What is Retinal Hemorrhage?
Retinal hemorrhages, or bleeding in the back of the eye, are important signals that can help diagnose a deep-seated and possibly systemic blood vessel disorder. These hemorrhages can vary in size from tiny spots (dot and blot hemorrhages) to very large bleedings (sub-hyaloid hemorrhages). Several details about hemorrhages, such as their location, size, and spread, can offer clues to their origin and reveal underlying health issues. These could include blood vessel diseases, blood disorders, infections, injury, or a lack of oxygen. Sometimes, retinal hemorrhages can occur without any known cause (idiopathically).
Most people who develop this condition need a detailed medical examination to identify the cause of the hemorrhages. Treatment typically involves monitoring the issue, treating the root cause, and managing eye health to lessen the effects of reduced oxygen to the eye (ischemic) and the development of new, often abnormal, blood vessels (neovascularization) that occur after the hemorrhages.
What Causes Retinal Hemorrhage?
Bleeding in the retina, known as retinal hemorrhages, can occur due to various conditions and the stage or severity of the disease might influence its occurrence. Here are some conditions that might lead to retinal hemorrhages:
- Ocular diseases: Certain eye diseases like Age-related macular degeneration (a condition where the central part of the retina deteriorates), polypoidal choroidal vasculopathy (an eye disorder that causes abnormal blood vessels under the retina), optic disc hemorrhages (bleeding in the eye’s optic nerve), and juxta foveal telangiectasia (condition that affects the blood vessels of the retina) can lead to retinal hemorrhages.
- Diabetic retinopathy: This is a complication of diabetes that affects the eyes, causing spots of blood and fluid leak in the retina.
- Hypertensive retinopathy: This condition is caused by high blood pressure, leading to damage in the blood vessels in the retina.
- Retinal vein occlusions: This is a blockage of the veins that carry blood away from the retina, which leads to bleeding in the retina.
Retinal hemorrhages can also be caused by a few other conditions or events:
Trauma: Various forms of physical trauma can cause bleeding in the retina. For instance, in Terson syndrome (caused by bleeding into the eye) and Valsalva retinopathy (caused by a sudden increase in pressure in the chest or abdomen), preretinal hemorrhages (bleeding into the space between the retina and the vitreous, which is the clear gel that fills the eye) are common. Shaken baby syndrome and birth trauma can also cause retinal hemorrhages.
Anemia, leukemia, bacterial endocarditis: These conditions can all lead to retinal hemorrhages, with different patterns of bleeding noted within the eye.
Sickle cell anemia: This is a severe hereditary form of anemia in which a mutated form of hemoglobin distorts the red blood cells into a crescent shape at low oxygen levels. This condition leads to retinopathy, a disease of the retina that results in visual impairment.
Ocular ischemic syndrome, preeclampsia, connective tissue disorders (lupus), high altitude retinopathy: In these conditions, the eye’s ability to get enough blood is affected, leading to retinal hemorrhages.
Mostly these conditions result in retinal hemorrhages in both eyes, although the intensity can vary.
Risk Factors and Frequency for Retinal Hemorrhage
Retinal hemorrhages are a medical condition where one experiences bleeding into the part of the eye called the retina. About 15% of critically ill children with no history of trauma or abuse experience this. Retinal hemorrhages are typically mild and often occur in children under two years old. They can be linked with systemic infections, accidental head injuries, and serious conditions that affect blood clotting.
Looking at newborns, about 25% of those born through normal delivery and 40% to 50% of those born through instrumental deliveries have birth-related retinal hemorrhages. Further, 30% of physically abused children show signs of such hemorrhages, and most of these children are less than six months old.
In adults, retinal hemorrhages are most often seen in those over 40 years old, as most systemic disorders are common at this age.
Signs and Symptoms of Retinal Hemorrhage
Doctor’s usually ask for a detailed history to determine a diagnosis; this might include questions about the patient’s environment, their use of medicines, if there’s been any injury or trauma, and if they have seen any flashes or floaters in their vision. This is necessary for understanding certain eye conditions. They also examine patients’ eyes using a device called a ‘slit lamp’, measure pressure inside the eye, and examine the back of the eyes once they are dilated. Other tests including OCT, FFA, and fundus photography are also commonly conducted to determine the details of the eye condition. If a child under three years old has injury marks on the retina along with a head injury, it may be a case of abusive head trauma.
- In-depth patient’s history
- Slit lamp examination
- Measurement of intraocular pressure
- Dilated eye examination
- OCT (Optical Coherence Tomography)
- FFA (Fundus Fluorescein Angiography)
- Fundus photography
Testing for Retinal Hemorrhage
If your doctor suspects that you may have retinal hemorrhages (bleeding in the part of your eye that senses light), they will need to conduct a series of tests to pinpoint the cause of the bleeding. This is because retinal hemorrhages can be due to different underlying health conditions.
Initially, the doctor will need to check your blood pressure, body mass index, and blood sugar levels. Following this, further tests may need to be carried out based on the suspected cause.
If the doctor suspects you may have diabetes or a metabolic syndrome, additional blood tests may be necessary. These include a complete blood count (measuring different types of cells in your blood), a platelet count (to check how well your blood can clot), a test for C-reactive protein and the erythrocyte sedimentation rate (to check inflammation), and checking fasting glucose, hemoglobin A1c and your lipid profile (to check for signs of diabetes).
If the suspected underlying cause is a hypercoagulable state, a condition where your blood clots more easily than normal, different tests may be required. These may check for different blood clotting factors and antibodies in your blood.
If an autoimmune disease such as systemic lupus erythematosus (SLE) is suspected, then your doctor may check for antibodies that are usually present in these conditions. Another reason you could be showing these symptoms is if you have an infection. To check for this, your doctor may use tests such as an ELISA (which checks for specific antibodies or proteins in your blood), or tests for specific infections such as herpes or syphilis.
Sometimes the cause of symptoms may be unclear or may mimic other diseases. This is often referred to as a “masquerade syndrome”. In these cases, your doctor may test for Lyme disease, herpes, and syphilis.
If both the front and back sections of your eye are impacted, your doctor may want to rule out a condition called Behcet’s disease. This condition occurs when your body’s immune system mistakenly attacks your own cells instead of harmful substances like viruses or bacteria. This could also be investigated using a test for HLA-B5/B12.
Remember, running these tests is a routine part of investigating suspected retinal the exact test your doctor requests may vary based on what they suspect to be the root cause of your symptoms.
Treatment Options for Retinal Hemorrhage
A single retinal hemorrhage, which is bleeding in the eye, can be monitored over time to see if it gets bigger or if more appear. If the bleeding doesn’t impact your vision, it doesn’t generally require immediate treatment. However, it’s important to find out and treat the underlying health problem that may be causing the bleeding in the first place. BUT, if the bleeding occurs in an area of the eye called the submacular, subhyaloid, or vitreous locations, treatment is required immediately due to their potential to permanently damage vision.
Certain types of retinal hemorrhages, like dot and blot, splinter, and flame-shaped ones typically don’t threaten vision and can simply be monitored. Hemorrhages related to retinal vein occlusions aren’t specifically treated, instead, any accompanying retinal swelling or the growth of new blood vessels needs to be addressed. Roth spots, another type of hemorrhage, usually resolve themselves when the disease causing them, often an infection of the heart lining, is treated.
In case of subhyaloid hemorrhage, which is commonly observed in Terson syndrome and Valsalva retinopathy, the first strategy is usually conservative observation. If it doesn’t improve within 1—3 months or if it greatly impacts the patient’s quality of life, a laser procedure can be performed to allow the blood to drain from the area, which helps recover central vision quickly. If vitreous hemorrhage, bleeding into the clear gel that fills the space in the middle of the eye, continues to block vision, a surgical procedure called pars plana vitrectomy (PPV) might be required.
Submacular hemorrhage (SMH) is serious and can cause vision loss due to damage such as the growth of abnormal blood vessels under the retina. This can affect people with age-related macular degeneration, high myopia, angioid streaks, and others. Symptoms of this condition include distorted or blurry vision. Untreated, it can cause irreversible vision loss.
Treatment for SMH revolves around moving the blood away from the fovea, the part of the eye responsible for sharp central vision. This can be accomplished through gas injections that displace the blood, clot dissolving medications, or injections of medicines that block abnormal blood vessel growth. In some specialized cases, a kind of eye surgery called pars plana vitrectomy with certain injections or devices may be adopted.
Vitreous hemorrhage, bleeding into the body of the eye, is often seen in conditions like diabetic eye disease and retinal vein occlusions. Treatment strategies here vary depending on how severe the bleeding and vision loss is. Rest and avoiding certain medications can help, along with certain treatments to seal retinal breaks or to treat abnormal blood vessels that may be present. If the bleeding doesn’t stop, or if the retina becomes detached, a procedure like pars plana vitrectomy may be necessary. If there’s a blockage in the eye’s drainage system due to a long-standing vitreous hemorrhage, treatment becomes crucial as it can increase eye pressure and lead to a form of glaucoma.
What else can Retinal Hemorrhage be?
Retinal hemorrhages, or bleeding from the blood vessels in the eye, can occur in people of any age, and the causes can differ depending on age.
For newborn babies, the common causes include those linked to birth trauma. These might be from a standard vaginal birth, or from birth assisted by vacuum extraction or forceps.
For infants and children, retinal hemorrhages might be due to:
- Eye-related conditions: child abuse, a disease called Coat disease, abnormalities with the jelly-like substance in the eye (persistent hyperplastic persistent vitreous), premature development of the retina in infants (retinopathy of prematurity), and abnormalities in the development of the retina (retinal dysplasia). Other things like high blood pressure, and nearsightedness also contributes.
- Systemic issues: These include blood or cardiovascular disorders, infections, or deficiency of a blood clot preventing substance called protein C.
For adults, common causes of retinal hemorrhages are conditions like diabetes, high blood pressure, leukemia, disorders of the blood, oxygen deprivation or high altitude syndromes, extreme nearsightedness, separation of the jelly-like substance at the back of the eye from the retina (posterior vitreous detachment), and retinal tear or detachment.
Roth spots are retinal hemorrhages with white or pale centers, and they can be caused by:
- Bacterial infection of the heart (subacute bacterial endocarditis)
- Leukemia
- Anemia
- Oxygen deprivation (anoxia)
- Carbon monoxide poisoning
- Long-lasting intubation during anesthesia
- High blood pressure during pregnancy (preeclampsia)
- High blood pressure
- Eye disease related to diabetes (diabetic retinopathy)
- Eye disease related to HIV (HIV retinopathy)
- Difficult labor and traumatic delivery in mothers and newborns
- Shaken Baby Syndrome
- Brain hemorrhage due to abnormal blood vessels (arteriovenous malformation) or a weak, bulging area on an artery (aneurysm)
- A sudden decrease in eye pressure following an eye surgery called trabeculectomy
What to expect with Retinal Hemorrhage
Most cases of retinal hemorrhages – bleeding in the back part of the eye – in newborns and infants that occur due to injury or trauma typically heal on their own in about 2 to 4 weeks. Similarly, those caused by metabolic syndromes or blockages in the veins improve once the underlying conditions are managed effectively.
However, not all retinal hemorrhages have a positive outcome. Submacular and subretinal hemorrhages, which occur in the area beneath the central part of the retina, can severely and permanently affect vision due to damage to the light-sensitive cells in the eye. These types of hemorrhages often have a very poor prognosis.
In contrast, subhyaloid hemorrhages, those that occur in the front part of the retina, typically have a good prognosis if they are appropriately and timely treated using a particular type of laser treatment known as ND-YAG laser.
Generally, most vitreous hemorrhages, which are bleeds into the gel-like substance in the eye, resolve within three months. However, small remnants of the blood clot might still be visible within the eye, settled at the bottom. Hemorrhages that do not resolve or those that lead to secondary glaucoma – a condition causing damage to the optic nerve – tend to carry a poor prognosis.
Possible Complications When Diagnosed with Retinal Hemorrhage
Here are the potential problems that can happen due to bleeding in the back of the eye (retinal hemorrhages) and related diseases:
- Damage to the light-sensing cells in the eye, which can cause permanent loss of vision
- New blood vessel growth and Ghost cell glaucoma, a type of eye pressure problem
- Blood buildup in the jelly-like substance inside the eye
- Fibrous tissue development beneath the macula, an area in the retina responsible for sharp central vision
- Abnormal growth of blood vessels in the retina
- Growth of fibrovascular tissue, a combination of fibrous and vascular tissue, between the retina and the vitreous humor in the eye

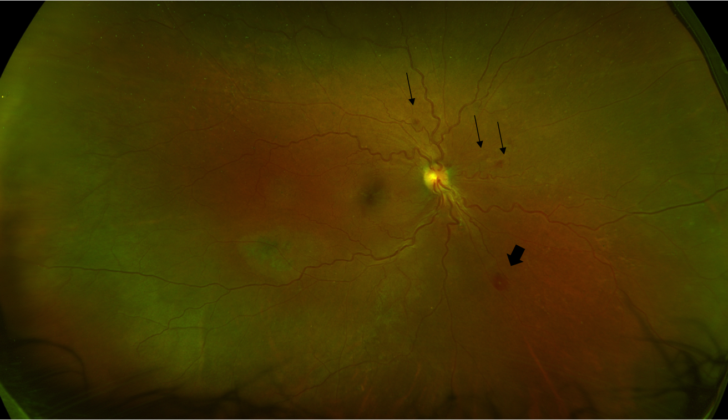
presenting with hemorrhagic ischemic vascular occlusion. Retinal hemorrhages,
vascular obliteration, and sheathing temporal to the macula can also be seen.
Preventing Retinal Hemorrhage
It’s important to let patients know about their retinal hemorrhages, which are bleeding instances in the back part of their eye. They should also understand how crucial it is to manage their other co-existing health conditions. Distributing educational hand-outs and materials can help them understand this better.
Patients should also be made aware of the concept of multidisciplinary liaison. This simply means that various health professionals work together to manage their health, as their different diseases can affect and interact with each other.
Moreover, patients should be informed about the potential threat retinal hemorrhages pose to their vision. They should be given a clear understanding of how these conditions may progress over time and what negative effects they may have if left unmanaged.