What is Leber Hereditary Optic Neuropathy (LHON)?
Leber hereditary optic neuropathy (LHON) is a rare eye disorder, chiefly affecting young males, which causes progressive vision loss due to decay of the optic nerve. This condition is unique because it’s most commonly inherited from the mother and linked to mutations in the mitochondrial DNA (mtDNA), which are specific changes in our genetic material that produce energy for our cells. In 90% of cases, this condition results from three particular gene mutations. However, it’s important to note that even if these mutations are present, not everyone will show symptoms because of different levels of these gene mutations present in different body tissues, a situation termed ’tissue heteroplasmy’. Factors like genetics, environment, other genes carried on the X chromosome, and immune system conditions influence the onset and progression of the disease.
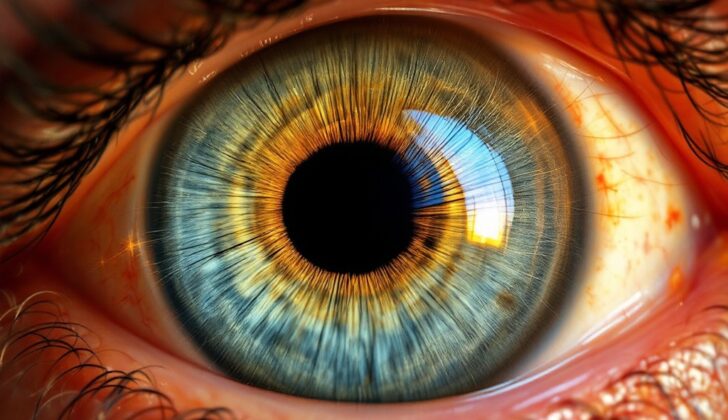
LHON usually begins without any pain in one eye and then advances to the other eye within a year. This condition causes serious vision loss, difficulty distinguishing colors, and trouble seeing the central field of vision. The diagnosis of LHON can be aided by an ocular examination called a fundus examination, yet even without changes in this examination, LHON can still be present. Recent technologies, such as optical coherence tomography (OCT)—an imaging test that provides pictures of the retina—have helped in comprehending and monitoring the disease’s stages better.
The management of LHON entails lifestyle modifications, vitamins supplements, and a medication called idebenone, which is used in the early stages of the disorder, hoping to recover vision. Nevertheless, most cases experience permanent vision loss, which requires ongoing supportive care and genetic counseling to help affected individuals and their families understand the condition better.
What Causes Leber Hereditary Optic Neuropathy (LHON)?
LHON was the first disease found to be linked to changes in mtDNA and is passed down through the mother. Both parents contribute to the zygote (the cell formed by the union of an egg and sperm), but the mother’s egg actually supplies the contents of the cell, including many mitochondria. This is what is referred to as ‘maternal inheritance’: the mother passes on the mitochondrial genes to all her children without any contribution from the father’s mtDNA. Mitochondria are the energy factories of our cells, especially necessary in those parts of our bodies that need a lot of energy, like our optic nerves and the retina.
If a new mutation (or change) occurs in mtDNA and the amount of this changed mtDNA exceeds a certain limit, the unchanged mtDNA can no longer keep up with normal cellular functions, and the disease starts showing symptoms.
In LHON, mitochondrial mutations affect genes that are part of the energy production chain. This results in the selective degeneration of nerves in our eyes (retinal ganglion cells) and can lead to optic atrophy (or loss of nerve fibers) within a year of disease onset. Three common mtDNA mutations account for about 90% of clinical cases in various and diversely ethnic families. These mutations are either absent or very infrequent in normal people.
Except in some rare cases, an mtDNA mutation will be present in all family members related to the mother of patients with LHON, although many of these people will never show symptoms. This implies, while the presence of an mtDNA mutation is required for the disease to manifest, it’s not always enough by itself. Since individuals at risk may have differing amounts of this mutated mtDNA in their optic nerves, it’s currently hypothesized that this variation may help explain why the disease presents differently in patients whose mitochondrial genotypes appear similar when tested via the blood.
Other genetic factors might influence how LHON presents itself. For example, some genes that control the expression of mitochondrial genes might play a role. Because LHON visual loss is more common in men, researchers have proposed the existence of a vision loss susceptibility gene on the X chromosome. Recent studies have identified a high-risk region on the X chromosome that’s associated with a dramatic increase in vision loss among patients with two specific LHON mutations.
Some researchers have proposed that factors related to the immune system might be involved, primarily to explain why LHON sometimes co-occurs with multiple sclerosis. However, studies have shown that the HLA-DR locus (a specific region on our genes) is not a major determinant for the development of visual loss.
Lastly, internal and external environmental factors may play a role. Things like systemic illnesses, poor nutrition, injuries, medications, or toxins that put stress on or interfere with mitochondrial metabolism have been suggested to influence how LHON presents itself.
Risk Factors and Frequency for Leber Hereditary Optic Neuropathy (LHON)
LHON, or Leber’s hereditary optic neuropathy, is considered the most common mitochondrial disease. The frequency of this disease varies, with rates being 1 in 27,000 in North East England and 1 in 45,000 in a study of the European population. It’s more often seen in males (80% to 90% of cases) and typically starts affecting people from ages 15 to 35.
- LHON is believed to be the most common mitochondrial disease.
- The occurrence of this disease may be 1 in 27,000 in North East England and 1 in 45,000 in Europe.
- This disease is more prevalent in males, accounting for 80% to 90% of cases.
- It usually starts to affect people when they are between 15 and 35 years old.
Signs and Symptoms of Leber Hereditary Optic Neuropathy (LHON)
Macular RGCs, which provide the axons for the papillomacular bundle and serve central vision, are typically affected first in cases of Leber’s Hereditary Optic Neuropathy (LHON). Patients typically report painless, central visual loss in one eye, which may come across as a foggy or faded vision. Usually, the other eye is affected weeks or months later, with 97% of patients experiencing this within a year.
Patients often experience a severe decline in their vision, with most deteriorating to visual acuities worse than 20/200. Colour vision also takes a hit, often early on in the disease, but usually after substantial vision loss. Compared to patients with other optic neuropathies, the pupillary light responses in LHON patients are usually preserved.
A typical characteristic of LHON is visual field defects which are often central or cecocentral. There may also be sudden appearances of scotoma, which is an area of partial alteration in the field of vision.
The illness has a few specific signs visible in the acutely inflamed eyes, such as dilation and tortuosity of the optic nerve head vessels, retinal and disc haemorrhages, implementation of exudates, and the obscuration of the disc margins. A triad of signs unique to LHON are a circumpapillary telangiectatic microangiopathy, nerve fiber layer swelling around the disc and absence of leakage from the disc on fluorescein angiography. As the disease progresses, the optic discs might not appear pale, which, coupled with the relatively preserved pupillary responses and lack of pain, may lead to misdiagnoses.
- Classic visual field defects (often central or cecocentral)
- Specific funduscopic abnormalities
- Sudden appearances of scotoma
- Specific triad of signs unique to LHON
Optical coherence tomography (OCT) and histopathology studies have exhibited a loss pattern in the retinal nerve fiber layer, which is useful in tracking disease progression. Typically, loss of macular RGCs occurs before the onset of clinical symptoms. The disease can be described in stages according to the timing of symptoms and clinical findings.
- The asymptomatic phase involves carriers of the mutation. During this time, the fundus examination may appear normal or present changes including vascular abnormalities, hyperemia of the optic disc, and retinal nerve fibre layer swelling.
- The subacute phase is marked by a deterioration in central visual acuity and the development of central scotoma. It generally starts within six months from the onset of symptoms, and it’s when most patients seek medical attention.
- The dynamic phase spans six months to one year from the onset of symptoms, with a plateau in visual fields and OCT measurements occurring about a year after the onset.
The progression towards visual loss may vary among patients, occurring either gradually or suddenly. The disease can present differently in children under 12 or in adults over 65. Though generally, vision impairment is the primary manifestation of LHON, some patients might also present with cardiac conduction abnormalities or minor neurological problems, and some may even showcase symptoms similar to multiple sclerosis.
Testing for Leber Hereditary Optic Neuropathy (LHON)
If your doctor suspects you have Leber’s Hereditary Optic Neuropathy (LHON), a type of vision loss, they will perform several tests. These include:
* Checking your clearness of vision (Visual acuity)
* Testing your ability to see colour (Color vision)
* An examination of the back of your eye (Fundus examination)
* A test to map the field of vision your eye can see (Visual field perimetry)
* A special imaging scan of your eye (OCT imaging)
For kids with the disease, the doctor checks the size of the optic disc (area where optic nerve enters the eye) using OCT imaging. A larger optic disc may mean a better chance of maintaining good vision. But in adults who show symptoms later in life, the doctor will consider whether exposure to toxins like cigarette smoke, alcohol, or environmental factors have had an impact.
They can also run tests to check the function of the optic nerve and the status of the retina. The visually evoked potential (VEP) is a test that measures the time it takes for your brain to respond to visual stimuli. The electroretinogram (ERG) is a test that measures the electrical response of the retinas (light-sensitive layers at the back of your eyes). Even if you’re not showing symptoms, these tests might show a slow response time or other changes that suggest LHON.
If there are any additional symptoms that aren’t related to the eye, an MRI of the brain might be recommended. Since LHON can sometimes cause abnormalities in heartbeat rhythms, an ECG (a test that measures the electrical activity of your heart) may be ordered. These tests help monitor the condition over the long term.
Treatment Options for Leber Hereditary Optic Neuropathy (LHON)
If you have a genetic condition known as LHON (Leber hereditary optic neuropathy), your doctor will strongly recommend certain lifestyle changes. These changes can help manage the condition and possibly reduce its symptoms. They include:
- Quitting smoking
- Avoiding excessive drinking of alcohol
- Reducing exposure to harmful chemicals like solvents and fumes
- Taking daily vitamin supplements
In 2017, a worldwide consensus statement – a document written by a group of leading medical experts – was published on how to treat and manage LHON. An important aspect of the statement was that your treatment should not be influenced by the predicted outcome of your condition. This means all patients should receive the best possible care and treatment, regardless of the severity of their condition.
Doctors may prescribe idebenone for patients with LHON, particularly if the disease is still developing. Idebenone is a man-made version of a natural substance called ubiquinone. It helps provide energy to cells and acts as an antioxidant, protecting cells from damage. The medication supports the function of mitochondria, which are the energy generators of cells.
If you are prescribed idebenone, you should start the medication as soon as possible and continue it for at least a year. This helps doctors see if the treatment is having any effect. Success with treatment would be defined as an improvement in visual sharpness and field of vision. If your doctor confirms a positive outcome from the treatment, they may recommend continuing it for another year.
In terms of follow-up visits, they are typically scheduled every 3 months for developing cases, then roughly every 6 months during the second year after the onset of the disease. After the second year, annual checkups are usually sufficient.
What else can Leber Hereditary Optic Neuropathy (LHON) be?
When doctors are trying to diagnose LHON, they need to consider other conditions that can cause similar symptoms. These include:
- Demyelinating optic neuritis, which is damage to the optic nerve due to loss of its protective covering
- Neuromyelitis optica spectrum disease, a group of conditions that cause inflammation and damage to the central nervous system
- Toxic optic neuropathy, damage to the optic nerve from harmful substances
- Compressive optic neuropathy, where pressure on the optic nerve damages it
- Maculopathies, which are diseases of the macula, the central part of the retina in the eye
- Nonorganic vision loss, which is vision loss that can’t be explained by physical damage to the eye or optic nerve
The doctor should take the patient’s history, consider their symptoms, and use imaging tests to tell the difference between LHON and these other possible explanations for the patient’s symptoms.
What to expect with Leber Hereditary Optic Neuropathy (LHON)
In most people with a condition called LHON, their loss of vision is usually severe and permanent. That said, some people may experience a gradual or sudden improvement in their vision over time, sometimes taking up to a decade after the initial eyesight problems start. Such an improvement might show up as a gradual clarity in central vision or a small area of clear vision surrounded by an area with impaired vision.
The chances for a better vision outcome are much higher if the condition begins at a young age. In fact, most patients who started experiencing symptoms before they turn 20 end up with a final vision that’s better than 20/80, which is somewhat below normal but still functional.
The specific type of genetic mutation a patient has can also affect how their vision fares over time. For instance, those with the 11778 mutation have the worst vision prognosis, with only 4% reporting spontaneous recovery. On the other hand, patients with the 14484 mutation have the best outcome, with 37% to 65% reporting spontaneous recovery. Generally, patients with the 14484 mutation find their vision to be significantly better than those with the 11778 and 3460 mutations.
It is rare, but in some instances, vision loss can reoccur in patients, whether they’ve experienced visual recovery or not.
Possible Complications When Diagnosed with Leber Hereditary Optic Neuropathy (LHON)
Most people suffering from LHON (Leber’s hereditary optic neuropathy) will experience optic atrophy, or damage to the optic nerve, within a year. This typically results in serious vision loss during their active years of life, and sadly, this damage is irreversible.
The potential for improvement in vision largely depends on what mutation the patient has. Unfortunately, the G11778A mutation often has the worst outcome overall. However, some good news is that those with the T14484C mutation have a chance at seeing some improvement if their vision loss started before they turned 20.
- Damage to the optic nerve in LHON patients
- Uncorrectable vision loss during the patient’s active years
- Variation in vision outlook depends on the specific mutation
- G11778A mutation generally has a poor prognosis
- Possible vision improvement for T14484C patients if vision loss starts before 20 years old
Preventing Leber Hereditary Optic Neuropathy (LHON)
LHON stands for Leber’s hereditary optic neuropathy, which is a disease that’s passed down through families and causes loss of vision. The severity and symptoms can vary based on the specific type of genetic mutation, environmental factors, and exposure to harmful substances. Patients who potentially carry this disease but don’t have any symptoms should maintain a healthy diet and add vitamins B1, B2 and B12 into their diets. It’s also important to avoid consuming large amounts of alcohol in a short time and avoid tobacco, as these can put extra stress on the mitochondria (the powerhouse of cells) and further damage vision.
If symptoms begin to show, taking a medication called idebenone, a type of quinone drug, along with continued vitamin supplements can increase the chances of getting better vision. When a person is diagnosed with LHON, it would be beneficial for their family members to also get genetic counseling and testing to determine whether they have inherited the same mutation, also known as the proband. This can help prepare them and provide early interventions if needed.