvenile spondyloarthropathy, Psoriatic arthritis, Inflammatory bowel disease, and undifferentiated spondyloarthropathies. These conditions could cause various eye issues such as inflammation, dry eyes, and cataracts.
A large-scale study found that the most common causes of uveitis were unknown followed by seronegative spondyloarthropathies (a group of diseases involving the joints), Sarcoidosis, Juvenile Rheumatoid Arthritis, Systemic Lupus Erythematosus, Behcet’s, and HIV. These conditions commonly cause anterior uveitis. Posterior uveitis (inflammation at the back of the eye), on the other hand, is commonly caused by Toxoplasmosis, unknown reasons, CMV, Systemic Lupus Erythematosus, and Sarcoidosis.
Risk Factors and Frequency for Iritis
Anterior uveitis, a type of eye inflammation, is the most common form of uveitis, affecting 12 out of every 100,000 cases. This condition mainly impacts young and middle-aged people. In fact, in western countries, between 50% and 70% of all uveitis cases are classified as anterior uveitis. It’s also important to note that uveitis is responsible for 10% of legal blindness in the USA, resulting in around 30,000 new cases of blindness each year. Its prevalence rate is highest in elderly individuals above 65 and lowest in children, with more women being affected than men.
- Anterior uveitis is the most common type of uveitis, affecting 12 out of every 100,000 cases.
- It predominantly affects young and middle-aged populations.
- In western countries, 50% to 70% of all uveitis cases are anterior uveitis.
- Uveitis accounts for 10% of legal blindness in the USA and approximately 30,000 new cases of blindness per year.
- The incident rates of uveitis are highest in people over 65 and lowest in children.
- The condition is more prevalent among women compared to men.
There are variations in the incidence and prevalence of uveitis based on geographical locations and specific subtypes of uveitis. For example, a study conducted in northern California reported an incidence of 52.4 cases per 100,000 people per year and a prevalence of 115.3 cases per 100,000 people. Furthermore, the incidence rates reported from the Northwest Pacific were lower, standing at 25.6 cases per 100,000 people, with a prevalence of 69 cases per 100,000 people.
- A study in northern California found an incidence of 52.4 cases per 100,000 people per year and a prevalence of 115.3 cases per 100,000 people.
- A separate study from the Northwest Pacific reported an incidence of 25.6 cases per 100,000 people and a prevalence of 69 cases per 100,000 people.
In the elderly population, uveitis’ incidence ranged between 302 and 424 cases per 100,000 people per year, with an average of 340.9 per 100,000 individuals. The mean incidence of uveitis was 243.6 per 100,000. It is also noteworthy that the reported cases of posterior uveitis and panuveitis, two different forms of uveitis, were 76.6 and 41.7 per 100,000, respectively.
- The incidence of uveitis in the elderly ranges from 302 to 424 cases per 100,000 people per year, with an average of 340.9 per 100,000 people.
- The overall incidence of uveitis stands at an average of 243.6 cases per 100,000 people.
- Posterior uveitis has an incidence of 76.6 cases per 100,000 people.
- Panuveitis has an incidence of 41.7 cases per 100,000 people.
Signs and Symptoms of Iritis
Uveitis, an inflammatory condition of the eye, can be categorized according to where it occurs (anatomical classification), what causes it (etiological classification), how long it lasts (timing of inflammation), and how it presents (clinical activity). The Standardization of Uveitis Nomenclature (SUN) Working Group, International Uveitis Study Group (IUSG), and others have proposed various classification systems.
Anatomical classification:
- Anterior Uveitis – affects the iris and ciliary body
- Intermediate Uveitis- affects the vitreous and pars plana
- Posterior Uveitis – affects the retina and choroid
- Panuveitis – affects the anterior, intermediate and posterior areas of the eye
Etiological classification:
- Infectious – caused by viruses, bacteria, parasites, or diseases such as Lyme disease
- Non-infectious – may be idiopathic or associated with systemic diseases
- Masquerade – symptoms may mimic neoplastic (cancerous) or non-neoplastic conditions
Timing of onset and duration of inflammation:
- Insidious or sudden onset
- Limited (lasting less than or equal to 3 months) or persistent
Clinical activity:
- Chronic – the condition persists and may relapse within three months after stopping the treatment
- Recurrent – There are repeated episodes with periods of no activity in between
- Remission – No active episodes for three months or more
Examining the eye with a device called a slit lamp can provide further information about the uveitis, such as location and severity. Specific findings like anterior chamber cells, flare, and erythema can indicate the degree and activity of inflammation. Other signs, like the presence of iris nodules or neovascularization, help identify the type of uveitis. Keeping track of these signs and symptoms can also reveal whether the uveitis is acute or chronic, or classified as granulomatous or non-granulomatous.
Testing for Iritis
If you are diagnosed with iritis, it means there’s inflammation in the front part of your eye, also known as anterior uveitis. Your doctor’s tests and treatment will focus on addressing this inflammation. In some instances, if your doctor suspects other health problems or infections are causing your eye issue, they may order further tests or imaging.
In general, most patients with this type of eye inflammation show normal test results, meaning the underlying cause can’t be pinpointed. It’s essential that each patient receives tailored investigations based on their specific symptoms. Sometimes, the cause of the inflammation is obvious, such as inflamed eyes following eye surgery. It’s often necessary for patients to be reviewed by an internal medicine doctor as well.
Your eyesight or visual acuity is usually slightly affected in cases of iritis. The degree to which it’s affected depends on the inflammation and related complications. Your doctor will monitor your vision during each visit, with an improvement in visual acuity signaling that the inflammation is receding.
Iris inflammation can sometimes raise the pressure within your eye, known as intraocular pressure (IOP). This pressure can be measured in various ways and will be checked at each visit. A drop in IOP can happen due to decreased fluid secretion from the eye, while increased IOP may arise from various causes.
It’s important to note that tests are not always mandatory for patients with iritis – for example, if this is your first incidence of mild iritis and you have a clean medical history. In other cases, such as severe, recurrent, or chronic instances of iritis, tests might be beneficial. The need for tests also depends on your symptoms and whether they hint at potential underlying causes.
Imaging tests, like chest X-rays, might be useful if diseases such as sarcoidosis or tuberculosis are suspected to cause your iritis. Tools like B Scan ultrasound, optical coherence tomography, and indocyanine green angiography could also be deployed to evaluate your eye condition. Your doctor will decide on the tests based on the specifics of your condition.
While routine laboratory tests aren’t always necessary for people with iritis, multiple tests like the Human Leucocyte Antigen tissue typing (HLA-B27), Syphilis Serology, Complete Blood Count, and others might be required, especially in cases of recurrent or bilateral iritis. Remember, even if your eye inflammation is mild and without systemic disease or trauma evidence, your doctor may still recommend laboratory tests.
In conclusion, diagnosing the underlying cause of iritis involves multiple tests depending on the individual’s symptoms. These can include imaging and several laboratory evaluations. Furthermore, a timely review by an internal medicine doctor can be crucial in identifying the cause accurately. For example, specific tests like a high-resolution CT scan in case of suspected pulmonary tuberculosis, or an MRI in case of potential multiple sclerosis, may be requested upon referral.
Treatment Options for Iritis
The treatment for uveitis, a condition which causes inflammation inside the eye, primarily focuses on reducing inflammation and pain, and preventing the condition from getting worse. Eye drops that dilate the pupil along with steroid drops are usually used as a first line treatment. These treatments can help to minimize the risk of the muscles around the pupil spasming and also to lessen inflammation in the eye. It’s important that the patient seeks the advice of an eye specialist within 24 to 48 hours of starting the treatment. The frequency of check-ups is based on the degree of inflammation and the specific symptoms experienced by the individual.
In more serious cases of inflammation, slow-release steroid implants can be put in the jelly-like substance in the eye to lessen inflammation. It should be noted, however, that the use of steroids should always be done in consultation with an eye specialist, as uveitis needs to be definitively diagnosed before steroids can be safely prescribed.
While steroids can be effective in treating uveitis, they may also cause some side effects such as increased pressure in the eye, cataract formation, steroid-induced glaucoma and the risk of herpes in the eye. If there is an ongoing need for steroid use to control the inflammation, medications that prevent a loss of potassium should be used. About half of all individuals with uveitis will need treatments beyond steroids to avoid the risk of losing vision.
Eye drops containing corticosteroids, which are drugs that help to reduce inflammation, are usually the first choice for treating uveitis. These drops work by reducing inflammation by targeting specific processes in the body that cause inflammation.
Cycloplegics, a kind of medication, are also commonly used to treat uveitis. They work by blocking nerve signals to certain muscles in the eye, which helps to reduce the discomfort caused by light (photophobia) and pain. They are also able to help the eye heal by breaking up and preventing adhesions in the eye, which are bands of scar tissue that can limit the movement of the eye muscles.
There are a variety of other medications and treatments that may be used to treat specific cases of uveitis, such as injections of steroids into the eye or oral steroids. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), cancer-fighting drugs known as antimetabolites, or medications that block a substance called tumor necrosis factor (TNF blockers) may also be used under certain conditions and with the supervision of a physician.
What else can Iritis be?
When it comes to diagnosing eye-related health issues, doctors typically consider various conditions. The list of possible diseases or issues may include:
- Acute angle-closure glaucoma
- Conjunctivitis (Pinky eye)
- Subconjunctival hemorrhage (bleeding in the eye)
- Trauma (damage from an injury)
- Episcleritis (inflammation of the outer layer of the eye)
- Scleritis (inflammation of the white part of the eye)
- Dry eyes
- Pingueculitis (inflammation of a small bump on the eye)
- Inflammed pterygium (growth on the eye)
- Corneal abrasion (scratch on the eye)
- Corneal ulcer (open sore on the eye)
- HSV keratitis (infection of the cornea)
- Intraocular foreign body (something in the eye that doesn’t belong)
- Ultraviolet keratitis (damage to the cornea from UV light)
What to expect with Iritis
The outlook is generally positive with proper treatment. Seeing an eye doctor within 24 hours is crucial for the best outcome. Your eye doctor will routinely check your eyes using a specialized microscope called a slit-lamp and measure the pressure in your eye over several days. Once the condition is stable, these checks might occur anywhere from every month to every six months.
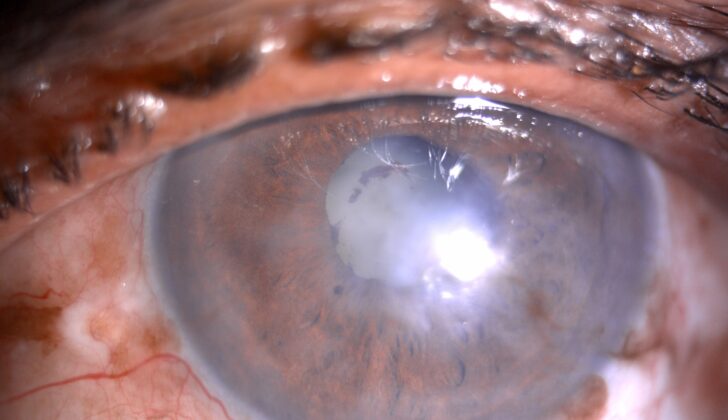
However, if the condition isn’t diagnosed and treated promptly, complications like cataract (clouding of the eye lens), glaucoma (an eye condition that damages your optic nerve), retinal detachment (a medical emergency where the retina pulls away from the tissue at the back of the eye), and macular edema (buildup of fluid in the macula, part of the eye needed for sharp, straight-ahead vision) can occur. Unfortunately, the outlook for these cases where complications have developed is less assured.
Possible Complications When Diagnosed with Iritis
- Scarring on the cornea (keratouveitis)
- Band like clouding of the cornea (band shaped keratopathy)
- Blood in the front part of the eye (hyphema)
- An eye condition where pus doesn’t get better (non-resolving hypopyon)
- Shrinkage and loss of color in the iris (iris atrophy)
- Iris sticks to the lens of the eye, potentially restricting eye movement (posterior synechiae)
- Clouding of the eye (cataract), which can be due to inflammation or a reaction to steroid treatment
- Increased pressure in the eye leading to potential vision damage (secondary glaucoma), which can result from a blockage of your eye’s drainage angle (pupillary block), inflammation, or use of steroid eye drops
- Blockage of the pupil with the iris (occlusio pupillae)
- Pupil that is stretched out (festooned pupil)
- Blockage of the pupil with inflammation (seclusio pupillae)
- Swelling in the central part of the retina, causing vision loss (cystoid macular edema)
- Damage to the optic nerve (optic neuropathy)
- New, abnormal blood vessels growing in the optic disc (optic disc neovascularization)
- A scar in the macula region of your eye (macular scar)
- Abnormally low eye pressure (hypotony)
- Bleeding into the vitreous, which is the clear gel that fills the space between the lens and the retina of your eye (vitreous hemorrhage)—this can be associated with inflammation inside the eye (intermediate, posterior, or panuveitis)
- Retinal detachment, or pulling away of the retina from its normal position
- An inflammation inside the eye, caused by an infection (endophthalmitis)
- Infection and inflammation of all layers of the eye (panophthalmitis)
- Total loss of sight (permanent blindness)
- Eyes that are not aligned with each other (strabismus)
Recovery from Iritis
If you have cataract surgery, after the procedure you’ll need to take care of your eye, especially if you also have a condition called glaucoma that’s getting worse or not improving. After your cataract surgery, the common treatment includes eye drops that have steroids (like 1% prednisolone or 0.1% dexamethasone) or a combination of steroids and an antibiotic (0.1% dexamethasone + 0.5% gatifloxacin), applied a decreasing number of times each day for a week. You’ll also use an eye drop that relaxes your eye muscles (a ‘cycloplegic’) – most likely 5% homatropine or 1% atropine – twice daily for about 2 to 3 weeks.
Your doctor will want to monitor you frequently after surgery to catch and address any problems early on. If you had surgery for glaucoma (known as ‘filtration surgery’), you’ll use the same eye drops as mentioned above, but apply them a larger number of times each day for a week, along with the cycloplegic. Regular follow-ups are important to check for complications like a rare vision-threatening event (macular snuff out), low eye pressure (hypotony), uncontrolled glaucoma, and to ensure the new drainage pathway in your eye (the bleb) is working properly.
If you’ve had surgery to fix a detached retina, your aftercare requires the same treatment as glaucoma patients. You’ll also have to have an operation to remove silicone oil 2 to 3 months later. It’s vital you keep up with your follow-ups to make sure your retina doesn’t detach again and to monitor any other complications from your eye surgery.
Preventing Iritis
Patients suffering from iritis, a type of eye inflammation, should understand how this condition affects the eye and the importance of consistently receiving treatment and regular check-ups. They should also know about any underlying health conditions that could be linked to their iritis and the crucial task of the internal medicine doctor in managing the condition. Patients must also be informed about any complications that might arise from iritis and possible side effects from inconsistent or prolonged use of steroids, a common medication used in treatment.