What is Keratoconus?
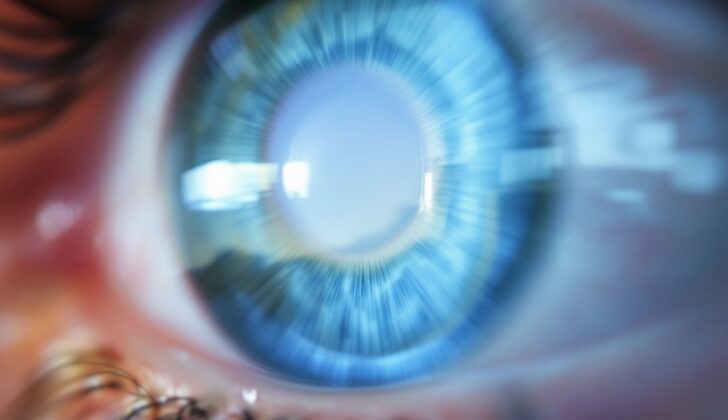
Keratoconus is a condition that causes the clear front part of the eye, the cornea, to bulge into a cone shape. This condition affects both eyes and can progress and worsen over time. Due to this distortion, patients often experience significant loss of vision. It is one of the main reasons for corneal transplantation, a surgery to replace the clear front part of the eye, in Western countries. The condition is normally noticed during adolescence or early adulthood and can be connected with other health problems.
The term ‘Keratoconus’ is derived from Greek words meaning “cornea” and “cone.” It was first thoroughly described by Dr. John Nottingham, a British doctor, in 1854. He observed that keratoconus has unique characteristics, making it different from other eye shape disorders.
For people suffering from keratoconus, the usual problems include notable and variable reduction in eyesight, image misrepresentation, and increased light sensitivity. These conditions hamper the ability of traditional glasses to correct vision properly. Keratoconus can cause nearsightedness and blurry vision, which results from reshaping and scarring of the cornea. In some cases, the condition may not show any symptoms and could be classified as a slightly uneven form of astigmatism, which is an irregular curve of the eye’s cornea or lens.
Emerging research contradicts the older belief that keratoconus has no connection with inflammation. It reveals that changes in substances causing inflammation might result in inflammatory changes in eyes affected by keratoconus. The condition is more common in individuals with a family history of keratoconus, and it may present alone or alongside other vision or health conditions. Although keratoconus affects both eyes, one eye may have more pronounced symptoms than the other. In severe cases, it may lead to sudden swelling of the cornea, known as acute corneal hydrops.
By the time a person enters their forties, the progress of the disease usually slows down. The main goal of treatment is to correct vision and keep the disease from progressing. Early treatment options may include a method to strengthen the cornea known as corneal collagen cross-linking, which can help slow down or stop the disease’s progression. While many patients manage the disease with the use of hard gas-permeable contact lenses, in extreme cases, some patients may need to undergo corneal transplantation.
What Causes Keratoconus?
Understanding the causes and development of keratoconus, which is a disorder of the eye that causes the cornea to become cone-shaped, is a bit complicated. It’s difficult to study because there are no adequate animal models, preserved human eye samples rapidly break down, and there aren’t enough healthy human eyes for comparison. People with keratoconus usually have less collagen, a type of protein, in their corneas than normal. As the disease gets worse, there’s a complex series of damaging and healing processes happening in the eye.
While we may not fully understand what causes keratoconus or how it progresses, we do know some risk factors that may make a person more likely to develop the condition:
- Systemic conditions: Certain illnesses like Down syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, Leber congenital amaurosis, and Noonan syndrome can increase the risk of developing keratoconus.
- Environmental factors: Some research has suggested a connection between keratoconus and conditions that are related to the environment, such as allergies, asthma, and hay fever.
- Eye rubbing: Rubbing your eyes often seems to either cause or worsen keratoconus. If a person is genetically predisposed to the disease, persistent eye rubbing or the use of hard contact lenses may cause injuries to the eye, thereby contributing to keratoconus advancing. These injuries may cause cells in the cornea, called keratocytes, to change and start repairing the damage, which could be related to the disease.
- Family and genetics: Having someone in the family, especially a close blood relative, with keratoconus greatly increases the risk of developing the disease. These individuals are up to 67 times more likely to get the condition than those without a family history. And while the disease usually appears randomly, 90% of patients who have a family history show a pattern of inheritance from one parent with a decrease in full expression of the disease. The rest tend to show a pattern of both parents passing on the trait, especially in families where the parents are closely related.
Modern eye scanning techniques can identify people who don’t show symptoms, broadening our understanding of cases related to family history. Although we’ve linked the development of keratoconus to a majority of our chromosomes, we’ve only confirmed one specific area on one of the chromosomes having an impact. This suggests that multiple genes are involved in developing the disease.
Research on key genes thought to be involved in the development of the disease, such as VSX1 and SOD1, haven’t given clear results yet, hinting that specific mutations along with variations in other ‘modifier’ genes may be integral to the disease showing up. So, it appears that both genetic and environmental factors play a role in the development of keratoconus.
Risk Factors and Frequency for Keratoconus
Keratoconus is a condition that usually starts showing signs during adolescence or early adulthood, and may continue to progress until around the fourth decade of life. It’s not more common in any specific gender, and while some studies suggest it may be more widespread among people of Asian descent from the Indian subcontinent, there isn’t concrete evidence to confirm this. It is worth noting, though, that Black and Latino people may have a 50% higher chance of developing keratoconus compared to White individuals.
- The condition affects between 50 and 230 out of every 100,000 people in the general population, with a recent extensive study suggesting an average prevalence of around 138 per 100,000 people across 15 countries.
- Thanks to more accurate and sensitive diagnostic tools, we’re now able to identify keratoconus even in more subtle cases, revealing it to be perhaps as high as 1 in 375 in some populations.
- In certain areas, such as the Middle East and particularly among Saudi Arabian adolescents, keratoconus is notably high with around 4790 cases per 100,000 people.
- Around 6% to 8% of keratoconus cases have been found to run in families.
- People with Down syndrome also seem to be more susceptible, with keratoconus rates ranging from 0.5% to 15%.
- Furthermore, this condition is quite common with individuals who have Leber congenital amaurosis (a severe congenital form of vision loss), affecting up to 30% of people aged 15 and above, and with patients who have a heart condition known as mitral valve prolapse, where it affects 58% of such patients.
Signs and Symptoms of Keratoconus
Keratoconus is a condition that usually shows up during puberty or early adulthood. It often starts with blurred vision or a sudden decrease in the ability to see clearly. One of the first signs may be the difficulty in improving the person’s eyesight to 20/20, even with corrective lenses. The symptoms of Keratoconus may last and gradually worsen until around the age of 40. Initially, glasses might help with vision correction, but as the condition worsens, contact lenses may become necessary due to the development of an irregular eye curvature.
Even though a person with Keratoconus often shows typical signs like a bump outwards in the cornea of the eye and a ‘scissors reflex’, these symptoms and their links to the disease’s severity can vary greatly. The ‘scissors reflex’ refers to two bands moving towards and away from each other when the eye is examined using a retinoscope.
Keratoconus is often associated with significant shortsightedness, but this alone cannot confirm the disease. The main signs include an irregular eye curve and localized thinning of the cornea, the transparent front part of the eye. Doctors must distinguish between localized thinning and overall thinness of the cornea. An evenly distributed, significant eye curvature is not indicative of Keratoconus. Instead, the condition is usually accompanied by a highly uneven eye curvature. Both the thinning of the cornea and this uneven curvature often occur in the area of the corneal bump, typically located in the lower outer area of the eye.
- Difficulty with visual correction: As the disease progresses, increasing shortsightedness and uneven curvature of the eye can make it challenging to correct vision using glasses or fit contact lenses.
- Asymmetric visual complaints: Even though Keratoconus typically affects both eyes, one eye may be more severely affected. Around 41% of patients report one-sided disease at the time of diagnosis.
- Münson sign: In advanced stages of Keratoconus, a v-shaped indentation in the lower eyelid may occur when looking down due to a prominent corneal bump.
- Fleisher ring: This brown-colored marking, best seen with the cobalt blue filter on the slit lamp, consists of iron from the tear film that accumulates around the base of the cornea’s bump. Fleisher rings can act as a subtle early sign of Keratoconus.
- Vogt striae: These are vertical lines caused by compression of the back lining of the cornea and are visible in the thinnest area of the cornea. Applying gentle pressure to the cornea can make these lines disappear.
- Rizzuti sign: This appears as a bright reflection from the side of the eye near the nose when light is shone on the side of the eye near the temple.
- Central and inferior paracentral corneal thinning: The early signs of Keratoconus include thinning in the central and upper-mid parts of the cornea, along with mild bump formation and protrusion.
- Corneal hydrops: This can occur in the advanced stages of Keratoconus and may cause sudden, painful vision loss and sensitivity to light. About 3% of people with Keratoconus experience corneal hydrops, with an average onset around the age of 25. Men may be more likely to experience corneal hydrops. Certain risk factors, such as allergies and the overall severity of the disease, may be associated with its occurrence.
- Corneal scarring: This is a result of spontaneous breaks in the protective layers of the cornea as it thins from Keratoconus. Nearly 20% of patients with Keratoconus have scarring in the cornea.
Testing for Keratoconus
The first step in diagnosing keratoconus, an eye condition that affects the shape of your cornea, involves measuring the way your eyes focus light, which is known as ‘refraction’. Healthcare professionals then use additional tools to learn more about the condition. These include a thorough examination of the front part of your eye, featuring a ‘slit-lamp biomicroscopy’, a ‘corneal topography’ that maps the front surface of the cornea and a ‘corneal tomography’ that creates a 3D map of the cornea. The thickness of your cornea may also be measured through a technique called ‘pachymetry’. Both corneal topography and tomography are particularly efficient at spotting early signs of keratoconus.
At first, a slit-lamp examination may appear normal in the early stages of keratoconus. However, as the condition advances, common changes might be seen including Fleischer rings and Vogt striae, unique patterns that form in the cornea, together with corneal thinning and scarring.
Corneal topography uses reflected patterns to evaluate the anterior, or front, curvature of your cornea, converting these patterns into color scales for easy interpretation. Meanwhile, corneal tomography considers both the thickness and the back curvature of your cornea, delivering a complete assessment of the cornea’s shape.
If you have early keratoconus, your slit-lamp examination might appear normal. Therefore, corneal imaging plays a crucial role in early detection. It is also useful in monitoring the progression of the disease and aiding treatment decisions. Common topographic patterns might include an asymmetric bowtie with or without steepening in the lower part of the cornea, or a superonasal flat area of decreased steepening. It is rare for patients to present with changes in the central part of the cornea.
Anterior segment optical coherence tomography (OCT) is an imaging test that has become very important in diagnosing keratoconus. OCT allows doctors to take cross-section pictures of the cornea revealing both the asymmetrically thinning cornea and a condition called posterior curvature asymmetry.
A hallmark of the eye’s surface layer or the epithelium is its variable thickness, this can sometimes disguise the irregularities in the underlying thickness of your cornea. As a result, it may seem that your corneal thickness is relatively uniform when in fact, it isn’t — this can hide early signs of corneal thickness fluctuations.
Simple tests such as retinoscopy and keratometry, which measure the way light bounces off the back of your eye and project a circular pattern onto your cornea respectively, can be helpful. These reveal a specific pattern of reflection called a ‘scissoring reflex’, as well as irregular patterns and corneal steepening which are common observations in people with keratoconus.
Pachymetry, a test to measure the thickness of the cornea, is often employed. These devices can map out areas of corneal thinning, usually at the location of the steepest part of the cornea. This asymmetry is a specific and reliable indicator of keratoconus.
The eye affected by keratoconus shows a significant difference between the front and back regions of the cornea relative to a normal eye. This noticeable difference is seen through OCT or through a technology called Scheimpflug imaging. These tests could accurately discern mild cases of keratoconus from normal eyes as they have a high specificity of 96% and sensitivity of 92%
In the recent decade, there has been growing interest in examining the cornea’s structure for detecting keratoconus. This is because of new tools that evaluate corneal properties based on their reaction to deformation. Early detection markers for keratoconus have been identified from these altered properties. However, these somewhat correlate with corneal thickness, thus their effectiveness in distinguishing normal eyes from early or advanced keratoconus is not yet clear, especially after corneal surgery.
Even though physical symptoms and examinations are extremely important, corneal topography remains a primary tool for detecting changes in the cornea. Combining different measurements such as pachymetry and corneal aberration data together with topography, increases diagnostic accuracy especially in early cases. Emerging imaging techniques such as corneal tomography further enhance sensitivity and specificity in identifying corneal changes. Additionally, the ongoing development of computer algorithms that can learn independently without being explicitly programmed hold promise for identifying the early stages of the disease, thus improving both early detection and ongoing management of keratoconus.
Treatment Options for Keratoconus
The treatment for keratoconus, a condition that affects the shape of your eye, is personalized to you. This is because the goal of treatment is to improve your vision and prevent the disease from getting worse, and everyone’s needs can be different. However, generally, we focus on correcting vision first, and then work to prevent the disease from progressing in all patients.
In the early stages of keratoconus, we usually start by prescribing glasses to improve your vision. As the condition progresses, you may notice your vision getting worse due to increased astigmatism – a type of refractive issue that causes distorted vision. At this stage, we often recommend contact lenses. In fact, about 90% of people with keratoconus use these lenses for treatment.
Then there are special contact lenses for keratoconus patients called rigid gas-permeable lenses. They are often preferred because they eliminate corneal irregularities – distortions in the front surface of the eye – and help to create a tear film behind the lens. However, some patients may find them uncomfortable, especially if they have scarring on their cornea.
For those who aren’t comfortable with standard contact lenses, there are other options like hybrid lenses, scleral lenses, and piggyback lenses which combine a rigid lens over a soft one. Scleral lenses, which are filled with saline solution before being put in, rest on the white part of your eye without touching the cornea, which makes them more comfortable and reduces the risk of scarring.
A system known as PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem), where custom-designed prosthetic devices are used, is another alternative option for treating keratoconus. These devices have been shown in studies to improve vision more quickly than standard corneal transplants.
For those with severe keratoconus or who cannot tolerate standard contact lenses, scleral lenses may be used. In cases where contact lenses are ineffective, we may need to consider surgical interventions.
Surgery can involve a technique called corneal collagen cross-linking, which helps stop keratoconus from getting worse by strengthening and stabilizing the cornea. This involves removing a small part of the central cornea, applying a solution called riboflavin, and exposing the eye to UV-A light. This process helps to strengthen the cornea by creating bonds in its stroma, the supportive tissue in the middle layer of the cornea.
It’s important to note that some people might not be suitable for this procedure, such as those with very thin corneas or a history of certain eye conditions. Additionally, while the procedure can help prevent your vision from getting worse, it doesn’t directly improve your eyesight, so you might still need glasses or contact lenses afterwards.
There are also refractive surgeries which help manage keratoconus after your condition has been stabilized. These surgeries can reshape the front portion of your cornea to improve your vision, or we can implant thin, semi-circular plastic inserts into the mid-layers of your cornea to flatten it and reduce astigmatism, potentially avoiding the need for a corneal transplant.
If these treatment options aren’t effective, you might need a corneal transplant. This procedure, where we replace your cornea with donor tissue, is the treatment of choice when contact lenses don’t provide enough vision correction. The type of transplant you’ll get can depend on how much of your cornea is diseased and needs to be replaced.
Keep in mind that these treatments are all designed to help manage your symptoms and stop keratoconus from getting worse. However, the best treatment option for you can depend on your unique situation and how advanced your condition is.
What else can Keratoconus be?
When diagnosing keratoconus, which is a disorder that results in thinning of the eye’s clear front surface, a doctor needs to make sure they have ruled out other possible conditions. These can include:
- Complications from wearing contact lenses
- Warpage of the cornea caused by contact lenses
- Corneal ectasia, a bulging of the cornea
- Ectasia as a result of refractive eye surgery
- Diplopia, or double vision
- Interstitial keratitis, inflammation of the cornea
- Keratoglobus, a rare condition causing the cornea to bulge all around
- Pellucid marginal degeneration, thinning of the lower part of the cornea
- Posterior keratoconus, a rare, non-inherited disorder
- Terrien marginal degeneration, a condition that slowly thins the cornea
- Scarring of the cornea
- Inherited disorders such as congenital hereditary endothelial dystrophy
- Other conditions that cause the cornea to degenerate such as Fuchs endothelial dystrophy
- Infectious or non-infectious keratitis
It’s crucial for the doctor to carefully consider these possibilities and conduct the proper tests to make an accurate diagnosis.
What to expect with Keratoconus
Keratoconus is an eye condition where the front part of the eye, known as the cornea, begins to thin and bulge outwards. This can lead to problems with vision. Similar to many diseases, how fast and severely it progresses can vary from person to person. Factors such as young age and having more curvature in the cornea at diagnosis time make it more likely for the condition to get worse. Progression can also lead to cornea scarring and worsen vision.
About 10% to 20% of people with keratoconus may eventually need surgery to replace the cornea. However, early steps like corneal collagen cross-linking, a procedure which strengthens the cornea, can slow down or stop the disease from getting worse. It’s very important to diagnose this issue early and manage it correctly, using regular check-ups and corrective lenses.
Research suggests that although the disease can progress, for most people it gets stable over time.
Possible Complications When Diagnosed with Keratoconus
The complications of keratoconus, a condition that affects the eye, are a variety of eye-related problems. These can include getting more nearsighted or developing astigmatism, scarring of the cornea, thinning of it, and experiencing a sudden swelling in the cornea. People might also find that they are more sensitive to light, have a hard time wearing contact lenses, and their vision might get worse even when they use corrective lenses. Other issues that could occur are Vogt striae (stress lines in the deeper parts of the cornea), the need for a corneal transplant, seeing glare or halos at night, scarring at the tip of the cornea, and new blood vessels forming at the edges of the cornea. If the situation is severe, it may be necessary to get a corneal transplant, which also comes with its own risks like graft rejection and a hazy cornea. Finally, after a procedure known as corneal collagen cross-linking, there could be complications like keratitis, swelling in the cornea, pain, and blurred vision.
List of Potential Complications:
- Increasing nearsightedness and astigmatism
- Scarring of the cornea
- Thinning of the cornea
- Sudden swelling in the cornea
- Increased light sensitivity
- Difficulty wearing contact lenses
- Deteriorating vision despite corrective measures
- Vogt striae (stress lines in the deep parts of the cornea)
- Need for corneal transplant
- Seeing glare or halos at night
- Scarring at the tip of the cornea
- New blood vessel formation at the edges of the cornea
- Graft rejection and hazy cornea post-transplant
- Keratitis, corneal edema, pain, blurred vision after corneal collagen cross-linking
Recovery from Keratoconus
Here’s a simple guide on how to care for your eyes and aid recovery after undergoing specific surgeries to treat a condition called keratoconus, where the clear tissue on the front of the eye, the cornea, becomes irregularly shaped.
After undergoing Corneal Collagen Cross-Linking you will need to protect your eye, usually with something like a bandage contact lens. You’ll also be given antibiotics and anti-inflammatory eye drops. It’s very important to avoid rubbing your eyes to reduce the risk of further irritation or harm. You will also need to make regular appointments with an eye doctor, known as an ophthalmologist, to monitor your healing and catch any complications early.
In the rehabilitation phase after this surgery, you may need to wear glasses or special contact lenses to correct vision issues as your cornea heals. Regular eye exams are also necessary to monitor how your condition progresses and to see how effective the treatment is.
If you have a Corneal Transplant surgery, after the procedure you should use an eye patch or shield and apply medicated eye drops to keep your eye safe, prevent infection, and control any inflammation. You will need to visit your ophthalmologist regularly, as this is important in tracking your healing and adjusting your medications as necessary. Avoid heavy lifting and activities that strain your eye.
As you recover, remember that improvement in your vision may be gradual and may take several months. You may also need prescription glasses or contact lenses to help with vision correction as your eye adjusts after the surgery. Lifelong check-ups with your ophthalmologist are crucial to identify and manage potential issues, like graft rejection, and to ensure your eye stays healthy and your vision keeps improving.
For the procedure involving Intacs, which are small plastic ring-shaped inserts placed in the cornea to reshape it, you’ll need to protect your eye at night with an eye shield while sleeping. You will also have to use prescribed antibiotics and steroid eye drops. Avoid exposing your eyes to water to keep infection at bay.
During your recovery, you might still need glasses or contact lenses to correct your vision. Regular appointments with your ophthalmologist are necessary to check how you’re healing and if the intacs are properly aligned.
The kind of care and rehabilitation you’ll need after surgery for keratoconus depends on the type of procedure you’ve undergone. Whatever the procedure, it’s crucial to follow a personalized plan which includes regular check-ups, taking medication as prescribed, protecting your eyes, and possibly needing glasses or contact lenses. Teamwork between you and your eye care team, which consists of your ophthalmologist, an optometrist, and other rehabilitative specialists, is vital for the best results.
Preventing Keratoconus
To help manage and slow down the progression of keratoconus, which is a condition that causes the cornea (the clear front surface of your eye) to become thin and gradually bulge outward, there are several deterrent strategies and education approaches that can be followed.
Regular eye check-ups are a must for catching keratoconus early on. This allows any necessary treatment to start as soon as possible.
People with this condition are also encouraged to make certain changes in their routine. For example, protecting the eyes by not rubbing them and wearing sunglasses when you’re outside can help prevent the disease from getting worse.
If keratoconus affects one person in a family, other members should be screened as well. This is because the condition can sometimes run in families. By doing this, doctors can catch and treat it early in other family members.
Additionally, it’s good to stay away from things that can make the condition worse, like straining your eyes for too long or wearing contact lenses that don’t fit right.
It is also important for people with keratoconus to understand their condition well. Knowing about the symptoms of keratoconus and the importance of regular eye check-ups motivates them to play an active part in managing this condition.
Patients should also be informed about all the treatment options available. This includes glasses, procedures like collagen cross-linking (a treatment which strengthens the cornea), and surgery. The more they know, the easier it is for them to make decisions that suit their needs.
Proper eye care habits also need to be taught to patients. These include not rubbing the eyes and handling contact lenses the right way. This can help to reduce some of the risks associated with keratoconus.
Providing emotional support is crucial as well since keratoconus can have an impact on a person’s quality of life. Connecting patients to support groups can be very helpful.
It’s crucial for patients to follow their doctor’s treatment plan, attend all their appointments, and act on the doctor’s advice. This helps in managing keratoconus in the best possible way.
Overall, the combined efforts of the patient, their family doctor, and their eye specialist are key to managing keratoconus effectively. Regular eye examinations, making key lifestyle changes, and educating oneself about the condition can help slow or even stop the progression of this eye condition, ensuring a better quality of life.