What is Retinopathy?
The retina in our eyes is made up of special cells called photoreceptor cells, which play a key role in processing what we see. They convert light signals into nerve impulses that travel along the optic nerve to our brain, creating an image. There are two types of these cells, rods and cones. Cone cells help us see color, while rod cells are great for seeing in low light conditions.
The macula, a small part of the retina, is responsible for our central vision. It contains a lot of cone cells, giving us clear, sharp vision. Retinopathy is a general term for any damage or alteration to the retina. This can be caused by many things, such as environmental conditions or genetic factors. The retina is especially vulnerable to damage from oxidative stress because it has a high content of polyunsaturated fatty acids and uses a lot of oxygen.
Much like the rest of our bodies, the retina relies on the circulation of blood for oxygen and nutrients to function. It gets this from two main sources, the retinal and choroidal circulatory systems. These are responsible for supplying oxygen and nutrients to the inner and outer halves of the retina, respectively. However, if blood flow to these areas is reduced, it can lead to damage of the optic nerve and loss of vision. Similarly, if the small blood vessels in the retina burst, it can cause bleeding into a part of the eye called the vitreous humor, leading to vision loss.
What Causes Retinopathy?
Diabetic retinopathy (DR) is a common eye condition related to diabetes, and it’s a leading cause of vision loss and blindness in adults. Poor control of blood sugar levels and high blood pressure are key contributors to this condition. There are two types of diabetic retinopathy: a proliferative form (PDR) and a nonproliferative form (NPDR).
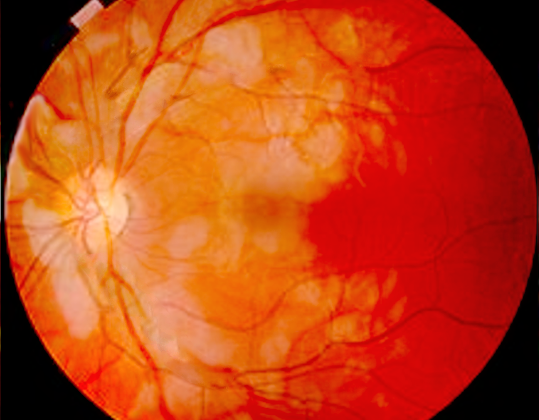
In NPDR – the less severe form – tiny blood vessels in the retina of the eye balloon and form pouches, often leaking blood and fluid into the retina. If this happens in the center of the retina, known as the macula, it can lead to a condition called macular edema which can impair vision. PDR is more advanced and occurs when new, leaky blood vessels grow within the retina. This eventually makes the retina more susceptible to bleed into the vitreous – the clear, jelly-like substance that fills the center of the eye. When this happens, light cannot reach the photoreceptor cells that provide vision.
Hypertensive retinopathy is another eye condition, caused by high blood pressure. Chronic high blood pressure can cause the small blood vessels in the retina to tighten, which can damage the blood vessel walls over time. This can eventually lead to the final “sclerotic” stage of the disease, which involves hardening of the small blood vessels.
Retinopathy of Prematurity (ROP) is a condition that can cause blindness and vision loss in premature and low birthweight babies. Although very rare, it can also affect full-term babies. This eye disease has been linked to premature babies needing to have additional oxygen treatment.
A protein called Vascular Endothelial Growth Factor (VEGF) plays a significant role in these eye conditions. Lack of oxygen in the eye can lead to increased production of VEGF that stimulates abnormal growth of blood vessels. Oxygen treatment for ROP initially suppresses VEGF, resulting in abnormal development of the retina’s blood vessels and, subsequently, cell death.
Age-related Macular Degeneration (AMD) is an eye disorder associated with aging that gradually destroys sharp, central vision. AMD is of two types: “wet” (or exudative) and “dry” (or atrophic). The most common is the “dry” form, accounting for about 80-90% of all cases. The “wet” form, although less common, it is responsible for about 90% of severe vision loss. The exact cause of AMD is unknown, but it’s thought to be related to the build-up of certain fatty substances in parts of the eye.
In summary, understanding these eye conditions is important in seeking the most effective treatment methods to manage symptoms and reduce the risk of vision loss. If you have diabetes, high blood pressure, or a history of premature birth, regular eye exams are important to catch these conditions early.
Risk Factors and Frequency for Retinopathy
Retinopathies, or diseases of the retina, are major causes of vision loss across the globe. Hypertensive retinopathy (due to high blood pressure), diabetic retinopathy, and age-related macular degeneration (AMD) are poised to become even more common as the world’s population gets older and rates of hypertension and diabetes rise. Additionally, improvements in premature baby healthcare have lead to more cases of retinopathy of prematurity (ROP), which is a retina issue in early-born babies. All these retinal diseases are influenced by numerous factors, including an individual’s lifestyle, the environment and genes.
- Approximately a third of those with diabetes display symptoms of diabetic retinopathy. Diabetes and high blood pressure are key risk factors, along with inflammation and oxidative stress.
- Two-thirds of patients with chronic high blood pressure show signs of hypertensive retinopathy. The main risk factors are the duration of high blood pressure, age, and high systolic blood pressure. However, BMI or gender does not significantly influence the risk.
- Age-Related Macular Degeneration (AMD) is one of the leading causess of blindness in people over 60, but is less common in people of African descent. Early AMD is more common in people of European ancestry than in Asians.
- A study conducted in the USA and Canada on the instance of Retinopathy of Prematurity shows that at least 40% of at-risk premature babies develop some stage of ROP, but most improve without treatment. However, about 8-10% can develop severe ROP, mostly seen in newborns weighing under 1250 grams.
Testing for Retinopathy
Examinations of most eye-related diseases rely on a process called ophthalmoscopy (also known as funduscopy). This process can check the health of the back of your eye (your retina), your optic disc (the area at the back of your eye that connects to your brain), and the vitreous humor (the clear, gel-like substance inside your eye). To get a clear view, your eyes would need to be dilated or widened.
There are several types of ophthalmoscopy. ‘Direct’ ophthalmoscopy uses a small handheld device with its own light source. This is usually used by general physicians for routine eye check-ups. Then there’s the ‘indirect’ variant, which also uses a handheld device but the light source is attached to your head. This type provides a wider view of your eye compared to ‘direct’ ophthalmoscopy and is generally performed by an ophthalmologist (a specialist for eye medical and surgical care). Another version is ‘pan’ ophthalmoscopy, which provides a broad view of the back of your eye without needing to dilate your pupils. ‘Slit-lamp’ ophthalmoscopy uses a fixed, powerful light source and a handheld lens, this too is typically performed by an ophthalmologist.
Interesting to note, ophthalmoscopy could help identify Alzheimer’s disease. People with this disease seem to have a higher level of drusen (small, yellow deposits) in the periphery of their retina compared to those who don’t. If this finding is confirmed, it could provide a non-invasive method for diagnosing Alzheimer’s – something we currently lack.
Moving on to hypertensive retinopathy (eye damage caused by high blood pressure), it’s evaluated best by examining photos of the back of your eye. There are various grading systems, based on the extent of damage seen through ophthalmoscopy. For example, the Keith-Wagener-Barker (KWB) system divides hypertensive retinopathy into four grades, based on the severity of damage from high blood pressure. These grades range from mild narrowing of the retinal arteries (your eye’s blood vessels) with no symptoms, up to severe eye damage with symptoms like vision loss, blurry or double vision, and headaches.
As for diabetic retinopathy (eye damage from diabetes), it’s categorized into two main types – ‘proliferative’ and ‘non-proliferative’. Different grading systems, like the Scottish system, offer a detailed protocol for classifying diabetic retinopathy. Retinopathy of prematurity (an eye disease occurring in premature babies) has five stages, based on how abnormally the blood vessels are growing. The stages range from mildly abnormal blood vessel growth to a completely detached retina, the latter being the final stage of this disease.
Treatment Options for Retinopathy
Retinopathy of prematurity (an eye disorder that affects premature babies) is mild for most newborns (at stages 1 and 2), and it often gets better on its own without treatment. To decrease the risk of the condition worsening due to high oxygen levels, babies are closely watched and the amount of oxygen they are given is carefully controlled. But, for about 8 to 10% of newborns with this eye disorder, doctors may need to intervene with treatments like laser therapy or cryotherapy.
One of the first steps towards preventing many types of retinopathy is making changes to everyday habits, such as losing weight, controlling the quantity and types of food you eat, doing aerobic exercises (like fast-paced walking with more than 130 steps per minute), quitting smoking, and limiting or avoiding alcohol. Keeping cholesterol levels normal is also important. For people who have developed eye damage due to high blood pressure, readily available and affordable medicines can help.
In the case of diabetic retinopathy (eye damage caused by diabetes), controlling your blood sugar levels is vital. If the eye disorder progresses, exercise might be risky as it can increase the chances of bleeding in the retina (the back of the eye) or the retina detaching. It’s best to avoid any form of exercise that increases blood pressure. Metformin, a medication used for type 2 diabetes, has been found to slow down the progression of this particular eye disorder.
For the treatment of AMD (age-related macular degeneration, a disease that damages the center of the retina), remedies may include diet supplements rich in antioxidants, injections of ranibizumab (a drug that inhibits VEGF, a protein that promotes the growth of abnormal blood vessels), and maybe even putting a small telescope inside the eye for patients with advanced stages of the disease.
Several lifestyle factors in pregnant women can increase the risk of having premature or low birth weight babies, who are more likely to develop retinopathy of prematurity. Addressing these risk factors can help prevent the eye disorder. These include quitting smoking, getting medical care early during pregnancy, managing substance abuse issues, and minimizing stress.
What else can Retinopathy be?
When it comes to eye health, various conditions could potentially affect the retina and surrounding areas. These include:
- Branch retinal vein occlusion
- Central retinal vein occlusion
- Hemoglobinopathy retinopathy
- Retinal microaneurysm
- Macular edema in diabetes
- Ocular ischemic syndrome
- Sickle cell disease
- Terson syndrome
- Valsalva retinopathy