What is Trachoma?
Trachoma is an eye disease that can have a serious and lasting impact on vision. It’s caused by a bacterium called Chlamydia trachomatis and is one of the main causes of blindness around the world. Without treatment, this bacterial infection primarily affects part of the eye called the conjunctiva. This can lead to constant cycles of inflammation and scarring on the inner part of the eyelids, and damage to the cornea, which is the clear layer at the front of the eye. These complications often result in permanent blindness. The World Health Organization recognizes trachoma among the top 20 neglected tropical diseases and it is the most common infection causing vision loss in less affluent countries.
As living conditions have improved, trachoma has significantly decreased in most North American and European countries. There have been significant reductions in the global impact of the disease due to deliberate strategies implemented over the past few decades. However, despite ongoing and rigorous interventions, trachoma continues to be common in certain societies.
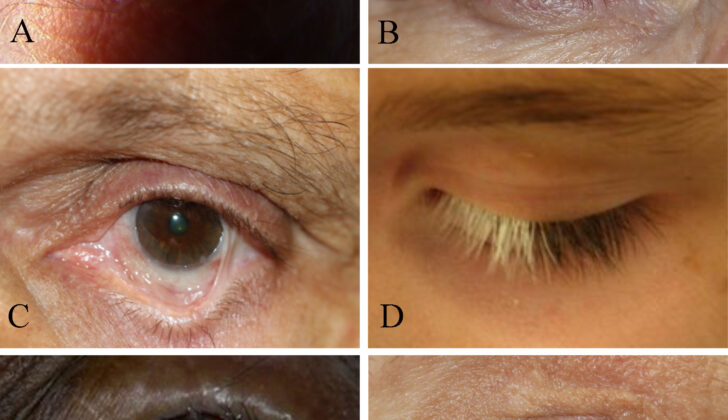
Trachoma develops in two distinct stages, each stage having unique symptoms and complications. The first stage symptoms include a persistent inflammation of the conjunctiva known as active trachoma. This inflammation is caused by multiple infections from the bacterium. The second stage of the disease is marked by periods of intense inflammation of the conjunctiva, which leads to scarring on the eyelids. This can cause the lashes to rotate and touch the eye, a condition known as “trichiasis”, and another condition where the eyelid curls inwards, known as “entropion”. These conditions that cause the lashes to scratch the cornea increase the risk of clouding and vision issues, leading to blindness in severe cases. If any of these pathological processes occur, it indicates the presence of trachoma.
It’s important to understand how trachoma spreads in order to take steps to prevent it. The disease is mainly spread through direct contact with discharges from the noses and eyes of infected people. It can also be transmitted through hand-eye contact, contact with infected objects, and by flies that are attracted to people’s eyes. Factors such as crowded living conditions, poor hygiene practices, and limited access to medical care all contribute to the spread of trachoma. Socioeconomic status, climate, and cultural customs also play a significant role in the spread of the disease. These factors contribute to how it spreads among populations and are often referred to as the “3 F’s” in scientific research:
Face-to-face contact: Close contact can quickly spread the highly infectious disease. This can occur through actions such as kissing, hugging, or sharing personal items like towels and washcloths with an infected person. During these interactions, the exchange of infected nasal and eye secretions between people can easily spread the bacteria.
Flies: Flies, especially a kind called Musca sorbens, are significant carriers of trachoma. These flies are attracted to secretions from people’s noses and eyes and act as carriers by holding the bacteria on their bodies. They then transfer the infection from one person to another, which is especially common in unsanitary conditions where flies are abundant.
Fomites: These are items or surfaces that are contaminated with the bacteria, such as infected linens, towels, or everyday utensils. Individuals can transfer the bacteria to these items, and those who later touch these contaminated items and then touch their face or eyes are at risk of getting the bacteria.
What Causes Trachoma?
Trachoma, an eye disease, is caused by a bacterium known as C trachomatis. The bacterium can spread from infected individuals to others through various ways. It can occur through direct eye-to-eye contact in close proximity, touching the eye with contaminated hands, coming into contact with items carrying the bacteria (commonly known as fomites), or even through flies that are drawn to the eyes.
Living in overcrowded areas, having poor hygiene practices, and a lack of access to clean water and sanitary facilities increase the risk of spreading trachoma. These factors create a suitable environment for the C trachomatis bacteria to thrive and continue spreading within communities. Understanding how trachoma spreads is vital in creating strategies to stop the disease, treat ongoing infections, and reduce its impact over the long term.
The C trachomatis bacterium not only causes eye infections like trachoma but can also cause sexually transmitted infections in humans. Trachoma primarily affects the part of the eye known as the conjunctiva, which is the clear, thin tissue covering the front of the eye. The bacterium’s life cycle and the human body’s immune response to it play a significant role in the development of trachoma. The bacterium enters the eye, infecting the cells of the conjunctiva, and undergoes a two-part developmental cycle. The infectious part of the bacterium attaches to and penetrates the cells. Inside, it changes into a form that multiplies within the cytoplasm of the cell, which is the substance within a cell that contains its components.
Clinical signs of trachoma include inflammation of the conjunctiva, enlargement of small areas of lymphoid tissue (follicles), and over time, scarring of the eyelids. These symptoms are caused by the inflammation resulting from the bacteria multiplying within the cells. The body’s immune response to the infection greatly influences the disease’s development and control. While a strong immune response can help clear the infection, repeated or ongoing infections can cause long-term inflammation and scarring. This, in turn, may lead to serious complications such as the eyelashes growing inward (trichiasis) and even blindness.
Risk Factors and Frequency for Trachoma
Trachoma is the third leading cause of blindness worldwide, following cataracts and glaucoma. Approximately 8 million people are blind or have serious vision loss because of this disease, with the highest rates seen in Africa, parts of the Middle East, the Indian subcontinent, Southeast Asia, and South America. Recent studies show that almost 2 million people across the world could be at risk of going blind because of trachoma, with a whopping 137 million people at risk of getting the disease. In 2023, it was identified that 116 million people lived in places where measures needed to be taken to prevent trachoma.
Even though 18 out of 62 countries where trachoma is endemic have managed to eliminate it as a public health issue, the disease is still a problem in many places. This is particularly the case in low- and middle-income nations where access to healthcare and hygiene facilities is limited. Factors like people’s socioeconomic status, where they live, and specific cultural behaviours all contribute to the spread of trachoma.
Despite efforts to eradicate trachoma globally by 2020, the disease still persists. However, there’s a ray of hope with treatment and prevention programmes striving to wipe out the disease by 2030.
Trachoma impacts women and children more than anyone else. Women are particularly vulnerable due to their exposure to dirty water and unsanitary conditions, often stemming from tasks related to childcare and household chores. Chances of getting trachoma can be up to four times higher in women than in men.
Age is another big factor. Children aged 10 or below are often the most affected. They’re likely to catch trachoma due to their limited ability to keep clean and their easy contact with infected individuals. After childhood, the prevalence of active trachoma normally decreases, but those who had untreated infections in childhood may face long-term issues, such as blindness and eyelid scarring.
Despite the fact that trachoma cases have drastically reduced worldwide, it’s still very dangerous in some places, particularly for disadvantaged groups with little access to clean water and healthcare facilities. To prevent this harmful eye disease, communities need to promote cleanliness, improve hygiene and sanitation, ensure access to clean water, provide antibiotic treatment, and control flies in places where the disease is common.
Signs and Symptoms of Trachoma
Trachoma is an eye infection that can cause symptoms like redness, itchiness, and discomfort of the eyes and eyelids. Other symptoms can include watery eyes, swollen eyelids, eye pain, and light sensitivity. It’s important to find out how long these symptoms have been occurring. When talking to a patient about their medical history, healthcare workers will ask about signs of trachoma and potential risks for getting the disease. Risk factors include travel to areas where the disease is common, such as North Africa, the Middle East, and India. If a patient is sexually active, doctors also rule out the possibility of related infections.
Detecting trachoma involves a detailed examination of the eyes and surrounding structures. The following components are part of the examination:
- Looking for tiny raised nodules resembling follicles on the inner surface of the eyelid. These can be a sign of trachoma.
- Checking the eyes and eyelids for signs of inflammation, which include redness, swelling, and discharge. The eyelids are also examined for inward bending or eyelashes scratching the eyeball, causing corneal scratches and vision problems.
- Using standard vision testing to identify any decrease in vision.
- Checking for signs of scarring on the inside of the eyelid, which can occur after prolonged inflammation from trachoma. Scarring may cause changes to the appearance of the tissue and its normal structure.
- Examining the cornea, or the clear front surface of the eye, for any signs of cloudiness, scratches, or ulcers. These can happen from persistent irritation caused by eyelashes scratching the cornea or from exposure of the cornea due to abnormalities of the eyelid.
- Feeling the local lymph nodes, particularly those near the ear, for any swelling. This could be a sign of infection from the bacteria that cause trachoma.
Getting a detailed medical history and physical examination is crucial for diagnosing trachoma. Recognizing unique signs and risk factors for the disease can guide the right tests and treatments to prevent complications and help save sight.
Active trachoma often presents as a type of conjunctivitis, often accompanied by a pus-like discharge from the eye. It can involve keratitis, which is inflammation of the cornea. The cornea may also become filled with blood vessels, leading to the development of pannus.
Cicatricial trachoma, a certain stage of trachoma, commonly shows up as star-shaped or linear scars, or larger connected scars on the inside of the eyelid in severe cases. This stage often impacts the upper part of the eyelid the most. As the follicles heal in this area, shallow indentations known as Herbert’s pits might form at the border of the cornea. Eyelashes may grow inward, rubbing against the eye, an extra row of eyelashes may form, blood vessels may grow into the cornea, or the eyelid may turn inward. These complications often come with severe clouding of the cornea. Eventually, damage of special cells and tear gland ducts leads to dry eyes.
Testing for Trachoma
Trachoma, an eye condition, is diagnosed primarily based on the patient’s personal health history and signs observed during a particular eye exam called a “slit-lamp examination”. Although some tests can help detect the bacteria causing trachoma, there is no universally accepted best course of testing.
Various lab tests can help in this process, such as:
– Giemsa staining: Here, a sample of cells from the inside of the eyelid is stained and examined under a microscope to look for the bacteria responsible for trachoma.
– Cell cultures and microscopy: This involves growing the cells in a lab and examining them under a microscope.
– Microbiological testing: There are certain tests, such as polymerase chain reaction and nucleic acid amplification tests, that check for the DNA of the bacteria in samples taken from the eye’s surface. These tests are very accurate but are generally considered too costly and complex for everyday use.
– Serological testing: This type of testing detects antibodies – which are substances our body produces to fight off foreign bodies like bacteria and viruses – against the bacteria in blood samples. These tests are primarily used for research rather than diagnosing individual patients.
After lab testing, a clinical evaluation is used to assess the severity of trachoma. The World Health Organization has devised a grading system based on the signs observed during an eye examination to categorize the severity of the infection.
Another part of the clinical evaluation is an examination for ‘trichiasis’, which is a condition where the eyelashes grow back into the eye, causing discomfort and potential damage to the cornea (the clear front surface of the eye). A simple flashlight examination can identify this issue.
Radiographic imaging (for example, scans such as optical coherence tomography or ultrasonography) can be used to examine structural changes in the eye, especially in situations where there is scarring or clouding of the cornea.
Sometimes, additional diagnostic methods are used, often involving technology. Tools like photographic record keeping, using mobile apps to track the illness’ progress, and employing artificial intelligence can be instrumental in diagnosing and monitoring trachoma.
Treatment Options for Trachoma
The World Health Organization (WHO) recommends the SAFE strategy (Surgery, Antibiotics, Facial cleanliness, and Environmental improvement) to deal with issues related to the eyes and face, including abnormal eyelash growth and eyelid problems.
Firstly, Antibiotics can help fight the infection. These should be given to the patient and all family members to prevent the spread of infection. Azithromycin, erythromycin, and doxycycline are some of the antibiotics used. Do note, some antibiotics may not be suitable for pregnant and breastfeeding women or children.
In some cases, a topical ointment containing tetracycline, a type of antibiotic, may be used. However, this is less effective than taking antibiotics orally.
Secondly, maintaining Facial cleanliness is important to prevent infections.
Thirdly, building a cleaner and healthier Environment is crucial. This includes ensuring access to clean drinking water, controlling the population of flies, and maintaining proper sanitation.
Lastly, Surgery may be required to treat certain conditions like trichiasis, a condition where the eyelashes grow inward, and entropion, where the eyelid folds inward. These surgeries can ensure complete closure of the eyelid and prevent further complications.
Trachoma, an infection of the eyes, is a common cause of blindness around the world. This blindness is often the end result of scarring in the eyelid and cornea due to trichiasis and entropion—a scenario which makes it imperative to manage these conditions effectively and promptly.
In areas where trachoma is prevalent, it is necessary to train local healthcare workers to perform simple, early intervention techniques. These techniques can help prevent scar formation on the cornea due to the scraping of inward-growing eyelashes.
Some of these techniques include the removal of eyelashes (epilation), destruction of eyelash follicles through cryotherapy, electrocautery, or laser treatment, and surgical removal of eyelash roots.
Patients suffering from trichiasis and entropion may need to undergo surgery to rectify the abnormalities of their eyelid and prevent damage to their cornea. This surgery would involve correcting the location and rotation of the eyelid, and may also incorporate lengthening procedures and eyelid margin adjustments.
What else can Trachoma be?
It can be difficult to differentiate trachoma from other eye conditions because they often share the same symptoms. It is very important to evaluate all potential health conditions thoroughly to prevent unnecessary treatments.
- Allergic conjunctivitis: This condition has many of the same symptoms as trachoma, including redness, itching, tearing, and eyelid swelling. Often resulting from exposure to allergens like dust, pollen, and pet dander, allergic conjunctivitis usually occurs in both eyes.
- Bacterial conjunctivitis: The signs of bacterial conjunctivitis and trachoma, such as eyelid crusting, discharge, and redness, can appear very similar. Bacterial conjunctivitis often occurs suddenly with symptoms resolving on their own, while trachoma is noted for recurring infections and continuous inflammation.
- Viral conjunctivitis: This condition, caused by viruses like adenovirus or herpes simplex virus, can also look like trachoma with symptoms of redness, tearing, and sensitivity to light. However, systemic symptoms like fever and feeling unwell are more commonly associated with viral conjunctivitis that can help distinguish it from trachoma.
- Dry eye syndrome: This condition also shares trachoma symptoms including redness, ocular discomfort, and feeling like something is in the eye. The main characteristic of dry eye syndrome is insufficient tear production or tear film stability, leading to dryness and discomfort.
- Pterygium and pinguecula: These benign growths on the conjunctiva can mimic trachoma and cause symptoms like redness and irritation. But these growths are usually one-sided and located around the limbus, making them different from the widespread inflammation seen in trachoma.
- Giant papillary conjunctivitis: This condition is an inflammatory disorder linked with contact lenses or ocular prostheses. It shares symptoms with trachoma like redness and itching, but usually happens in both eyes and is related to irritation of the surface of the eye.
- Atopic keratoconjunctivitis: This is a chronic inflammatory condition of the cornea and conjunctiva linked with atopic dermatitis. It can look like trachoma due to similar symptoms of redness, itching, and sensitivity to light. But unlike trachoma, this condition typically appears in both eyes and might be connected to additional systemic atopic symptoms.
Less common conditions that may resemble trachoma include chronic follicular conjunctivitis, Parinaud oculoglandular conjunctivitis, silent dacryocystitis, issues linked to contact lens use, and several causes of entropion and trichiasis.
What to expect with Trachoma
The future health of someone with trachoma, a type of eye infection, can depend on various things. These can include the stage of the disease, other health problems like trichiasis (misaligned eyelashes) and corneal opacities (cloudiness in the eyes), accessibility to healthcare, and the success of therapies and preventative measures to combat the disease. Global efforts, like the SAFE approach, to combat trachoma have seen recent improvements in this disease’s outlook.
Research has shown significant decreases in active trachoma due to these strategies. If trachoma is caught and treated early (TF and TI stages), patients usually have a good chance of overcoming the disease. Antibiotics such as azithromycin and topical tetracycline are successful in eliminating the C trachomatis infections, which reduces the chance of the disease worsening. Education about cleanliness and changes to the environment also play key roles in stopping the spread and reinfection of trachoma within communities.
For those in the advanced stages of trachoma, where scarring (TS stage) has occurred, problems could worsen if complications arise. Trichiasis and corneal opacities can lead to scratches on the cornea, ulcers, and even blindness. However, surgical techniques can considerably help these conditions and prevent blindness.
Long-term outlooks for trachoma patients can be significantly impacted by complications like cloudiness of the cornea, new blood vessel growth, and irreversible vision loss. If left untreated, corneal cloudiness and scarring from recurring infections and chronic inflammation can lead to blindness or visual impairment. In severe cases, however, some vision might be restored through certain medical and surgical procedures, such as corneal transplantation.
Global efforts to manage and stop trachoma have led to significant improvements in the disease’s future. Initiatives like the International Trachoma Initiative (ITI) and the WHO Alliance for the Global Elimination of Trachoma by 2020 have greatly reduced the prevalence of trachoma and blindness. Through mass medication campaigns, surgical outreach, and community treatments, patient results have improved and access to care has increased.
Despite these improvements, trachoma remains a major public health issue, particularly in areas with limited resources. However, advancements in diagnosis, prevention, and treatment have led to better outcomes for those affected. To eliminate trachoma globally and prevent unnecessary blindness, continued funding is necessary for trachoma control programs, research efforts, and awareness campaigns.
Possible Complications When Diagnosed with Trachoma
Trachoma, if not diagnosed or managed correctly, can lead to problems that might cause permanent blindness and impaired vision. These issues are usually due to repeated infections, ongoing inflammation and scarring associated with the disease.
Here are some key complications associated with trachoma:
- Trichiasis: This is when eyelashes grow in the wrong direction and rub on the surface of the eye. Over time, this repeated rubbing can cause corneal sores, ulcerations, and scarring. Without treatment, this can progress to cause cloudiness of the front of the eye and blindness.
- Entropion: This complication happens when the eyelid turns inward, causing eyelashes to scrape the surface of the eye. This can lead to discomfort, corneal sores, and risk of blindness if not treated. Entropion can occur because of advanced scarring and recurrent infections from trachoma.
- Distichiasis: This is when an extra row of eyelashes grow inwards towards the eye. This can cause pain, redness, and potential damage to the cornea.
- Dry eye syndrome: Trachoma can negatively impact the cornea and the conjunctiva, which could reduce tear production and eventually lead to symptoms like redness, burning, itching, and impaired vision.
- Superadded bacterial infection: Trachoma can weaken the eyes’ immune defenses, making them more prone to secondary bacterial infections. If not treated, these infections can intensify trachoma symptoms and lead to conditions like conjunctivitis, corneal ulcers, and potentially blindness.
- Corneal opacities: These occur due to prolonged inflammation and scarring of the cornea. This cloudiness of the cornea can cause reduced vision and possibly irreversible vision loss.
- Corneal neovascularization: This is the abnormal growth of blood vessels in the cornea, which can disrupt the eye’s clear view and potentially lead to impaired vision.
- Conjunctival scarring: Recurring inflammation in trachoma can lead to scarring of the conjunctiva, making the eye more prone to dryness and infections.
- Blindness: Trachoma can eventually lead to irreversible blindness if not treated or managed properly. This not only affects the individual but also has major socio-economic impact on their community.
Preventing Trachoma
If you want to avoid getting sick, it’s important to stay away from crowded places and keep yourself clean. One way to do this is by not touching your eyes too often. Washing your hands regularly and keeping your face clean can also help prevent illness. When you wash your face, make sure to use soap and water – this helps get rid of any harmful germs that might be on your skin. If you’re in a place where a lot of people get sick often, make sure to dry your face with a clean towel and don’t share things like towels or washcloths with others.
Keeping your hands clean is particularly important before you touch food and after you go to the bathroom. This is because germs can spread from your hands to your mouth and make you sick. If where you live doesn’t have good access to clean water or proper waste disposal, it’s important to address these problems to help reduce the spread of diseases. This could be as simple as making sure everyone has access to clean water, or as complex as improving the local waste disposal system.
If you live in a high-risk area, you should know the signs and symptoms of trachoma, a disease that affects the eyes and can cause redness, irritation, discharge, and blurred vision. If you’ve got these symptoms, it’s really important to see a medical professional right away. Your doctor might recommend you take antibiotics, which have been shown to effectively treat this disease. Community-wide education sessions can help everyone understand the disease, how to avoid it, and when to get treatment. This needs to be done in a way that respects local culture and responds to the specific needs of that community.
If someone in your family or community has trachoma, you should try to avoid close contact with them so you don’t get the disease yourself. You should also learn as much as you can about the disease, including how it spreads, how you can avoid it, and what happens if it’s not treated correctly.
Overall, helping everyone understand and manage trachoma can help prevent its spread and improve the health and well-being of those affected. This requires an ongoing commitment to educating people, developing healthy habits, and making important changes at the community level.