What is Retinal Traction Detachment?
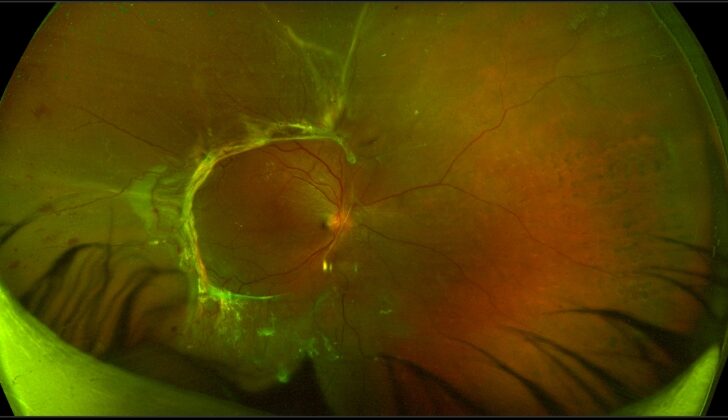
Retinal traction detachment (RTD) – or tractional retinal detachment (TRD) – refers to when the layer of nerve cells in the eye (the neurosensory retina) gets separated from the layer of cells at the back of the eye that give it its color (retinal pigment epithelium). This happens because of a pulling force caused by growing membranes on the retina surface or the jelly-like substance in the eye called ‘vitreous’. This growth of membranes can come from different causes, but it is most often caused by a condition called proliferative diabetic retinopathy (PDR). PDR is a complication of long-term unchecked diabetes.
In a detached retina situation, the retina takes a concave (curved in) shape rather than the convex (curved out) shape seen in a condition called rhegmatogenous retinal detachment (RRD). The key difference between RRD and RTD is that RRD is caused by one or more tears or breaks in the retina. On the other hand, RTDs are caused by pulling forces, and there’s no actual tear or break in the retina in the case of RTD.
What Causes Retinal Traction Detachment?
Retinal traction detachment, a condition where the retina pulls away from its normal position, can occur due to several reasons. These reasons can be sorted into two groups: those that affect adults and those that affect children.
In adults, different factors can lead to this condition:
- PDR (Proliferative diabetic retinopathy, a complication of diabetes that affects the eyes)
- RVO (Retinal vein occlusion, a blockage in one of the small veins that carry blood away from the retina)
- Retinal vasculitis (inflammation of the blood vessels in the retina)
- Physical injury to the eye
- Sickle cell retinopathy (eye problems resulting from sickle cell disease)
- Uveitis (inflammation inside the eye)
- PVR (Proliferative vitreoretinopathy, an eye condition that causes scarring on the retina)
- Penetrating trauma (severe physical injury that tears the eye)
In children, various factors can lead to retinal traction detachment:
- ROP and its complications (Retinopathy of prematurity, an eye condition that affects premature babies)
- FEVR (Familial exudative vitreoretinopathy, a hereditary eye disorder that can cause vision loss)
- PFV (Persistent fetal vasculature, a rare birth defect where blood vessels in a baby’s eye don’t develop normally)
- Toxoplasma retinitis (an infection in the retina caused by a parasite called Toxoplasma)
- Toxocara retinitis (an infection in the retina caused by a parasite called Toxocara)
- Sickle cell retinopathy
- Physical injury to the eye
- PVR
- Incontinentia pigmenti (a rare genetic disorder affecting the skin, hair, teeth, nails, and eyes)
Risk Factors and Frequency for Retinal Traction Detachment
Retinal traction detachment (RTD) is a condition that affects the eye. Large scale studies detailing its exact occurrence aren’t widely available, mainly because it has multiple causes. Yet, one research in southern Denmark showed the yearly rate to be about 1.25 cases per 100,000 residents. In this research, there was an almost even split in cases between men (48.7%) and women (51.4%), with the average age being 59.3 years.
- Diabetic vitrectomy, a surgical procedure for the eye, can sometimes lead to RTDs. This has been reported in 20% of the early studies and risen to 46% in more recent ones.
- Another report found RTDs in 36.6% of all cases of a procedure named ‘pars plana vitrectomy’ – an indication that RTDs are increasingly becoming a major reason for this surgery in diabetic retinopathy (a diabetic eye disease) patients.
Signs and Symptoms of Retinal Traction Detachment
Retinal traction detachment is often caused by systemic issues, so understanding a person’s health history is crucial. For adults, information about conditions such as diabetes, high blood pressure, kidney health, sickle cell retinopathy, and trauma are important. Similarly, for children, details about birth weight, gestational age, any infections the mother had during pregnancy, and family history are vital. Also, any co-occurring health conditions like kidney disease, heart disease, and nerve damage should be noted. It’s important to include whether these conditions are well-managed or not well-controlled.
Testing for Retinal Traction Detachment
If you’re having an eye examination, various tests might be done to get a better understanding of what’s happening inside your eye. This could include a detailed light test (slit-lamp biomicroscopy), a test to examine the back of your eye (fundoscopy), photos of the back of your eye, a dye test to look at the blood vessels in your eye (fundus fluorescein angiography), and a 3D scan of your macula (the part of your eye responsible for detailed vision).
Your doctor will also check how your eyes align – if they’re not lined up correctly especially over a long period, this could lead to other challenges like loss of vision. Another check will involve shining a light into your eyes (pupillary reflex) to check for any defects in the nerve pathways between your retina and your brain.
The structure and blood flow of your iris (the colored part of your eye) would also be inspected for signs of abnormal blood vessel growth (neovascularization). If you also have a cataract (cloudy patch in the eye), this would be assessed as well because this would help decide if cataract surgery should be done as well.
Focusing on the back of your eye, the doctor will take note of any abnormal growths, areas of retinal detachment (when the retina pulls away from its normal position), and presence of blood either beneath or on the retina. These details are important to note before any eye surgery.
A 3D imaging test (Spectral-domain optical coherence tomography) can also help in understanding the exact state of your eye membranes. This technique might reveal details around the perfect location for surgical action, the presence of bands under the retina, the exact status of your fovea (a small spot in your retina responsible for sharp, clear vision) and any distortions or damage.
Through the use of different types of photographs, doctors can document the severity and progression of any issues in the retina. There’s also a specific imaging test (fundus autofluorescence) that helps to see the parts of the retina where laser treatment could work.
In some unclear cases where the exact cause of the retinal issue isn’t obvious, a dye test might be given to highlight areas of unnoticed abnormal vessel growth or ‘starved’ areas of the retina which could impact how successful a vision recovery might be after treatment.
Another test, Ultrasound B scan, might be used to help find areas of retinal detachment, floating clots or cells in the jelly-like substance inside your eye, and bleeding in and around the retina. It described retinal detachment in an ‘x’ or ‘H’ shaped manner based on whether the retina attached at a small or large area respectively.
Finally, beyond the eye, blood tests would be done to check your blood sugar levels, kidney function, blood pressure, blood cholesterol levels and a simple urine test might be done to check for protein, often an early indicator of kidney disease. This is important to ensure that any underlying conditions are also treated to prevent recurrence or complication of eye problems.
Treatment Options for Retinal Traction Detachment
The treatment plan for Tractional Retinal Detachment (TRD), a condition that can lead to vision loss, involves two approaches: systemic management and ocular management.
Systemic management focuses on controlling the underlying medical conditions that could contribute to TRD like diabetes, high blood pressure, kidney diseases, and hemoglobin diseases. This part is usually guided by one’s personal physician or the appropriate specialist.
Meanwhile, ocular management focuses on treating the eye problem itself, which is usually directed by a vitreoretinal surgeon. It had been shown that the use of modern surgical equipment has led to better outcomes for patients with Tractional Retinal Detachment. The decision to perform surgery is dependent on various factors such as the overall health condition of the patient and the progression of the eye problem.
Before the surgery, some patients are given anti-vascular endothelial growth factor (VEGF) agents. These are medications that help slow down the growth of new blood vessels within the eyes. Common examples include bevacizumab and ranibizumab. These agents help reduce bleeding during surgery, which can make the surgical procedure a bit easier. They are usually administered a few days before the surgery.
In addition to anti-VEGF agents, a procedure called Pan-retinal Photocoagulation (PRP) might be considered. PRP uses a laser to treat the entire retinal surface. This can help stabilize the eye in cases of TRD.
Vitrectomy is the surgical procedure used for TRD, and demands a high level of surgical skill. The procedure involves removing the jelly-like substance called vitreous that fills the eye. In TRD, this substance is usually detached in the mid periphery but multiple attachments remain at the center of the eye, thus forming a vitreous cone. Firstly, the surgeons remove the central vitreous and then proceed to release any remaining vitreous in the periphery.
Different surgical instruments and techniques are used in vitrectomy, according to the surgeon’s expertise and the individual patient’s condition. After surgery, some patients might be given tamponade agents, which are substances that help seal retinal tears or detachments.
This surgery is a complex one and requires careful planning, the surgeon’s expertise, and a good understanding of the disease. But thanks to scientific advances and the development of new surgical equipment, TRD surgery has become more predictable and safer, leading to improved outcomes for patients.
What else can Retinal Traction Detachment be?
When eye doctors are diagnosing a retinal traction detachment, there are a couple of other conditions they consider because they can present similar symptoms. These conditions include:
- Taut Posterior Hyaloid (TPH)
- Vitreomacular Traction Syndrome (VMTS)
What to expect with Retinal Traction Detachment
The recovery outlook for Retinal traction detachment, a condition where the retina gets pulled from its normal position, can be affected by several body-wide (systemic) and eye-specific (ocular) factors. Body-wide factors include how well diabetes is controlled, kidney function, blood pressure levels, and the presence of a condition called sickle cell hemoglobinopathy, which affects red blood cells.
When it comes to the actual surgery to fix retinal detachment, several factors can influence the recovery process. These include the equipment used in the surgery, how long the surgery takes, the technique used to remove the membrane causing the detachment, what agent is used to place pressure on the mend, and the experience of the surgeon. Some studies have found that using a material called silicone oil can result in less successful recovery. This might be because silicone oil is often used in more complex cases, where more extensive damage has already occurred to the retina.
The results of this type of surgery can vary greatly, but they usually depend on how well certain body-wide conditions are managed, like diabetes.
Interestingly, a study found that racial backgrounds may influence recovery outcomes. It suggested that those from African descents lost vision after the operation, while white and Asian individuals gained vision. This could be due to more extensive areas of the retina being stuck down in those of African descent. There have also been reports that low-income Latinos may have more advanced retinal detachment when they first seek treatment and may not always comply with post-operation care instructions.
Patients with diabetic retinal detachments are usually at a late stage of diabetic retinopathy, a complication of diabetes that affects the eyes. Doctors should explain the advanced stage of the disease and the potentially serious impact on vision. The goal of the surgery is to reattach the retina in hopes of maintaining current vision levels or to prevent additional vision loss. However, in some cases, vision may continue to decline and the loss of light perception may occur.
Unfavorable vision results may be caused by delayed treatment, advanced disease, longer duration and increased elevation of the part of the retina responsible for central vision (macula) being detached, damage to the optic nerve due to aging or insufficient blood supply, thinning or holes in the macula, persistent fluid under the retina, damage to the outer layer of the retina and light-sensing cells, and insufficient blood supply to the entire retina.
Possible Complications When Diagnosed with Retinal Traction Detachment
Retinal traction detachment can lead to many complications, such as progressive retinal ischemia and atrophy, which can affect the layer of the eye that senses light, known as the photoreceptor layer. As the retinal ischemia progresses, new blood vessels can form in the iris (NVI), angle (NVA), or cause neovascular glaucoma (NVG), a type of eye condition. Surgery for retinal traction detachment – vitrectomy – also has its complications. These may include bleeding into the vitreous humour (VH), increased eye pressure, recurrence of the retinal detachment, cataract formation, and NVG.
After eye surgery, patients might face a few complications:
1. Dispersed vitreous hemorrhage (VH): After retinal traction detachment repair, 5% to 55% of patients might experience this type of bleeding. Though immediate VH might resolve on its own, constant occurrences may require treatments such as vitreous lavage, removing remaining membranes, or silicone oil tamponade.
2. Increased intraocular pressure: Post-operative increased eye pressure could be linked to inflammation, bleeding, or tamponade. If eye drops or other medications do not relieve the pressure, a glaucoma drainage device might be needed.
3. Recurrent retinal detachment: Retinal detachment can reoccur in 5-15% cases of people who undergo vitrectomy. These cases generally have a worse prognosis. Non-resolving cases of retinal detachment might require a repeat vitrectomy.
4. Cataract: Cataract formation and progression are common after vitrectomy. Cataract surgery with the implantation of intraocular lenses might be needed when the visual impairment from the cataract becomes significant.
5. Neovascular glaucoma: After a diabetic vitrectomy, levels of a molecule called VEGF increase inside the eye risking new blood vessel formation in the anterior segment. Anti-VEGF injections can counteract this process. However, in some cases, the prognosis is poor, and glaucoma drainage devices might be recommended.
List of complications:
- Progressive retinal ischemia and atrophy
- New blood vessels formation in the iris or angle or causing neovascular glaucoma
- Bleeding into the vitreous humour
- Increased eye pressure
- Recurrence of the retinal detachment
- Cataract formation
- Neovascular glaucoma after vitrectomy
Recovery from Retinal Traction Detachment
After eye surgery, doctors typically use medications such as eye drops that contain steroids and antibiotics, along with drops that help to relax the eye muscles. These are used to aid the recovery process. If any complications occur after surgery, these will be treated based on the doctor’s assessment of the situation.
Depending on where the break in the retina is located and other factors, the person who had the surgery may be advised to hold a specific posture early in their recovery. This could help the healing process. It is also very important to take care of one’s overall health during this time.
Preventing Retinal Traction Detachment
When the diagnosis of TRD (Tractional Retinal Detachment, a condition where the retina pulls away from its normal position) is delayed, it can lead to worse health outcomes. Thus, it’s crucial for people with diabetes to have regular eye check-ups to ensure early treatment of TRD can take place if needed. Similarly, babies who were born prematurely, had a low birth weight, or had blood infection (known as septicemia), are at risk of developing ROP (Retinopathy of Prematurity, an eye problem that occurs in some premature babies). It’s important for these babies to be screened early for ROP, so it can be diagnosed and treated promptly. Patients with blood disorders known as hemoglobinopathies, also need to regularly see an eye doctor to rule out any damage to the retina (retinopathy).