What is Malignant Eyelid Lesions?
Cancerous lumps on the eyelid can be spotted by eye specialists, general practitioners, or skin doctors during a regular check-up. The most common types of cancer found on the eyelid are basal cell carcinoma, squamous cell carcinoma, sebaceous cell carcinoma, melanoma, and Merkel cell carcinoma. There are more types of eyelid cancers, but they are less common and are not discussed in this article.
It’s important to remember that any type of skin cancer can appear in the area around the eye. Doctors should check each new patient thoroughly, asking about their health background and doing a physical exam. They should ask about things that might increase the chances of getting skin cancer, how long the lump has been there, how fast it’s grown, and whether it’s sore, leaking fluid, or bleeding. The doctor should also look at the lump carefully. If a patient has had skin cancer before, spent lots of time in the sun, or has sores that won’t heal or keep coming back, the doctor should consider the possibility of skin cancer around the eye.
Doctors can get a better look at any suspicious lumps by using special equipment like a slit-lamp or a dermoscope. A dermoscope is a device that can help to avoid unnecessary operations. If the doctor thinks the lump could be cancer, they should refer the patient for a biopsy. This is a procedure where a small piece of the lump is removed and looked at under a microscope to see if it’s cancerous. Then, if needed, treatment can be started. This could include surgery to remove the lump, radiation therapy, chemotherapy, immunotherapy, cryosurgery (freezing the tumor), or laser treatments.
What Causes Malignant Eyelid Lesions?
Actinic Keratosis, or AK, also known as solar keratosis, usually develops due to prolonged exposure to ultraviolet (UV) rays. Other factors that may increase the risk include being male, older age, baldness, and having had skin cancers such as melanoma or squamous cell carcinoma. These skin lesions usually show up on areas frequently exposed to the sun like the hands, shoulders, and face. They can appear as single or multiple lesions and usually have yellow/brown scales on top. The skin around may show signs of sun damage like blood vessel enlargement (telangiectasias) and yellow discoloration.
Basal Cell Carcinoma (BCC), the most common type of skin cancer in the world, happens most frequently on the face and neck. In some cases, BCC can also affect the eyelids. Studies have suggested that a significant number of squamous cell carcinomas and basal cell carcinomas can develop from previously diagnosed Actinic Keratoses. There are certain medical conditions that might increase the risk of developing BCCs such as Sturge Weber/Port-wine stain, or syndromes such as Basal Cell Nevus Syndrome, Gorlin-Goltz, Rombo, Bazex-Dupré-Christol, and Xeroderma Pigmentosum.
Squamous Cell Carcinoma (SCC) of the eyelid is a result of abnormal growth of skin cells. Factors such as extended exposure to UV radiation, old age, exposure to arsenic, Human Papilloma Virus (HPV) infection, and HIV infection could contribute to its development. Keratoacanthomas (KA), a variant of SCC, and Actinic Keratoses, precancerous lesions, are related to SCC. Conditions that could make a person more liable to developing KA/SCC include Oculocutaneous albinism, Epidermolysis bullosa, Fanconi anemia, Ferguson-Smith, Muir-Torre syndrome, Mibelli-type porokeratosis, Rothmund-Thomson syndrome, Keratitis-ichthyosis-deafness syndrome, Bloom syndrome, Epidermodysplasia verruciformis, and Xeroderma pigmentosum.
Sebaceous Carcinoma (SC) of the eyelid commonly appears as a yellow, painless mass on the eyelid margin, originating from the sebaceous (oil-secreting) glands like the meibomian glands or glands of Zeis. They may look like a chalazion or hordeolum (styes), but the clinical history might indicate otherwise.
Eyelid melanoma is similar to skin melanoma. Risk factors include excessive sun exposure, presence of abnormal moles, a personal history of melanoma, older age, and light skin types. Certain conditions can also predispose individuals to develop eyelid melanomas such as Familial atypical multiple mole melanoma syndrome, Familial melanoma, and Xeroderma Pigmentosum.
Merkel Cell Carcinoma (MCC) was originally thought to originate from Merkel cells, which are receptor cells in the skin. But it’s now understood to stem from epithelial skin cells and neuroendocrine cells. Polyomaviruses, a type of virus, have also been linked to the development of MCC.
Risk Factors and Frequency for Malignant Eyelid Lesions
Various studies have looked at the types and frequencies of eyelid lesions. In one study, it was found that 59% were skin cell related, 1.5% were cancerous, and 6% were identified as having the potential to turn into cancer, like actinic keratosis or Bowen’s disease. Basal cell carcinoma, a type of skin cancer, appeared in the majority of the cancerous lesions (95%). Other cancers, like squamous cell carcinoma, were much less common (5%), and there were no instances of sebaceous cell carcinoma.
Another study found similar results with most eyelid tumors benign (85.7%) and a smaller number identified as having the potential to become cancer (1.1%). There were also malignant lesions, which are cancer cells (13.1%). Of these cancerous lesions, 60% originated from skin cells and 34.6% from gland cells. The most common types of cancer were basal cell carcinomas (56.5%) and sebaceous carcinoma (34.6%), with smaller instances of squamous cell carcinomas (3.8%) and lymphoma or plasmacytoma (1.7%).
Actinic keratosis, a skin condition that can lead to skin cancer, is quite common. Between 1990 and 1994, it was the reason for 14% of all dermatology visits. In 2004, approximately 40 million people in the United States were affected by it. However, the prevalence of actinic keratosis can vary from country to country.
Risk factors for developing actinic keratosis include being male, having a lot of sun exposure over time, being older, being bald, having a history of melanoma or squamous cell carcinoma, and having fair skin.
Basal cell carcinoma, a type of skin cancer, is the most common sort of cancer in the eyelid in the U.S. and Western countries. In India, basal cell carcinoma is the second most common after sebaceous carcinoma.
Squamous cell carcinoma, another type of skin cancer, is typically found in patients over 50, but can occur at any age. It is the second most common cancer of the eyelid after basal cell carcinoma in the U.S. and Western countries. In India, squamous cell carcinoma is the third most common after sebaceous and basal cell carcinoma. It is also common after organ transplantation due to the diminished ability of the immune system to fight off cancer cells.
- Sebaceous carcinoma generally appears in people around 65.2 years old, with a higher prevalence in females.
- Melanoma is a type of skin cancer that rarely appears on eyelids (around 2% of melanoma cases). It’s more common in females than males.
- Merkel cell carcinoma is a rare type of skin cancer that specifically affects older white patients. However, it can also occur in younger patients who have had organ transplants or who have HIV/AIDS.
- Lentigo maligna, a condition that can turn into skin cancer, is not well-studied in areas around the eyes. It requires a team of healthcare professionals for proper management.
Signs and Symptoms of Malignant Eyelid Lesions
A medical examination starts with taking a patient’s history, which covers a range of topics such as personal or family history of skin or other cancers, any history of compromised immune system, radiation therapy, or fair skin. Doctors should also keep details about excessive sunlight exposure and any persistent or recurring skin issues on record.
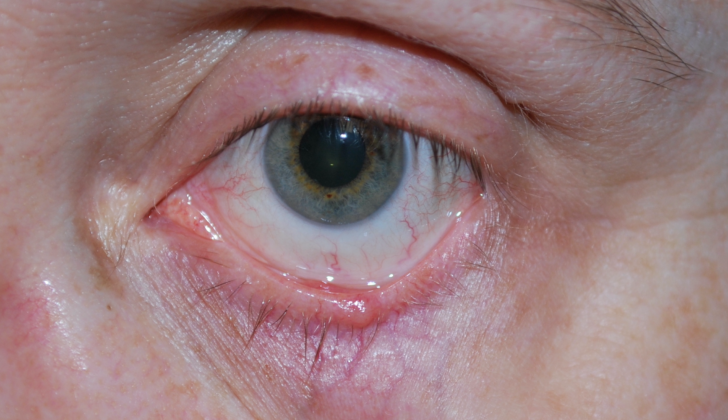
Doctors should ask patients about any unusual characteristics of eyelid lesions, including itching, bleeding, ulceration, blistering, chronicity, change in color, change in size, and loss of typical eyelid architecture such as the loss of eyelashes.
Physicians should also ask about details like the location, onset, nature, and duration of eyelid lesions, as well as any previous treatments or recurrence of these lesions. Examinations of the eyelid and surrounding tissues should be conducted in rooms with sufficient lighting, using aids like a dermatoscope, slit lamp, or pocket flashlight if needed. Physicians should observe the patient’s skin type and note any significant difference in skin tone between sun-exposed and sun-protected areas.
During the clinical examination, doctors should look for lesions showing irregular pigmentation, ulceration with scabs or bleeding, dilated blood vessels, or the loss of eyelashes or skin wrinkles.
Using magnification equipment such as a slit-lamp or dermatoscope can help get a clearer picture of the lesion. Each suspicious lesion should be measured in both vertical and horizontal dimensions in millimeters. Also, touching the edges of the lesion helps to check if it is affecting or attached to deeper tissues.
Turning the lower lid inside out (everting) and double turning the upper lid is important to check the involvement of the conjunctival and the creases of the eye. Lymph nodes in areas like in front of and behind the ear, along the jaw, and under the chin should be checked for swelling (lymphadenopathy). Doctors should take a photograph of the lesion to record how it looks.
If any suspicious eyelid lesion is found, the patient should be referred to a skin specialist for a full-body dermatologic examination. Detecting one skin cancer can often signal the likelihood of having other pre-cancerous or cancerous lesions elsewhere on the body.
Testing for Malignant Eyelid Lesions
When a healthcare provider is examining a potentially cancerous growth on the eyelid, they consider many factors. These include how fast the growth has developed, whether it causes pain, and how it has affected your eye health and vision. They will check your vision quality, color perception, eye movements, pupil reactions, and visual field (the total area you can see without moving your eyes).
These results could be influenced by conditions affecting your eye, eye socket, the tissues around your eye, and your eyelid. In particular, when checking the growth on your eyelid, they will note:
– The color of the growth(s)
– The size of the growth, including its width, height, and possibly depth
– If there are unusually twisted or enlarged blood vessels (telangiectasic or atypical vasculature) in or around the growth
– If the shape of your eyelid has changes
– If the growth involves the inner lining of the eyelid (palpebral conjunctiva) – they might turn your upper eyelid inside out to check the back surface of the eyelid (conjunctival fornix)
– Loss of eyelashes in the area (madarosis)
– Sores or breaks on the surface (ulceration)
– Whitening of your eyelashes (poliosis)
– Swollen lymph nodes nearby
It’s crucial that they work closely with a laboratory professional when collecting a sample from your eyelid for testing. This ensures that they get useful information to diagnose your condition quickly and accurately. They might remove a full-thickness portion of the growth for examination in the laboratory before starting treatment for cancerous growths. Furthermore, they will also consider the possibility that cancer could have spread from somewhere else to your eyelid.
To get a better understanding of how the growth affects your eye and the space around it, they may arrange for you to have imaging tests such as a magnetic resonance imaging (MRI) scan and a computerized tomography (CT) scan. An MRI scan can provide detailed images of the soft tissues around your eye, while a CT scan helps evaluate the bone structure. Both these tests are valuable for planning your treatment.
Treatment Options for Malignant Eyelid Lesions
Actinic Keratosis (AK) is a skin condition that may resolve on its own, but because it may turn into cancer, doctors usually opt for treatment. When the condition is present near the eye, the most common treatment for small AKs is local excision, a minor surgical procedure to remove the affected area. Other possible treatments, including freezing (cryotherapy), topical chemotherapy, light therapy (photodynamic therapy), and laser therapy, are also considered. However, these should be carefully used and are generally recommended in consultation with an eye specialist.
Basal Cell Carcinoma (BCC) is a type of skin cancer that commonly affects the eyelids. The primary method of treatment for BCC of the eyelid is surgical removal. Generally, a special surgical procedure called Mohs micrographic surgery or a local excision is used for removal. After removal, the surgical wound is then repaired. There has been some success with using a medication called vismodegib to shrink the tumor before surgery and help avoid excessively invasive surgical procedures. A notable study known as the SINS trial found that surgery was more effective than imiquimod, a topical medication, for treating BCC, though it also suggested the drug might be beneficial in selected cases.
Squamous Cell Carcinoma (SCC) and Keratoacanthoma (KA) are often difficult to differentiate and hence, usually, a biopsy is performed. The primary treatment for SCC, once confirmed, is surgical removal, often using the Mohs micrographic surgery. The wound left by the surgery is then repaired. If there is evidence that the SCC has spread into the orbit (the eye socket), further treatments such as presurgical (neoadjuvant) treatment and surgical removal of the eyeball (orbital exenteration) might have to be considered. There have been some cases where radiation has been used as a treatment option when surgical removal is not feasible. Some drugs that specially target cancer cells have shown some promising results for when surgical management is not possible.
The treatment and management of Sebaceous Carcinoma (SC) are not fully agreed upon, however, guidelines have been proposed. A complete skin examination and an examination of adjacent lymph nodes should be performed. Based on certain factors, genetic testing might be done as well. The tumor can then be treated with a certain type of surgery, such as Mohs micrographic surgery, or by complete removal with a wide excision. If the tumor has invaded the orbit, it might require orbital exenteration or radiation therapy.
The primary treatment for localized melanoma is the wide removal of the skin. There are various suggested safety margins based on the thickness of the melanoma. Sentinel lymph node biopsy might be performed, which can provide valuable information regarding the prognosis. For patients with metastatic melanoma, surgical removal is not curing; instead, treatments like chemotherapies and immunotherapies are more commonly used.
Merkel Cell Carcinoma (MCC) is a highly aggressive skin cancer type. Possible treatments include surgical excision, radiation therapy, chemotherapy, and immunotherapy. Given the radiosensitivity of these tumors, radiotherapy might be particularly effective. Chemotherapy works well as a first line of treatment for metastatic MCC when the disease has spread or is local. Immune checkpoint inhibitors are newly added treatments and show promise in treating MCC.
After successful surgical removal, patients should be advised on proper sun protection, which includes sunscreen, UV-blocking sunglasses, wide-brimmed hats, long sleeve clothing, and other protective clothing, as well limiting sun exposure, especially in the middle of the day.
What else can Malignant Eyelid Lesions be?
When looking at the different types of eyelid tissue, doctors will consider various potential conditions in their diagnosis. The conditions can be grouped according to three types of cells: epithelial cells, melanocytes, and adnexal structures like sweat glands and hair follicles.
In the category of epithelial cells, the following conditions can be pre-cancerous or malignant:
- Pre-malignant Lesions
- Actinic or solar keratosis
- Seborrheic keratosis
- Keratoacanthoma
- Cutaneous horn
- Malignant Lesions
- Bowen disease (Stage 0, non-spreading cancer)
- Basal cell carcinoma
- Squamous cell carcinoma
- Merkel cell carcinoma
Next are the melanocytes, which can also have pre-malignant and malignant conditions:
- Pre-malignant Lesions
- Dysplastic nevus
- Large congenital nevi (skin marks larger than 20 cm, which have a 4% to 20% chance of becoming malignant)
- Blue nevus variants, which can potentially turn malignant
- Oculodermal melanocytosis, which needs monitoring every six months as it can lead to glaucoma or melanoma of the skin, iris, and choroid
- Malignant Lesions
- Melanoma
Finally, there are conditions associated with the adnexal structures, which can also become malignant:
- Adnexal Lesions
- Malignant hair follicle tumor (a type of BCC)
- Sweat Glands
- Malignant syringoma
- Mucinous sweat gland adenocarcinoma
- Gland of Moll adenosarcoma
- Sebaceous Glands
- Sebaceous carcinoma
What to expect with Malignant Eyelid Lesions
The outlook for a skin tumor depends largely on its type and stage. Here’s a brief summary of the prognosis for each type:
Actinic Keratosis (AK) doesn’t affect lifespan but can turn into cancer. It’s especially concerning if it exhibits signs of progression like sores, rapid growth, size of more than 1 cm, and inflammation. A good number of AKs (between 21% and 70%) improve on their own. But, having AK increases your risk for skin cancer six times.
Basal Cell Carcinoma (BCC) often appears on the lower lid (50% of cases), the medial canthus (30% of cases – this is the inner corner of the eye), upper lid (15% of cases), and the lateral canthus (5% of cases – outer corner of the eye). It generally has an excellent prognosis with a 95% cure rate and a yearly recurrence rate of 1% to 5% after surgical removal. However, those with BCC linked to Gorlin syndrome have a lifelong risk of multiple BCCs.
Squamous Cell Carcinoma (SCC) usually occurs on the lower lid (60.8% of cases), followed by the medial canthus (17.6%), lateral canthus (11.8%), and upper lid (9.8%). It tends to be more aggressive than BCC. But, with clean surgical margins, the mortality rate is good. Yet, there’s still a substantial risk of complications.
Sebaceous Carcinoma (SC) often gets misdiagnosed, contributing to a poor prognosis. In one study, nearly 60% of SC patients had about a 14.7-months delay in diagnosis. Some common misdiagnoses include chalazion and blepharitis. This misdiagnosis has previously led to a mortality rate of up to 50%, but it’s now between 4% to 11%.
Melanoma often results in a higher mortality rate if it occurs on eyelids or caruncle (the pinkish raised area in the corner of the eye). Prognosis also depends on the depth and extent of the tumor, as determined by several grading systems. According to a study in 2021, the 5-year survival rate for eyelid melanoma is 88.6% if it’s only on the skin surface and 77.1% if it has invaded deeper. Older age, more advanced staging, and lymph node involvement all point to a poorer outlook.
The prognosis for Merkel Cell Carcinoma (MCC) of the eyelid is generally poor, with mortality rates of 33% to 46%. Some factors linked to a poorer prognosis include being male, having a weakened immune system, a tumor size of between 2 cm and 5 cm, nodal metastasis (spreading of cancer to lymph nodes), and older age. About 10% to 30% of MCCs metastasize, or spread, to distant sites, like lymph nodes, bone, brain, liver, and lung.
Possible Complications When Diagnosed with Malignant Eyelid Lesions
If a medical condition is not diagnosed correctly, this might lead to the issue becoming more severe, as it continues to grow. This misdiagnosis can also result in the spread of the disease through the nerves, bloodstream, or lymphatic system. Additionally, complications can arise from surgery near the eye or from radiotherapy, each carrying various risks. These include:
- Difficulty in complete eye closure (lagophthalmos)
- Adhesion of the eyelid to the eyeball (symblepharon)
- Pullback of the eyelid (eyelid retraction)
- Drooping of the eyelid (ptosis)
- Outward turning of the eyelid rim (ectropion)
- Inward turning of the eyelid rim (entropion)
- Eyelashes growing towards the eye (trichiasis)
- Dry eye syndrome due to exposure, lack of aqueous fluid, or evaporation
- Damage to the tear drain system (nasolacrimal system)
- Double vision (diplopia)
- Injury to the eyeball and surrounding structures
- Bleeding in the eye socket (orbital hemorrhage)
- Infections
- Difficulty in healing tissues (especially with radiotherapy)
- Aesthetically displeasing outcomes
- Emotional distress
Considering treatments involving the body’s immune system or chemotherapy also carry further specific complications, so it’s crucial that doctors collaborate closely with cancer specialists and pharmacists when contemplating these treatment paths.
Preventing Malignant Eyelid Lesions
During every medical visit, doctors should remind patients about the steps they can take to lower their chances of developing eyelid cancer. The two main factors that can be controlled are protecting the skin against sun damage and avoiding nicotine or quitting smoking. Sunrays, particularly the short-wavelength UVB rays, are more harmful than long-wavelength UVA rays. They can harm the DNA in genes that usually suppress tumour growth. Research indicates that exposure to UV rays contributes to around 65% of melanoma (a serious skin cancer) and 90% of other skin cancers.
To protect against sun exposure, patients should avoid spending too much time under the sun, wear wide-brimmed hats to shield the head and neck, keep away from tanning salons, and use sunscreen lotion with a suitable SPF. Quitting smoking or avoiding nicotine is also advised, as it increases the risk of cancers. Additionally, patients who have a family history of skin cancers, a weakened immune system, previous radiotherapy, or exposure to harmful substances have a higher risk of developing skin cancers.