What is Superior Oblique Myokymia?
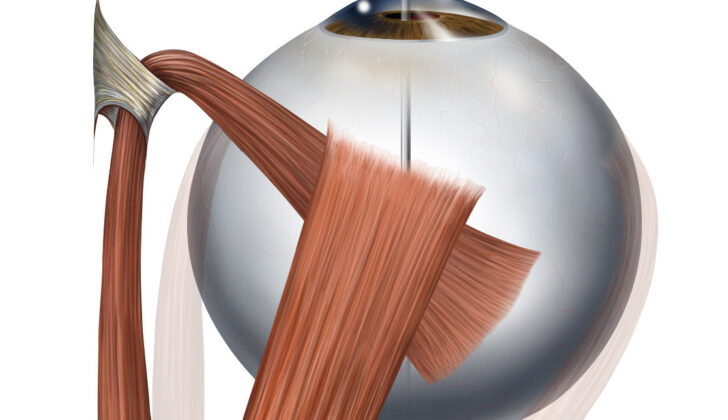
Superior oblique myokymia (SOM) is a condition where a certain eye muscle, the superior oblique, involuntarily contracts. This creates a sensation of things shaking or seeing double. SOM is something that affects only one eye. It was first noticed in 1906 by Alexander Duane, whose patient described seeing an object jump out of another and appear to move up and down. In 1970, the condition was named superior oblique myokymia by William Hoyt and James Keane, and it’s also known by this name today.
Now let’s take you back to the story of how this condition was discovered and understood. Duane first encountered it when a 24-year-old woman came to him. She complained that she had been experiencing episodes of double vision where it felt like things were moving up and down. Upon checking her out, Duane noticed that her left eye was quickly and repeatedly moving back and forth in a pattern sometimes mixed (moving vertically and spinning around) and sometimes only spinning around.
For decades, scientists did not fully understand this condition. Then in 1970, Hoyt and Keane studied five patients with similar symptoms and felt that the problem was related to the superior oblique muscle or the nerve controlling it. Dr. Hoyt found that these episodes happened out of the blue in otherwise healthy patients, with the affected eye showing rapid and low-intensity movements multiple times a day. These episodes could also go away for a few years and then return. Hoyt also detailed the best way to check for SOM: by using a tool called a slit-lamp to watch a small blood vessel in the eye for signs of unusual eye movement.
Regarding the cause, Hoyt and Keane suggested that it could be due to an injury to the nerve controlling the muscle or a change in the membrane threshold of neurons (nerve cells in the brain and spinal cord). They even compared it to a similar condition affecting the facial muscles.
Based on all these insights, Dr. Hoyt carried out a surgical procedure on the superior oblique muscle which relieved the patient’s symptoms. However, he noted that in most cases, treatment should be limited to reassuring patients that the condition is harmless. He also pointed out that surgery on the superior oblique muscle may not always be the best solution, as it could lead to persistent double vision when looking downward. This, according to him, could be more troublesome than the original condition.
What Causes Superior Oblique Myokymia?
There isn’t a one-size-fits-all reason for SOM (Superior Oblique Myokymia). Multiple incidents and health conditions could contribute.
For instance, some reports show SOM appearing in people with a family link to multiple sclerosis. This is a condition where the body’s immune system attacks the protective covering of nerves. On two occasions SOM was associated with a phenomenon where their symptoms, such as muscle stiffness and weakness, were worsened with exposure to heat. One such case involved a person who did not have multiple sclerosis.
SOM has also developed in some people after they’d experienced brain tumours, injuries or changes to the part of the brain where it connects with the brainstem and spinal cord. There is a case where a person started experiencing SOM after developing a specific brain tumour called a pilocytic astrocytoma. Once the tumor was removed, the symptoms of SOM went away. In another case, symptoms improved after treatment of a dural arteriovenous fistula, an abnormal connection between veins and arteries.
In some cases, people have developed SOM after suffering from trauma or a condition called superior oblique palsy, which is a weakness or paralysis of the eye muscles. Despite noting these associations, it’s important to note that many people with SOM have not previously experienced trauma or palsy.
There’s also evidence to suggest that structural disruptions of the trochlear nerve, a nerve in the eye, can lead to SOM. This could occur from either an injury or an issue with nerve regeneration. Conditions like hemifacial spasm, facial synkineses, epilepsy, and ocular neuromyotonia fall under this category as they’re also associated with this kind of nerve transmission.
SOM has been found to be caused by the compression of the trochlear nerve by an adjacent artery in some cases. Some patients have been relieved of their SOM symptoms after undergoing a procedure to relieve this compression. The notion of this nerve compression was first proposed as a cause of SOM in the 80s. Imaging tests like a magnetic resonance imaging (MRI) scan can help to identify these cases of nerve compression.
An understanding of the blood vessels around the trochlear nerve, like the superior cerebellar artery, has improved the understanding of SOM. Variation in the form of this vessel can influence the likelihood of nerve compression. It’s believed that nerve compression can lead to the loss of nerve protection, which likely leads to apparent nerve transmission and incorrect nervous signals causing SOM. Conditions like trigeminal neuralgia, hemifacial spasm, ocular neuromyotonia, and vestibular paroxysmia, related conditions which affect the facial nerves, endure recurrent symptoms due to nerve compression.
Though nerve compression can lead to SOM, it’s important to note that not all instances of SOM have this compression. There’s belief that some cases may involve the recovery from trochlear nerve palsy, which results in irregular nerve regeneration or transmission.
Risk Factors and Frequency for Superior Oblique Myokymia
According to a detailed review of 116 cases of a condition called superior oblique myokymia (SOM), researchers found out several important facts:
- The age of the patients examined ranged from 17 to 72 years, with an average age of 42 years.
- The age of onset of the condition was the same for both men and women.
- Half of the people observed developed the condition between the ages of 31 and 50 years, irrespective of their gender.
- The majority of the patients were young, healthy adults.
- SOM tends to affect the right eye more often (in 61% of cases).
- This tendency was statistically significant in women, but not in men.
- Both men and women are equally affected by SOM.
- All cases of SOM were found in just one eye, not both.
- MRI studies showed no differences in the structure of the trochlear nerve or the superior cerebellar arteries.
Signs and Symptoms of Superior Oblique Myokymia
Patients with this condition often complain about seeing double or experiencing a sensation of spinning images, also known as oscillopsia. These symptoms can come and go throughout the day, lasting anywhere from a few seconds to several hours. Interestingly, these symptoms only occur when the patient is awake and vanish during sleep. However, in the case of hemifacial spasms, the spasms may still be visible even when the patient is sleeping.
Patients typically associate these symptoms with factors like stress, tiredness, use of nicotine or caffeine, and even heat. However, for most people, these symptoms appear randomly. When they occur, patients become very aware of an unusual eye movement, describing it as resulting in double vision or spinning images. In some instances, having the patient look in specific ways or directions can induce these episodes.
The movements caused by these spasms are typically characterized by high frequency (up to 50 Hz) and low amplitude (less than 4 degrees). This is usually accompanied by a torsion or twisting of the eye, resulting in a rapid, irregular eye movement. Though these movements are generally small in scale, jerking movements of 5 degrees or more may occasionally be observed.
Some unique physical symptoms have been reported in certain cases. One such symptom was an unusual sound heard when a stethoscope was placed over the affected eye, described as similar to the rapid firing of a machine gun. However, this finding has not been widely reported. The intensity of these symptoms can vary greatly, with periods of remission and intensification lasting from days to years.
Usually, no abnormalities are found during an eye movement examination, although slight weakness in the superior oblique muscle might be noticeable in some cases. Other signs may include an unusual up or downward gaze or an overshifting in the downgaze of the affected eye.
Another symptom, called torticollis, might occur, which is a subtle tilting of the head to one side and down. This happens as the patient tries to position their head in a way that minimizes the discomfort caused by the oscillations in their vision.
Testing for Superior Oblique Myokymia
If you’re a patient who might have a specific nerve problem, your doctor doesn’t usually ask for an electromyography test. However, should they request it, this test can reveal important information as it shows off high-voltage discharges which are long-lasting.
Contrast-enhanced magnetic resonance imaging (MRI) is another potential test which uses a powerful magnetic field and radio waves to create detailed pictures of your body. It’s not a common choice for all patients who show signs of Superior Oblique Myokymia (SOM), a disorder affecting one of your eye muscles, because the chance of discovering a tumor in the brainstem is low. Nevertheless, if your symptoms persist or worsen despite medication, a tailored MRI can be ordered. In particular, two specific types of MRIs called FIESTA and CISS, which provide detailed flow imaging, can give a thorough view of your midbrain area.
The doctor might also consider a Magnetic Resonance Angiogram. This test can help visualize blood vessels, checking for any issues such as compression of the root of a tiny nerve called the trochlear nerve near your eye. The MRI can also provide valuable information about potential tumors or signs from a previous trauma.
Treatment Options for Superior Oblique Myokymia
Superior Oblique Myokymia (SOM) is a rare eye condition with less than 200 reported cases. It can vary in its symptoms and patients often have periods of time where they are symptom-free, which makes finding an effective treatment challenging.
Some patients have experienced relief with several medications. These include topical beta-blockers, carbamazepine, baclofen, clonazepam, memantine, mirtazapine, and phenytoin. All these medications help stabilize the cell membranes.
Carbamazepine is a medication used to control seizures and has been shown to greatly improve or even completely resolve symptoms in 80% of patients. However, it can cause side effects like rash, anemia, low sodium levels, and elevated liver enzymes which can limit its use.
Other approaches that have been successful include topical beta-blockers and systemic propranolol to manage cases of SOM. These treatments are often the first choice, as they usually have minimal side effects.
A muscle-controlling drug called botulinum toxin can also be injected into the superior oblique muscle, which is the muscle affected by SOM. However, it is difficult to inject this without affecting other muscles which could cause double vision. For this reason, this option is not commonly used.
When patients do not respond to medical treatments, surgery may be an option. There are several types of surgery that have been tried with varying success. This could include surgery on the superior oblique muscle itself, partially weakening the superior oblique tendon, or releasing pressure from the trochlear nerve, which is responsible for controlling the superior oblique muscle. These surgeries can, however, lead to other issues like double vision and may require additional procedures. Therefore, all possibilities should be discussed with the patient beforehand.
Microvascular decompression is a more complex procedure where offending arterial loops are separated from the trochlear nerve. This has proven effective but should be reserved for patients with severe symptoms not alleviated with other treatments or surgeries.
Finally, for patients with minimal symptoms, a “watch and wait” approach with no treatment may be the best option. For symptomatic patients who do not respond to treatments, neuroimaging (scanning of the brain and nerves) can be used to look for more targeted surgical interventions.
To sum up, the optimal management of SOM depends on the patient’s symptoms and their response to specific treatments. If symptoms persist despite trying one treatment, other options may be explored in consultation with the healthcare provider.
What else can Superior Oblique Myokymia be?
When we talk about different eye conditions, it’s crucial to understand the different symptoms and causes. Let’s break these down into more simple terms:
- Inferior oblique myokymia: This is a rare condition where the eye moves away from the nose rather than towards it when you look up. This was first described by Chinskey and Cornblath in 2013.
- Alternating superior and inferior oblique myokymia: This involves changes in the eye’s movements that are small but fast. Symptoms include the eye moving towards and away from the nose. This was described by Smith and Cornblath in 2014.
- Eyelid myokymia: Here, patients experience contractions in the muscle surrounding the eye, which can lead to changes in vision. This isn’t a type of double vision, but rather the result of the pressure from the contracting muscle on the eye. Triggers could be stress, fatigue, or caffeine. This condition can last for a few hours or even weeks, but usually resolves on its own. In some cases, you might need an injection of a drug that relaxes muscles.
- The Heimann-Bielschowsky phenomenon: This condition involves vertical movement of the eye. It typically occurs in individuals with reduced vision in one eye, has a low frequency, and is associated with no other neurological conditions.
- Square wave jerks: These are tiny, fast movements of the eye associated with central neurological conditions resulting in the eye’s inability to stay still. Patients may not have any symptoms, or they may see side-to-side image movements.
- Ocular neuromyotonia: This involves sudden and temporary contractions of one or more muscles that move the eyes. It’s often related to injury from radiation and is considered to be caused by damage to the nerve lining. The spasms are slower than those seen in SOM, and it’s rare for only the muscle that moves the eye towards the nose to be involved. It’s usually triggered by an unusual gaze.
What to expect with Superior Oblique Myokymia
Most people with SOM (superior oblique myokymia) will experience symptoms such as a “shaky” or double vision. As the range of symptoms can differ greatly, not everyone will need treatment. However, most people who are treated with eye drops known as topical beta-blockers, sometimes along with other medications, will notice a decrease or even disappearance of their symptoms.
Some people may need a specific type of eye muscle surgery, known as superior oblique tendon surgery, sometimes accompanied by another procedure called ipsilateral inferior oblique surgery, to alleviate or even erase their symptoms.
Last of all, a small number of patients whose symptoms are particularly stubborn and impossible to resolve by normal means should consider an operation performed on the brain called neurosurgical decompression surgery. This is a major operation and not without risks, but so far, it has proven to be quite effective.
Possible Complications When Diagnosed with Superior Oblique Myokymia
Patients who have a surgical procedure to weaken the superior oblique tendon often experience double vision. Over one third typically have this issue. These patients may require another surgery on the external muscles of the eye to correct the double vision, or they may need to use prismatic glasses. It’s hard to evaluate the complications of neurosurgical procedures, like neurovascular compression, simply because it has been performed on very few patients so far. However, we know that half of these patients develop a condition called fourth nerve palsy after surgery. This condition usually improves on its own over a period of weeks or months. You should be aware that all types of neurosurgical procedures come with certain risks, including potential health problems and even death.
Common Complications:
- Double vision
- Need for further eye muscle surgery
- Need for prismatic glasses
- Fourth nerve palsy
- Potential health problems from neurosurgery
- Death
Preventing Superior Oblique Myokymia
It’s crucial to inform patients about a condition known as superior oblique myokymia. In most instances, there’s no hidden condition causing this, so there’s no need for treatment. Superior oblique myokymia involves minor, repetitive contraction of the superior oblique muscle, a small muscle in the eye. Very seldom, it can be caused by tumors in the brainstem or cerebellopontine angle, areas in the lower part of the brain.
Patients experiencing minor symptoms typically do not require any medical or surgical interventions. However, for those troubled by more severe symptoms, their treatment will follow the suggested course of action discussed above. It’s essential for the patient to consult with their doctor to determine the best course of treatment based on their specific symptoms and health profile.