What is Macular Degeneration?
Age-related macular degeneration (ARMD) is the leading reason for vision loss in developed countries, especially in individuals over 60 years old. This condition affects the middle part of the retina known as the fovea, which is responsible for sharp, central vision. As a result, it can make activities like reading or driving difficult. In fact, ARMD is responsible for 8.7% of all cases of blindness worldwide.
What Causes Macular Degeneration?
There are different factors that can increase the risk of getting age-related macular degeneration (ARMD), a disease that affects the eyes. These factors include things related to our lifestyle, age, hormonal changes, inflammation, genetic makeup, and our cardiovascular health.
Age, gender, race, and economic background are all factors. The disease is found to be more likely in older people, and women seem to be at a higher risk. It’s also more common in non-Hispanic white people compared to black and Hispanic people. However, factors like education, income, job status, or marital status don’t seem to have an effect on how likely someone is to get the disease.
Smoking increases the risk of ARMD. But drinking alcohol is not linked to the condition. The role of obesity and physical activity is still unclear. Certain vitamins and zinc supplements have been found to reduce the risk of the disease and prevent vision loss.
When it comes to heart health, research has found a weak-to-moderate link between high blood pressure and ARMD, and hardened arteries might increase the risk of the disease. There is no solid link between cholesterol levels and ARMD. More research is needed to understand how good cholesterol (HDL) is related to ARMD.There’s not a strong connection between diabetes and the condition.
Hormone replacement therapy, a treatment for symptoms of menopause, might have a protective effect. Research also suggests that inflammation and one’s genetic makeup might play a role in ARMD. Certain variants in several genes related to the immune system are associated with the disease.
Risk Factors and Frequency for Macular Degeneration
By 2020, it’s expected that around 196 million people will be affected by this disease, with the number predicted to rise to 288 million by 2040. There’s a notable difference in who gets the disease early on: people of European descent are more likely to get early AMD than Asians. However, when it comes to late-stage AMD, both groups have the same prevalence. In 2015, AMD was the fourth leading cause of blindness worldwide, and also the third leading cause of substantial visual impairment. It’s clear that the global impact of AMD is becoming increasingly important.
Signs and Symptoms of Macular Degeneration
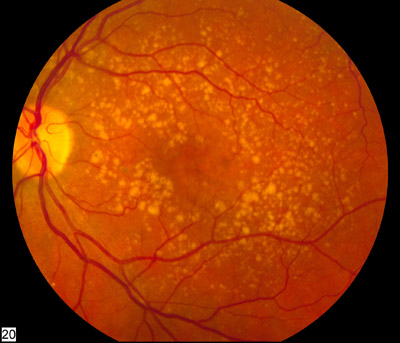
Age-related macular degeneration, or ARMD, is an eye condition that can be classified in two ways: dry or non-neovascular, and wet or neovascular. People with this condition experience gradual vision loss, especially in the early or intermediate dry stage. Those with ARMD will have yellowish deposits (drusen) or changes in their retinal pigment epithelium (RPE), which is a layer at the back of the eye. Their condition may worsen when these drusen combine, create larger deposits, and cause the RPE to detach. In the advanced stage, known as Geographic atrophy, there is significant vision loss when the center of the macula is involved.
ARMD can be staged into four groups depending on the patient’s condition:
- Group 1 (no ARMD): no drusen or 5–15 small drusen (less than 63 microns in diameter) and no other ARMD signs.
- Group 2 (early-stage ARMD): more than 15 small drusen or less than 20 medium-sized drusen (63-124 microns in diameter) with pigment changes, but not geographic atrophy.
- Group 3 (intermediate stage): at least one large druse (over 125 microns in diameter), or many medium-sized drusen and non-central geographic atrophy (atrophy not affecting the fovea).
- Group 4 (advanced stage): central geographic atrophy affecting the fovea or presence of neovascular ARMD.
Geographic Atrophy, the advanced form of dry ARMD, is an area of the eye that lacks RPE and has visible underlying blood vessels. It is known to enlarge over time and may affect both eyes. Those with one affected eye may risk developing the wet form of ARMD in the other. Signs of progress to Geographic Atrophy include large drusen, combined drusen and changes to the pigment overlying the area of drusen.
The wet form of ARMD, or neovascular ARMD, is recognized by the growth of abnormal blood vessels from a thin membrane at the back of the eye (choroidal neovascular membrane or CNVM). This leads to fluid or blood accumulating under the RPE and disturbing the normal function of the eye. Patients may experience blurred vision, distortion in vision or other vision changes.
On an eye examination, different types of pigment epithelial detachments (PEDs) can be seen. Below the RPE, a CNVM can be found. Types of PEDs include serous (smooth, well-defined dome-shaped RPE elevation), fibrovascular (irregular elevation of the RPE), and drusenoid (RPE detachment caused by soft drusens). A fourth type, hemorrhagic PED, is characterized by blood underneath the RPE.
Testing for Macular Degeneration
Dry age-related macular degeneration (ARMD) and neovascular ARMD are health conditions that can affect your eyesight. To better understand what’s happening in your eyes, medical professionals use various types of imaging to get a closer look.
For dry ARMD, here are some of the methods that doctors can use:
Fundus Fluorescein Angiography (FFA): This is a test that uses a special dye to map the blood flow in your eye. In this case, the dye will highlight certain parts of the eye called drusen. The technique can also show areas of your eye where tissue has worn away.
Indocyanine Green Angiography (ICGA): This is another dye method where the dye becomes more noticeable in the eye a few minutes after being used. This technique can distinguish between hard and soft drusens in your eye. The hard drusen will become more vibrant, while soft drusen typically stay the same color or become darker.
Autofluorescence: This test helps evaluate cells in your eyes that are vital for healthy vision. It helps define areas where tissue has worn away. The worn-away areas appear darker on the test, while their borders may be slightly brighter. If a bright border appears, this could tell your doctor that the worn-away area is getting larger. This technique is highly sensitive and can catch these changes sooner than a regular eye test.
Optical coherence tomography (OCT): This technique uses light waves to get cross-sections of your eyes. The OCT reveals little bumps in your eye called ‘drusen.’ And, the more drusen, the greater your risk for ARMD. OCT can measure this drusen. The OCT can also show areas where tissue has worn away.
For neovascular ARMD, similar techniques are applied:
Fundus Fluorescein Angiography (FFA) & Indocyanine green angiography (ICGA): These dye techniques are also used in neovascular ARMD. Depending on the type of eye changes your doctor is looking for, the dye will act differently. It can show anything from bright spots that persist during the test to darkness due to blood interference.
Optical coherence tomography (OCT): OCT is a useful tool in tracking and monitoring neovascular ARMD. It helps classify a certain type of abnormal blood vessel growth beneath or above a special part of your eye called RPE. This scan can help your doctor monitor your disease progress and the effectiveness of your treatment by showing changes in the amount of fluid in your eye.
These imaging techniques are crucial for accurate diagnoses and effective treatments in dealing with ARMD. They allow doctors to see details within the eye that would not be visible otherwise and help in monitoring eye health.
Treatment Options for Macular Degeneration
Patients with dry Age-Related Macular Degeneration (ARMD) need regular check-ups to spot any signs of the disease progressing to a more advanced stage. If you have early ARMD in both eyes, you probably won’t need to have any treatment quite yet. There’s no proof that taking dietary supplements full of antioxidants and minerals can help prevent early ARMD from progressing to a more advanced stage. However, it’s important for these patients to have check-ups every year to see if the disease has progressed to intermediate ARMD. If you have intermediate ARMD, or advanced ARMD in one or both eyes, you might want to consider starting a dietary supplement regimen. This is based on recommendations from the Age-Related Eye Disease Study (AREDS).
AREDS have put together a dietary supplement regimen that includes daily doses of vitamin C, vitamin E, zinc oxide, copper oxide, lutein, zeaxanthin and omega -3 fatty acids. Originally, this regimen also included beta carotene, but it was removed because it may increase the risk of lung cancer in smokers. Macular pigments lutein and zeaxanthin have the potential to reduce the risk of the disease getting worse.
Now let’s talk about treatment for Neovascular ARMD. This can be treated with Laser Photocoagulation if the lesion is safely away from the central area of the retina (the fovea). However, this treatment has fallen out of favor because the results have been poor and there is a high chance of the disease coming back.
Photodynamic Therapy is another treatment that was introduced in 2000. This treatment involves injecting a special dye (verteporfin) and using light to cause a reaction in the targeted area. This slows down the growth of abnormal blood vessels but doesn’t improve vision greatly.
Antiangiogenic Therapy is a treatment that targets and blocks the action of a protein, known as vascular endothelial growth factor (VEGF), that promotes the growth of these abnormal blood vessels. The first treatment of this kind to be approved was pegaptanib, followed by ranibizumab, bevacizumab, and aflibercept. These treatments have been shown to reduce the growth of these abnormal blood vessels and can help with the reduction of swelling. There are various treatment regimens, and the one you may follow can depend on different factors like the progress of the disease and the recurrence of fluid.
Two other treatments that are used in rare cases are surgery to displace blood that is underneath the retina and intravitreal injections. These treatments may be considered when the disease has progressed significantly and other non-invasive treatments have failed. However, even with the use of these treatments, a significant number of patients can ultimately go blind. In these cases, using devices to aid low vision can be very effective.
What else can Macular Degeneration be?
Reticular pseudodrusen are deposits that occur above a specific layer of the retina, and they need to be distinguished from other deposits called drusen. These are found on a different level of the retina.
Additionally, dry Age-Related Macular Degeneration (ARM), which affects the central part of the retina, can show similar features to adult vitelliform macular dystrophy and drug-induced retinal toxicity. In adult vitelliform dystrophy, there are yellow deposits below the retina. However, if certain drugs, such as hydroxychloroquine, deferoxamine, and cisplatin, cause retinal damage, they can mimic the appearance of dry ARM.
Doctors also need to differentiate Neovascular AMD, another type of macular degeneration, from conditions like retinal angiomatous proliferation and Polypoidal Choroidal Vasculopathy (PCV). In retinal angiomatous proliferation, new blood vessels start to form within the retina and grow towards other layers. This condition can be identified through a fluorescein angiography, a type of medical imaging, which shows a retinal vessel dipping into the new blood vessel growth, indicating an connection between the retina and the new blood vessels.
Polypoidal Choroidal Vasculopathy can be identified during an eye examination by the appearance of orangish nodules along with a buildup of blood or fluid under the retina. An OCT scan can show enlarged blood vessels in these cases. The retina in Polypoidal Choroidal Vasculopathy is thicker, unlike in Age-Related Macular Degeneration where it is thinner. An Indocyanine Green Angiography (ICGA) shows polyps, which are bulging or swelling of blood vessels, and these are diagnostic indicators of PCV.