What is Steroid-Induced Glaucoma?
Steroids, commonly known as “anti-swelling” or “anti-inflammatory” drugs, are often used to fight various conditions where the body’s immune system overreacts and causes inflammation. However, regular use of these medications can lead to side effects in the eyes, particularly causing conditions like glaucoma or cataracts. Glaucoma caused by steroid use was first recognized in the 1950s when researchers noticed some patients developed the condition after using hormones and steroids for other medical conditions.
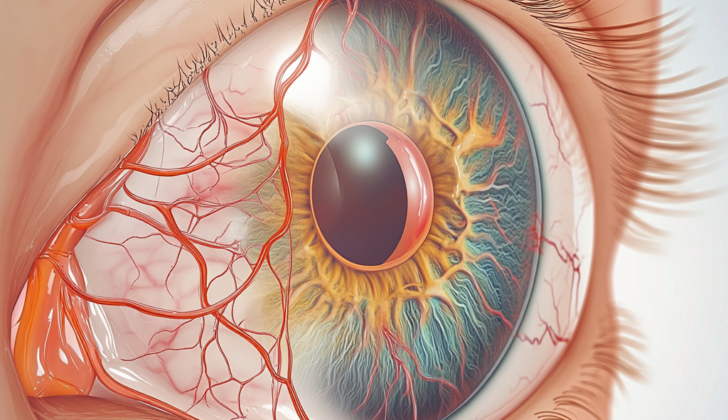
Some specific factors seem to greatly contribute to the rise of pressure inside the eyeball, or what doctors call “intraocular pressure”. One of the primary reasons for this is changes in the ‘plumbing systems’ of our eyes. Our eyes have specific structures (trabecular meshwork) that help control the fluid flow. Steroids can cause a clog in this system by altering its structure and making it more rigid.
Studies have shown that steroids can modify this structure by causing changes in the fine strands, or ‘actin fibers’, present in the trabecular meshwork. Additionally, steroids seem to increase the buildup of substances like collagen and fibronectin in some parts of this meshwork. Another impact of steroids is on the management of some substances and enzymes in the eye that help maintain the fluid balance. These modifications lead to an increase in the resistance to fluid outflow, leading to higher fluid pressure inside the eyeball.
Understanding these effects of steroid use on the eye is important when considering treatment options and preventing potential side effects.
What Causes Steroid-Induced Glaucoma?
Using steroids can sometimes lead to a condition called ocular hypertension (OHT) – this basically means the pressure inside your eyes gets too high. This is usually seen in people who are already at risk of this condition.
One type of secondary glaucoma, known as steroid-induced glaucoma (SIG), can develop if your eye pressure stays high enough to cause irreversible damage to the optic nerve, which is the part of the eye that sends images to your brain.
People who show an increase in eye pressure after using steroids are often called “steroid responders” (SR). In medical terms, an eye pressure above 21 to 24 mmHg or experiencing an increase of more than 5 to 10 mmHg compared to normal levels can make you a steroid responder.
These increases in eye pressure are most commonly seen in steroid responders after the use of steroids applied directly to the eyes, or injected around or inside the eyes. However, ocular hypertension can happen even when you use steroids through your nose, lungs, body (systemic use), or skin.
Usually, the pressure in the eye starts to rise around 3 to 6 weeks after using steroids on the eye, but it can happen sooner. If you stop using the steroid eye drops, the pressure usually goes back to normal within about two weeks. On the other hand, steroid injections in the eye can quickly raise your eye pressure. Although, other ways of using steroids might affect your eye pressure, these effects tend to be less noticeable in comparison to directly using steroids on or in your eyes.
Risk Factors and Frequency for Steroid-Induced Glaucoma
While the exact number of people with Steroid-Induced Glaucoma (SR) is unknown, studies show that cortisone eye drops cause a moderate eye pressure rise (6 to 15 mmHg) in over 30% of people, with around 5% experiencing a much higher rise (>16 mmHg). This condition can be just as, if not more, common in children compared to adults. It’s crucial to note that a sudden increase in eye pressure in people with SR and types of glaucoma like primary-open angle glaucoma, can make their condition worse.
Based on how the eye pressure responds to two types of steroids (betamethasone and dexamethasone), there are three groups:
- High responders (around 4 to 6% of people): Their eye pressure rises by more than 15 mmHg from the start or goes above 31 mmHg.
- Moderate responders (about 1/3 of people): Their eye pressure rises by 6 to 15 mmHg or falls between 25 and 31 mmHg.
- Non-responders (about 2/3 of people): Most people in this group either experience a rise of less than 6 mmHg or have an eye pressure of less than 20 mmHg.
Steroid-Induced Glaucoma can be more likely in those with certain risk factors, including a diagnosis or family history of primary open-angle glaucoma, diabetes, severe short-sightedness, and connective tissue disorders like rheumatoid arthritis. Older people and children under six are also more likely to develop the condition. In fact, studies revealed that older people are as much as 1.72 times more likely to develop SG after using cortisone eye drops.
Signs and Symptoms of Steroid-Induced Glaucoma
Using steroids, in any form, can lead to a condition known as glaucoma. This might happen if topical steroids are used, even for minor problems, after certain types of eye surgery, or if steroids are used for a long time to treat inflammatory conditions. Glaucoma caused by steroids is often like other types of glaucoma; it usually doesn’t cause symptoms and is often found by an eye doctor during a routine exam. In serious cases, patients may notice that their vision is blurry or that they have trouble seeing certain areas. These issues can come from swelling in the cornea or from cataracts caused by the steroids. Sometimes, if the pressure in the eyes gets really high really fast, it can cause a headache centered around the eyes or brows.
During an eye exam, people with this kind of glaucoma usually seem normal. The main sign is that the pressure in the eye is higher than the typical range of 10 to 22 mmHg. If a patient has a history of using steroids and their eye pressure is high, they’re considered to have steroid-induced eye hypertension. As with all forms of glaucoma, a test to measure eye pressure is essential to diagnose steroid-induced glaucoma. If high eye pressure continues for a long time, it may lead to glaucoma, with symptoms like damage to the optic nerve (the nerve in the eye that sends images to the brain) and typical vision issues seen in glaucoma.
The patient’s age can also affect the symptoms of steroid-induced glaucoma. In children, it can lead to a larger-than-normal cornea, a condition similar to one type of glaucoma that babies can have at birth. Older adults who’ve used steroids and then stopped might seem like they have normal-tension glaucoma. That’s why it’s so important for doctors to ask about past steroid use when a patient has high eye pressure.
Testing for Steroid-Induced Glaucoma
If you’re experiencing signs of a certain eye condition, your medical history can give your doctor helpful clues. People who have conditions like vernal conjunctivitis or other types of allergic conjunctivitis often use steroid eye drops for a long time. Some people might be using steroid treatment for eye conditions after surgery, such as photorefractive keratectomy (PRK), which is a type of surgery that reshapes the cornea. Others may have a steroid implant in their eye. People who have received a kidney transplant might also be more likely to develop this condition.
To diagnose steroid-induced glaucoma (SID) — a condition where the pressure in the eyes increases due to the use of steroids — doctors use the same methods they use to diagnose other kinds of ocular hypertension (OHT) and glaucoma. First, they measure how well you can see (visual acuity). They then do a thorough examination of the front (anterior) and back (posterior) parts of your eye.
Your eye doctor will also measure the pressure in your eyes by performing tonometry. This process can help them assess SID and ocular hypertension. The Goldmann applanation tonometry (GAT) is the standard method used for this. However, if this procedure is difficult to perform — such as with children, uncooperative patients, or bedridden individuals — an alternative device known as the iCare tonometer can be used. This device is easier to use and does not require anesthesia drops and a dye called fluorescein.
Other tests include visual field testing, which checks if your vision has any gaps or blind spots, and ocular coherence tomography (OCT). OCT is a non-invasive imaging test that uses light waves to take cross-section pictures of your retina. In some cases, another technique called gonioscopy might be used. This test allows your eye doctor to have a clear view of the structures at the front of your eye.
Treatment Options for Steroid-Induced Glaucoma
The first step in managing steroid-induced glaucoma (a condition where the fluid pressure inside the eye increases due to the use of steroids), is to stop using steroids, if possible. In cases where steroids can’t be completely stopped, the dosage should be reduced or a less potent steroid should be used. If the pressure in the eye is still too high, medications to lower this pressure can be introduced.
Steroid-induced glaucoma can be managed in three main ways:
1. Medication: The same types of medication used to treat primary open-angle glaucoma (a condition where the eye’s drainage canals get clogged over time) can be used. These may include beta-blockers, prostaglandin analogs, alpha-2 agonists, and carbonic anhydrase inhibitors. Beta-blockers are usually the first choice of medication for this condition.
2. Laser Treatment: If the medication doesn’t work and there’s a risk of damage to the optic nerve (which carries visual information from the eye to the brain), argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) might be used. These procedures use a laser to help fluid drain out of the eye. However, these procedures may only provide relief for several months, so they may need to be repeated. They might also be considered for patients who experience unpleasant side effects from glaucoma medication.
3. Surgery: If both medication and laser treatment fail, surgery may be necessary. This is especially true for patients who are expected to continue using steroids. The most common surgery is a trabeculectomy, which creates a new drain in the eye for fluid to exit. Other surgical options include deep sclerectomy, canaloplasty, tube shunt surgeries, or cyclophotocoagulation procedures, all of which aim to improve fluid drainage in the eye.
What else can Steroid-Induced Glaucoma be?
There are several conditions that could cause a rise in the pressure inside your eye (IOP), even when using steroids. The good thing about the increase in pressure due to steroids is that it goes away once you stop using them. That’s one way to differentiate it from glaucoma. Here are a few conditions that could cause higher than normal IOP:
- Primary open-angle glaucoma (POAG)
- Angle-closure glaucoma
- Angle-recession glaucoma
- Pigmentary glaucoma
- Plateau iris glaucoma
- Pseudoexfoliation glaucoma
- Uveitic glaucoma
What to expect with Steroid-Induced Glaucoma
The chances of getting glaucoma from high eye pressure (IOP) caused by steroids are similar to other types of glaucoma. If the eye pressure is managed properly, the chances of developing glaucoma are very low.
Preventing Steroid-Induced Glaucoma
If a patient is taking steroids, it’s important they understand these medicines could potentially raise their eye pressure, a condition medically known as Intraocular Pressure (IOP) elevation. The good news is that for most people, steroid medicines won’t significantly affect their IOP. However, a small group of people might experience a substantial increase in eye pressure. Therefore, doctors ought to inform their patients, especially individuals who already have eye conditions such as glaucoma, about the potential for an increase in eye pressure. It’s crucial to know that the risk associated with steroids causing higher IOP and advancing glaucoma is greater than for people without these eye conditions.