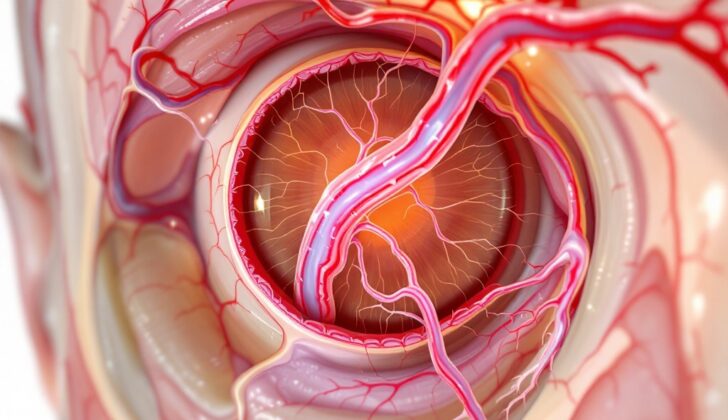
What is Orbital Vascular Anomalies?
Orbital vascular anomalies (OVAs) are a range of abnormal blood vessel conditions found in the eye socket area. The eye socket’s intricate structure, the changing nature of these conditions, differing symptoms among each type, and limited knowledge of how these conditions progress over time, make OVAs difficult to manage. A detailed examination, the use of specific imaging tests (like an MRI or CT scan), and a calculated step-by-step strategy are all important in correctly identifying these anomalies and deciding the best course of treatment.
What Causes Orbital Vascular Anomalies?
Over time, experts have developed several systems to classify different kinds of blood vessel discrepancies.
In 1982, Mulliken and Glowacki arranged these discrepancies into two main categories: hemangiomas and vascular malformations.
Hemangiomas are growths that develop when cells in blood vessel walls divide more than they should. They can be separated into two stages. The first, called the proliferative phase, is when these growths rapidly increase in size during early infancy, thanks to quick cell division. The second stage, known as the involuting phase, sees these growths slow their growth and ultimately reduce in size.
Vascular malformations are abnormalities in the structure of the blood vessels where the vessels aren’t dividing too quickly which makes them different from hemangiomas. They consist of abnormal versions of different types of vessels, namely capillary, venous, lymphatic, and arterial, either mixed together or isolated.
In 1999, the Orbital Society proposed another system. This system classifies these issues based on the direction and speed of blood flow: no flow, venous flow (blood returns to the heart), or arterial flow (blood flows away from the heart).
Further classification led to the development of Rootman’s Hemodynamic Model of Orbital Vascular Malformations. This model takes into consideration the nature of the blood flow and the connections to the venous system. This helps doctors decide the course of treatment which could include surgical glue or other specialized procedures to achieve the safest and most predictable results.
Fast-forward to 2014, the International Society for the Study of Vascular Anomalies (ISSVA) introduced a new classification system. This system uses the latest technology and advancements to group vascular lesions based on factors like clinical features, blood flow properties, and characteristics seen on imaging tests. This was later updated in 2018 to include more biological and genetic insights.
According to this system, orbital vascular anomalies – issues in the blood vessels around the eye- are grouped into two categories: vasoproliferative tumors and malformations.
Vasoproliferative tumors can be benign (non-cancerous), locally aggressive, or malignant (cancerous). Benign examples include infantile and congenital hemangiomas. Locally aggressive tumors include hemangioendothelioma and Kaposi sarcoma while malignant examples include angiosarcoma and the epithelioid variant of hemangioendothelioma.
Vascular malformations are either simple or mixed. Simple malformations can be related to capillaries, veins, lymph vessels, or arteries, while when mixed, two or more types of vessel components could be found in a single growth.
It’s important to note that terms like “cavernous hemangioma” and “lymphangioma” should be avoided. They are not true tumors, but vascular malformations. Today, they are known as Venous-Lymphatic Malformations (VLMs) and Solitary, Encapsulated Venous Malformations respectively. Additionally, terms like “orbital varix” and “capillary hemangioma” are being phased out for accuracy.
Schobinger introduced a clinical staging system for arteriovenous malformations in 1990. This system divides the malformations into four stages, each with characteristic features like color, pulsations, ulceration, bleeding, skin changes, and effects on the heart.
Lastly, there are anomalies that affect major named vessels, sometimes referred to as “channel type” or “truncal” vascular malformations, and syndromic malformations, that are part of conditions like Klippel-Trenaunay syndrome and Sturge-Weber syndrome.
Risk Factors and Frequency for Orbital Vascular Anomalies
Orbital Vascular Anomalies or OVAs, which are irregularities in the blood vessels in and around the eyes, make up roughly 10% of eye-related medical conditions. One study in 2011 suggested that a quarter of all lumps in the orbital region were from these ‘vasculogenic’, or blood vessel-related, conditions, while another study found the incidence to be 12%. It’s important to note that these studies didn’t use the most recent guidelines, which could mean they underestimated how common OVAs are. So, there’s a theory that OVAs might be the most common issue found in the area around the eye.
The reason why the various types of OVAs affect different genders in different ways is not yet understood. For example, infantile hemangioma (IH), a type of OVA common in children, is five times more common in girls than boys. But congenital hemangioma (CH), another type of OVA, affects both genders equally. Other risk factors for IH include being born prematurely, having a low birth weight, and a family history of the condition.
- Cavernous venous malformations (CVMs), the most common eye-related benign (non-cancerous) lesions in adults, most often occur in middle-aged women (20 to 40 years old).
- In contrast, distensible orbital venous malformations, another type of OVA, affect both genders equally.
Signs and Symptoms of Orbital Vascular Anomalies
Hemangiomas are common vascular tumors that often appear in infants and children, primarily in the area of the head and neck. They can be present at birth or develop within the first couple of weeks of an infant’s life. These tumors undergo two primary phases. The first phase involves rapid growth over 6-12 months, during which the tumor appears as a raised, red, rubber-like lump, similar to a strawberry. Following this, the tumor enters a slower growth phase that can last up to 5-9 years, which results in the tumor changing in appearance, showing signs of scarring, wrinkling, or discolored blood vessels.
The hemangiomas that are present at birth, known as congenital hemangiomas, do not follow this two-phase pattern and are less likely to regress on their own. Some types of these congenital hemangiomas may grow and disappear within the first 1-1.5 years of life, while others may continue to grow in line with the child’s growth.
Orbital venous malformations are another type of vascular disorder that can occur in the eye. These malformations can either be flexible (distensible) or rigid (non-distensible). According to a recent classification, these malformations can be categorized into three types, based on their behavior:
- Type 1: Low-flow, non-distensible malformations, often appearing in the middle third of the orbit. Symptoms can include blurry vision, pain, and balance issues in the eyes, which could even affect vision.
- Type 2: Low-flow, distensible malformations that typically manifest in early adulthood. Symptoms include swelling of the eye or ecchymosis (bleeding underneath the skin).
- Type 3: Malformations affecting both the eye and venous system, typically resulting in an eye moving backward within the socket. Straining, coughing, or lifting heavy objects can lead to significant forward movement of the eye.
Lastly, arteriovenous malformations are characterized by abnormal, fast blood flow from the arteries to the veins, bypassing the normal flow of blood within the vessels of the eye. These malformations present with pulsating proptosis (swelling or protrusion of the eye) and could bleed, resulting in ecchymosis. These malformations are invasive and can become too aggressive, especially when not treated appropriately.
Orbital arteriovenous fistulas (AVFs) are abnormal connections between arteries and veins, which can be either congenital or acquired in nature. In either case, this can lead to swelling around the eye, pulsations, unusual noises, glaucoma, and visual disturbances.
Testing for Orbital Vascular Anomalies
Imaging techniques have become crucial in diagnosing and treating orbital vascular anomalies (OVAs), or abnormal blood vessels in the eye. Modern technology has also eliminated the need for a biopsy, or a tissue sample, for every suspected case.
When dealing with a hemangioma, a birthmark that shows up at birth or within the first or second week of life, it’s crucial to distinguish whether it’s congenital (from birth) or infantile (appeared after birth). This information helps to plan the treatment. Doctors may use doppler ultrasound to check blood flow in the suspected area. An MRI or CT scan can also shed more light on the characteristics of the lesion. These exams help to rule out other serious conditions, such as rhabdomyosarcoma, a type of cancer.
Cavernous venous malformation (CVM), which is a blood-filled growth, can be initially evaluated with an ultrasound. A CT scan will show it as a well-defined, thick, uniform, lesion within the conal space of the eye. It does not usually adhere to the extra-ocular muscles and can sometimes erode bone. CT angiography, which uses a dye to visualize the blood vessels, can further help with diagnosis.
Special MRI techniques can also be used to assess blood flow in the area. For example, time-resolved imaging of contrast kinetics (TRICKS) provides high-quality images of contrast flow in the affected area. This can be helpful in identifying and assessing the condition.
It’s also important to evaluate and diagnose vascular malformations, or blood vessel abnormalities. An MRI is the preferred tool to understand the characteristics of these lesions. For example, distensible venous malformations, which previously were called “varix,” appear normal on T1-weighted images and brighter on T2-weighted images. They show strong enhancement when a contrast agent is injected.
Lymphatic malformations, which are malformations in the lymphatic system, contain micro or macro cysts. The cysts can often be found on imaging. These malformations appear as irregular patches on imaging and MRIs are more effective than CT scans in terms of differentiating recent and old bleeding.
Arterio-venous malformations (AVMs) are a specific kind of vascular malformation that can be located in or around the eye. Colour Doppler ultrasonography and other imaging tests can be used during outpatient evaluation. Various forms of CT and MRI scans can be used to evaluate AVMs. The presence of multiple void signals, which correspond with high flow vessels, is a common feature on MRIs. Angiography, an imaging test that utilizes an injection of a contrast agent directly into the feeder vessels, is a very effective method for mapping the entire vasculature of AVMs.
Treatment Options for Orbital Vascular Anomalies
When it comes to diagnosing conditions related to blood vessels (vascular lesions) in the eye socket (orbit), the way you correctly diagnose them is key, as it can dictate the best course of treatment.
Hemangioma, for example, is a condition where blood vessels grow excessively in an area. There are two main types: infantile hemangioma (IH) and congenital hemangioma, both of which require different treatments. For infantile hemangioma, commonly, beta-blocking medications like propranolol and timolol are typically used. Atenolol may also be used if propranolol is not suitable. In more severe cases that do not respond to these treatments, drugs like bevacizumab or bleomycin may be used, though these drugs are still being tested. Laser treatment may sometimes be used for treating scars after the hemangioma is gone. Before starting any medication, a thorough heart examination of the child is necessary.
For congenital hemangioma, which is present from birth, there are no proven medicinal treatments currently. Surgical removal is usually done between the ages of 2-5 years. For larger hemangiomas, pre-operative embolization, a procedure done by an interventional neuroradiologist to cut off blood flow to the hemangioma, can help prevent excessive bleeding during surgery.
Vascular malformations like cavernous venous malformations (CVM) are often monitored until they cause symptoms such as vision loss, disfigurement, or misalignment of the eyes. Surgical removal of these can be considered when symptoms appear. The approach to surgery depends on where exactly the malformation is located.
There are also other types of vascular malformations, including venous and lymphatic malformations which often require different treatment approaches depending on associated symptoms. Treatments can range from observation for less severe cases, to minimally invasive procedures, or even surgery for more severe conditions or large, localized lesions.
Arteriovenous malformations (AVMs) are another group of conditions where there is disordered blood flow because of abnormal connections between arteries and veins. Proper understanding of the condition’s characteristics helps inform the best treatment strategy, which often includes pre-operative embolization followed by surgical removal of the malformation. Care is taken to remove all of the malformation to prevent recurrence. AVMs that cannot be removed may be managed conservatively, as surgery can carry significant risks. Carotid-cavernous fistulas (CCFs) are a subset of AVMs which can often be managed using a minimally invasive procedure known as embolization.
Finally, there are dural fistulas, which are abnormal connections between an artery and a vein within the layers that surround the brain. They are often managed conservatively as they can resolve on their own. Surgical intervention may be considered if they lead to persistent symptoms or vision loss.
By understanding the specifics of each condition, your doctor can work towards providing you with the most effective and appropriate treatment for your situation.
What else can Orbital Vascular Anomalies be?
When a doctor is trying to determine the cause of a mass in the orbit, or eye socket, they consider a few factors including:
- Is the mass inside (intraconal) or outside (extraconal) the area containing the eye’s muscles and nerves?
- What is the nature of the mass?
- Where exactly is the mass located in the orbit?
If the mass is a well-defined solid tumor, they will consider these possibilities:
- Cavernous venous malformation (a cluster of dilated veins)
- Schwannoma (tumor from nerve sheath cells)
- Solitary fibrous tumor (rare tumor of soft tissues)
- Lymphoid lesions including lymphoma (cancer of lymphocytes) or benign reactive hyperplasia (non-cancerous enlargement)
- Orbital metastasis (cancer that has spread to the orbit from other parts of the body)
- Fibrous histiocytoma (a type of cancer affecting the connective tissue)
- Neurofibroma (tumor of nerve tissue)
What to expect with Orbital Vascular Anomalies
Each blood vessel abnormality in the eye area behaves differently. How well you might do (the prognosis) largely depends on the type, size, and location of the abnormality. Also, how good your vision is and the condition of your optic nerve – the part of your eye that sends images to your brain – can impact the outlook.
Possible Complications When Diagnosed with Orbital Vascular Anomalies
Surgeries for larger lesions that extend to the back of the eye and those associated with optic nerve damage can lead to higher chances of vision complications. Other potential complications include drooping of the eyelid (ptosis) and limitations in eye movement. However, these side effects typically go away within a few months. It’s also not rare for these issues to come back. A crucial aspect to keep in mind when managing blood vessel irregularities in children is the risk of developing lazy eye (amblyopia).
Possible complications:
- Vision-related complications for larger lesions
- Drooping of the eyelid (ptosis)
- Limitations in eye movement
- Reoccurrence of these issues
- Risk of developing lazy eye (amblyopia)
Preventing Orbital Vascular Anomalies
Patients and their family members should be advised to keep up with regular appointments with their eye doctor, children’s doctor, and the relevant imaging specialist. It’s essential to understand the details of their condition, what complications could occur, and the pros and cons of the recommended treatment. This understanding will help them make informed decisions about their care.